- Department of Neurosurgery, Neurosurgery Teaching Hospital, Baghdad, Iraq,
- Department of Neurosurgery, Jordan Hospital and Medical Center, Amman, Jordan,
- Department of Neurosurgery, University of Baghdad, College of Medicine, Baghdad, Iraq,
- Department of Neurosurgery, University of Louisville, Louisville, Kentucky, United States
- Department of Neurosurgery, University of Wisconsin, Madison, Wisconsin, United States
- Department of Neurosurgery, University of Cincinnati, Cincinnati, United States.
Correspondence Address:
Samer S. Hoz, Department of Neurosurgery, University of Cincinnati, Cincinnati, United States.
DOI:10.25259/SNI_1023_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mustafa Ismail1, Osman Elamin2, Teeba A. Al-Ageely3, Hagar A. Algburi3, Mayur Sharma4, Zaid Aljuboori5, Samer S. Hoz6, Norberto Andaluz6. Rectus gyrus hematoma: An overview. 02-Dec-2022;13:558
How to cite this URL: Mustafa Ismail1, Osman Elamin2, Teeba A. Al-Ageely3, Hagar A. Algburi3, Mayur Sharma4, Zaid Aljuboori5, Samer S. Hoz6, Norberto Andaluz6. Rectus gyrus hematoma: An overview. 02-Dec-2022;13:558. Available from: https://surgicalneurologyint.com/surgicalint-articles/12042/
Abstract
Background: Rectus gyrus hematoma (RGH) is a localized intracerebral hemorrhage involving the most medial part of the orbital surface of the frontal lobe. It can be an imaging finding in the setting of a ruptured anterior communicating artery aneurysm; however, other differentials are rarely reported in the literature. In this paper, we opt to present for the 1st time an overview of RGH regarding its history, anatomical correlation, and related neuroimaging with particular emphasis on the potential differential diagnosis for underlying pathologies.
Methods: A literature review was conducted in PubMed, Medline, and Google scholar databases to review the existing literature highlighting the history, pertinent anatomy, and clinical characteristics of RGH.
Results: The literature review yielded papers targeting the RGH neither as a radiological sign nor as a surgical correlate to the cerebrovascular lesion. We used the available indirectly related articles to formulate an overview to serve the aim of this paper and to highlight the potential value of studying the RGH.
Conclusion: The RGH may represent an overlooked radiological finding that has potential significance through its relation to a set of vascular lesions affecting the brain. Further studies into the topic are needed to expand the utility of this sign.
Keywords: Aneurysm, Brain anatomy, Gyrus rectus, Intracranial hemorrhage, Rectus gyrus
BACKGROUND
Rectus gyrus hematoma (RGH) is a localized intracerebral hemorrhage in the medial aspect of the sub-frontal area. The term jet hematoma or flame hemorrhage also can be used to describe such intracerebral hematoma. RGH may occur due to a ruptured intracranial aneurysm adjacent to the frontal lobe. A ruptured anterior communication artery (Acom) aneurysm is a common encountered etiology of RGH as it is closely related to the sub-frontal area. However, other associated conditions may be considered in the differential diagnosis, such as arteriovenous malformation (AVM) and cavernous malformation. For these multiple pathologies associated with RGH, one of the underlying mechanisms for developing hematoma within the rectus gyrus (RG) is the pressure difference between the area in and outside the brain parenchyma.[
HISTORY
The history of precisely identifying intracerebral hematomas begins with computed tomography (CT) scans in the 1970 s. Pasqualin et al. 1986 argued that before the clinical use of CT scan in 1976, angiography was not accurate enough to detect such lesion. Moreover, even the cases that underwent autopsy before 1976 could not recognize the hemorrhage intracranially as it is small and may fade post-mortem quickly.[
PERTINENT ANATOMY AND FUNCTION OF RG
The RG, also called the straight gyrus, occupies the inferior aspect of the frontal lobe in the medial margin. Boundaries of the RG, medially the interhemispheric fissure, and wrap around the inferomedial surface of the frontal lobe. The rostral gyrus is located superiorly, separated by the inferior rostral sulcus — the olfactory sulcus significant landmark separating RG laterally from the medial orbital gyrus.[
The function of the gyrus rectus remains unclear; consequently, many authors call it non-functional gyrus because there are no specific functions related to it.[
DIFFERENTIAL DIAGNOSIS
Ruptured intracranial aneurysms
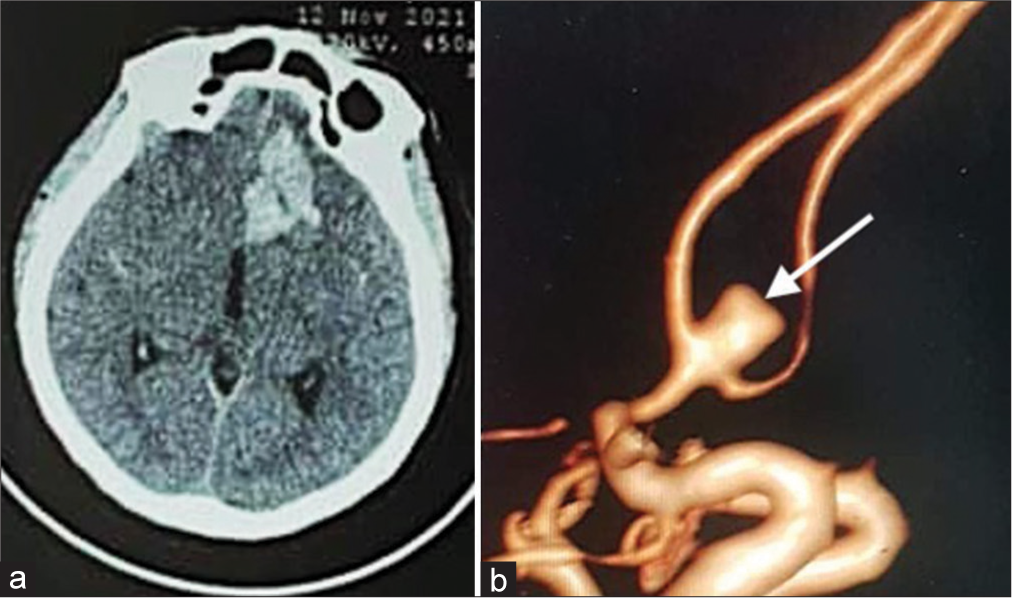
Multiple pathologies may be associated with RGH; however, based on our experience, a ruptured Acom aneurysm is located at the top of the differential diagnosis, primarily when directed superiorly or anteriorly or combined superior-anterior projection. Moreover, RGH due to rupture Acom aneurysm is usually associated with intraventricular hemorrhage in the lateral ventricle frontal horn [
Figure 1:
(a) Case 1: A 43-year-old female presented with a sudden onset headache. Computed tomography scan of the head (Axial view) showing intracerebral hemorrhage in the left the frontobasal area (Rectus gyrus). (b) 3D constructed angiography demonstrating a superior-anteriorly directed AcoA aneurysm (white arrow).
Based on the literature, other rupture aneurysms near RG have been reported to be associated with RGH, including a left distal internal carotid aneurysm in which imaging showed restricted left RG hematoma with SAH.[
Non-aneurysmal pathologies
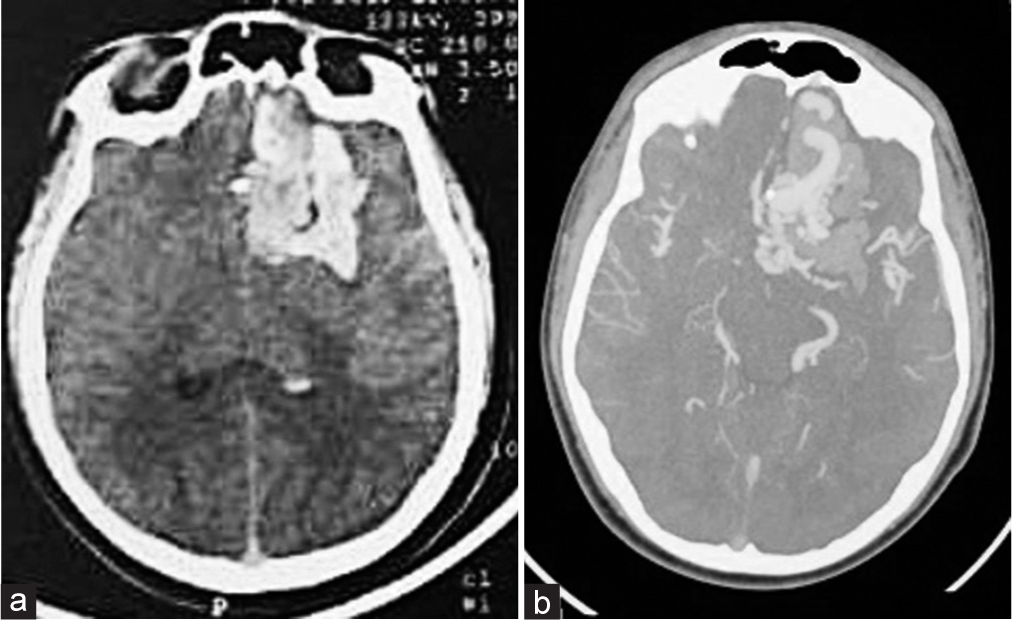
The literature did not name the RGH as a finding of any non-aneurysmal lesions. However, one can argue that hemorrhage in the inferomedial aspect of the frontal lobe from any cause can be included in the spectrum of RGH. Based on our experience, non-aneurysmal associations with RGH can include frontal AVM and cavernomas [
Figure 2:
(a) Case 2: A 14-year-old male presented with loss of consciousness. Computed tomography (CT) scan of the head (Axial view) shows the left intracerebral haemorrhage in the frontal lobe within the rectus gyrus and there are no signs of subarachnoid hemorrhage. (b) CT angiography scan of the head (Axial view) illustrates a tuft of vessels (Arteriovenous malformation) in the left rectus gyrus.
SYMPTOMS AND SIGNS
RGH can have variable presentations, mainly dependent on the underlying associated pathology. The recognition of direct and precise symptoms from the RG lesion is feasible only after the functional significance of this anatomical structure is well addressed, a topic that can be addressed in the future with more dedicated studies tackling this issue.
In general, the RGH can have a presentation related to the underlying pathology. In patients with ruptured Acom aneurysms, the symptoms are usually related to SAH, such as headache, vomiting, and other symptoms of SAH.[
PROGNOSIS
The isolated clinical prognosis of RGH cannot be specified based on the current available evidence. However, the general overview based the available reports, there is a noticeable good prognosis trend from all the described etiologies underlying RGH.
Limitations and future direction
The available literature did not study the GRH sign as an independent factor to assess its significance and its potential impact on the outcome. A large and multicenter study is required to evaluate this sign and its clinical and surgical potential correlation.
In summary, this article highlights an overview of RGH, beginning with its first recognition after CT scans became widely available. Further, the relevant anatomy and function of the RG were discussed. A differential diagnosis of this sign is provided based on whether it is an aneurysmal cause or others. In this study, we are the first to pinpoint the potential value of this sign and list the available possible differential diagnoses in addition to the already known that the RGH is a valuable radiological clue in the setting of a ruptured Acom aneurysm.
CONCLUSION
The RGH may represent an overlooked radiological finding that has potential significance through its relation to a set of vascular lesions affecting the brain. Further studies into the topic are needed to expand the utility of this sign.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abbed KM, Ogilvy CS. Intracerebral hematoma from aneurysm rupture. Neurosurg Focus. 2003. 15: E4
2. Budohoski KP, Tajsic T, Barone DG, Guilfoyle M, Santarius T, Kirollos RW. Surgical resection of an arteriovenous malformation of the orbital surface of the frontal lobe with olfactory tract preservation: 2-dimensional operative video. World Neurosurg. 2022. 158: 156-7
3. Cummings JL. Frontal-subcortical circuits and human behaviour. Psychosom Res. 1998. 44: 627-8
4. Da Costa LB, Valiante T, Terbrugge K, Tymianski M. Anterior ethmoidal artery aneurysm and intracerebral hemorrhage. Am J Neuroradiol. 2006. 27: 1672-4
5. Ellington E, Margolis G. Block of arachnoid villus by subarachnoid hemorrhage. J Neurosurg. 1969. 30: 651-7
6. Hornak J, Bramham J, Rolls ET, Morris RG, O’Doherty J, Bullock PR. Changes in emotion after circumscribed surgical lesions of the orbitofrontal and cingulate cortices. Brain. 2003. 126: 1691-712
7. Joo MS, Park DS, Moon CT, Chun YI, Song SW, Roh HG. Relationship between gyrus rectus resection and cognitive impairment after surgery for ruptured anterior communicating artery aneurysms. J Cerebrovasc Endovasc Neurosurg. 2016. 18: 223-8
8. Kareem ZM, Arnaout MM, Al-Baidar RA, Al-Sharshahi ZF, Hoz SS. Gyrus Rectus cavernoma masquerading as an intracranial aneurysm: A case report and review of literature. Neurosurg Cases Rev. 2021. 4: 5
9. Karttunen AI, Jartti PH, Ukkola VA, Sajanti J, Haapea M. Value of the quantity and distribution of subarachnoid haemorrhage on CT in the localization of a ruptured cerebral aneurysm. Acta Neurochir (Wien). 2003. 145: 655-61
10. Knutson KM, Dal Monte O, Schintu S, Wassermann EM, Raymont V, Grafman J. Areas of brain damage underlying increased reports of behavioral disinhibition. J Neuropsychiatry Clin Neurosci. 2015. 27: 193-8
11. Pasqualin A, Bazzan A, Cavazzani P, Scienza R, Licata C, Da Pian R. Intracranial hematomas following aneurysmal rupture: Experience with 309 cases. Surg Neurol. 1986. 25: 6-17
12. Patankar AP, Vaja M. Lower limb weakness with gyrus rectus hematoma: An unusual presentation of paraclinoid aneurysm; A case report with review of literature. Egypt J Neurol Psychiatry Neurosurg. 2019. 55: 67
13. Ramos A, Chaddad-Neto F, Joaquim AF, Campos-Filho JM, Mattos JP, Ribas GC. The microsurgical anatomy of the gyrus rectus area and its neurosurgical implications. Arq Neuropsiquiatr. 2009. 67: 90-5
14. Winckler C, Magezi D, Croquelois A. Restricted left gyrus rectus hemorrhage with unusual frontal syndrome presentation. Eur Neurol. 2011. 65: 129-31