- Department of Orthopedic Surgery, Nagoya University Graduate School of Medicine, Nagoya, Aichi, Japan.
Correspondence Address:
Kei Ando, Department of Orthopedic Surgery, Nagoya University Graduate School of Medicine, Nagoya, Aichi, Japan.
DOI:10.25259/SNI_1187_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Naoki Segi, Kei Ando, Hiroaki Nakashima, Masaaki Machino, Sadayuki Ito, Hiroyuki Koshimizu, Hiroyuki Tomita, Shiro Imagama. Recurrent ossification of the posterior longitudinal ligament in the upper thoracic region 10 years after initial decompression. 12-Jan-2022;13:17
How to cite this URL: Naoki Segi, Kei Ando, Hiroaki Nakashima, Masaaki Machino, Sadayuki Ito, Hiroyuki Koshimizu, Hiroyuki Tomita, Shiro Imagama. Recurrent ossification of the posterior longitudinal ligament in the upper thoracic region 10 years after initial decompression. 12-Jan-2022;13:17. Available from: https://surgicalneurologyint.com/surgicalint-articles/11335/
Abstract
Background: Posterior decompression surgery consisting of laminoplasty is generally considered be the treatment of choice for upper thoracic OPLL. Here, we describe a patient who, 10 years following a C3–T4 level laminectomy, developed recurrent OPLL at the T2–3 level with kyphosis requiring a posterior fusion.
Case Description: A 64-year-old male with CT documented OPLL at the C3–4, C6–7, and T1–4 levels, originally underwent a cervicothoracic laminectomy with good results. However, 10 years later, when T2–3 OPLL recurred along with kyphosis, he warranted an additional posterior fusion.
Conclusion: Due to the long-term risks of developing kyphotic deformity/instability, more patients undergoing initial decompressive surgery alone for upper thoracic OPLL should be considered for primary fusions.
Keywords: Indirect decompression, Ossification of the posterior longitudinal ligament, Posterior decompression, Posterior fusion with dekyphosis, Upper thoracic ossification of the posterior longitudinal ligament
INTRODUCTION
Ossification of the posterior longitudinal ligament (OPLL) occurs in approximately 1–5% of patients and may contribute to severe myelopathy.[
CASE REPORT
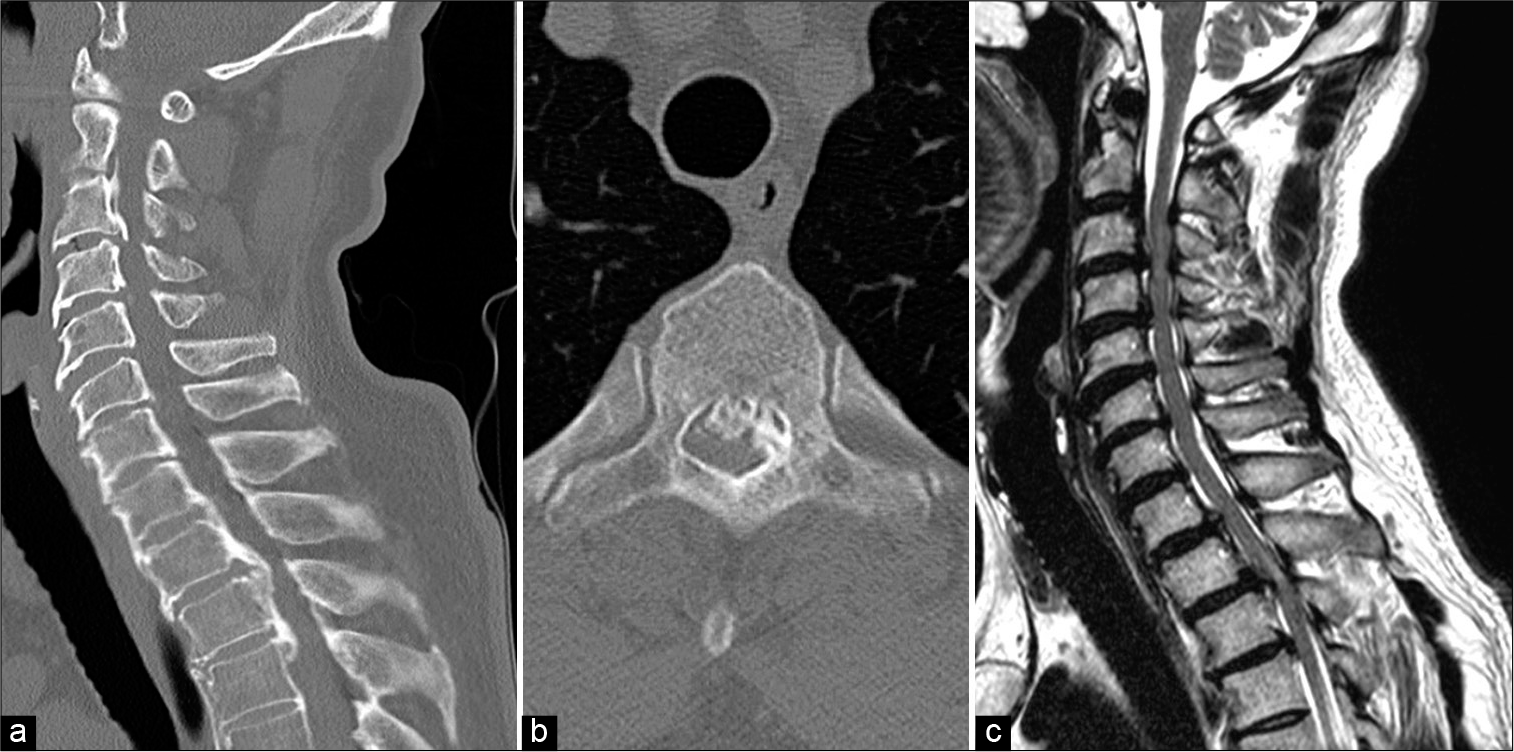
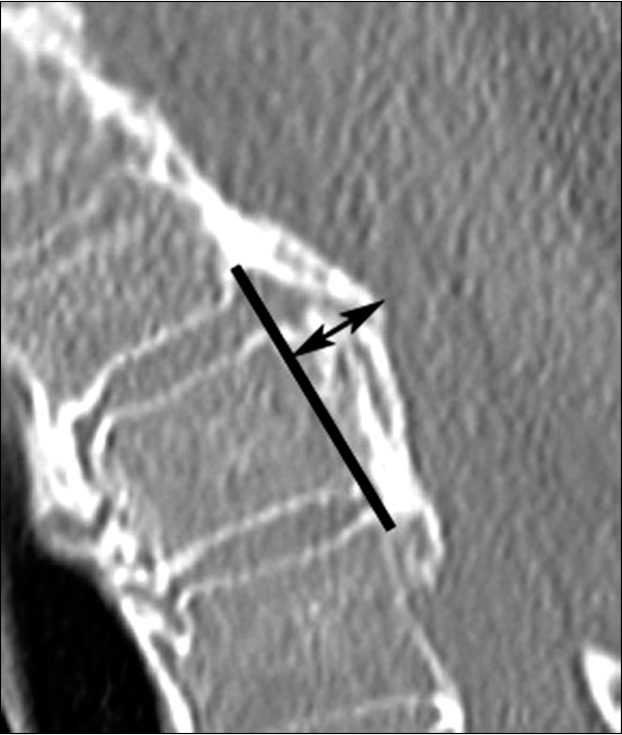
A 64-year-old male presented with a progressive quadriparesis (i.e., JOA score 11)/myelopathy due to cervicothoracic OPLL. The MR and CT studies showed spinal canal stenosis with cord compression at the C3–4/T2–3 levels, and OPLL at the C3–4, C6–7, and T1–4 levels. The occupancy ratio for OPLL of 51.2% was maximal at the T2–3 level [
Figure 1:
Images before the initial surgery. (a) CT sagittal image showed OPLL. (b) Ossification lesion at the T2–3 level. (c) MRI showed hyperintense changes of the spinal cord at C3–4 and T2–3 levels. CT: Computed tomography, MRI: Magnetic resonance imaging, OPLL: Ossification of the posterior longitudinal ligament.
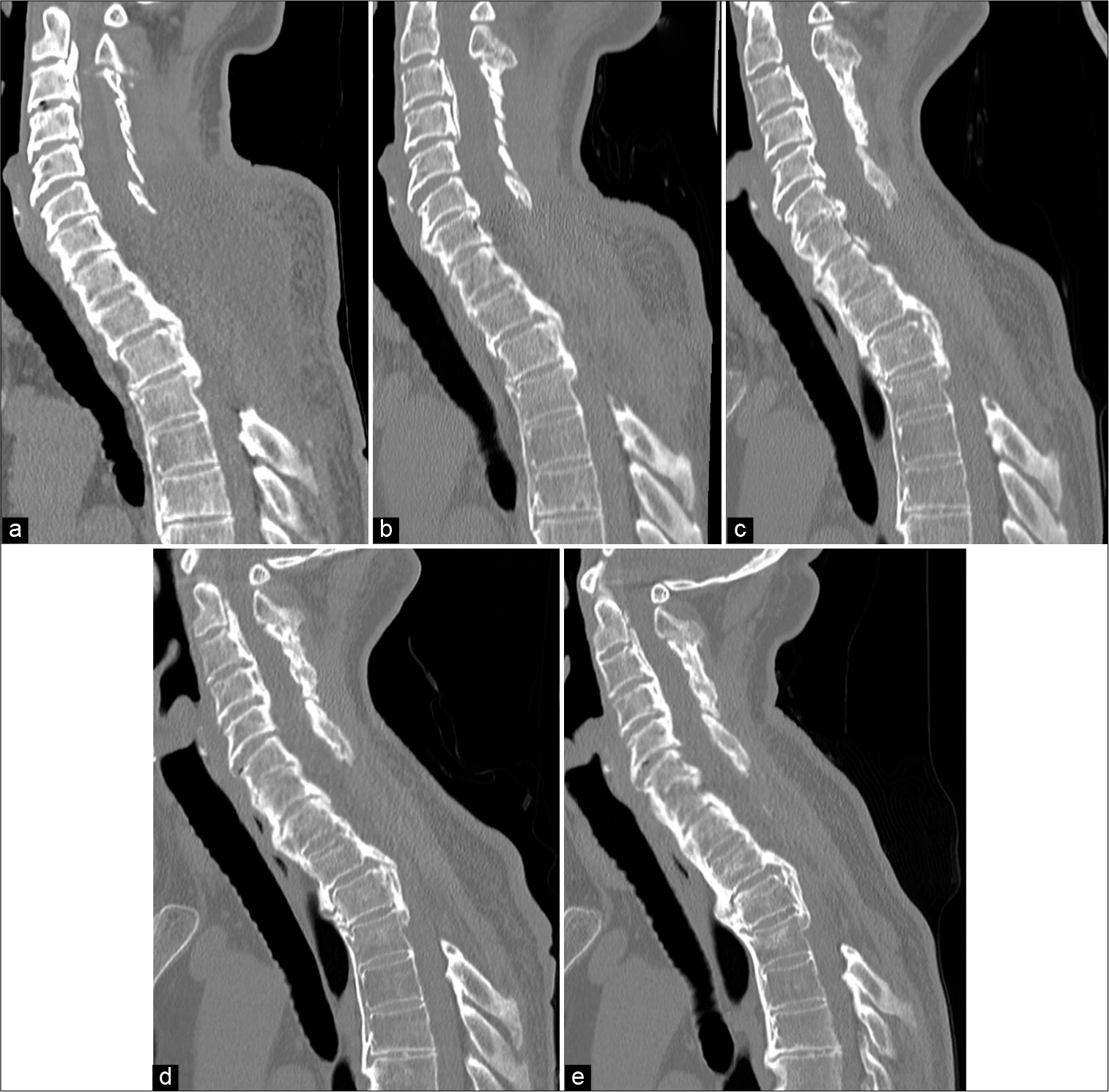
Figure 2:
Change in CT sagittal image. CT sagittal images (a) after initial surgery and at (b) 2 years, (c) 5 years, (d) 7 years, and (e) 9 years. T1–4 kyphosis was 18.3°, 18.1°, 18.4°, 23.2°, and 28.7°, respectively, and OPLL thickness was 8.7 mm, 8.6 mm, 8.8 mm, 9.4 mm, and 11.2 mm, respectively. CT: Computed tomography, OPLL: Ossification of the posterior longitudinal ligament.
10-year follow-up revealing T2–T3 kyphosis warranted posterior fusion
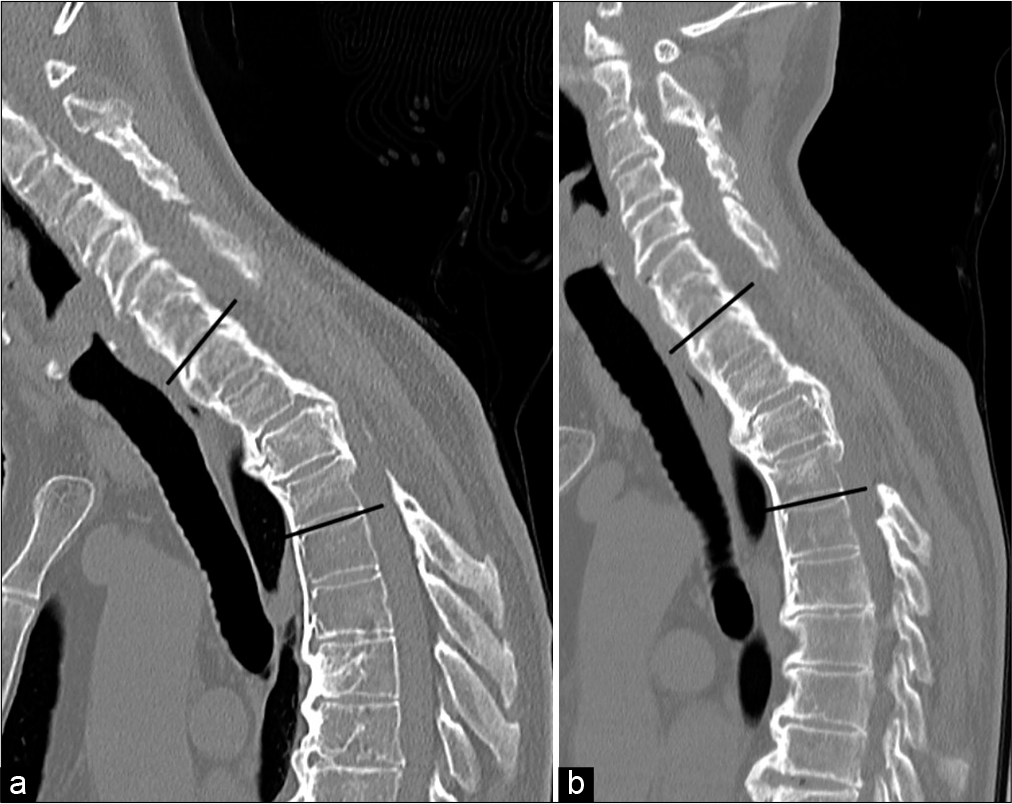
Ten years later ate age 74, the patient presented with a recurrent paraparesis/myelopathy (i.e., JOA score 14). attributed to MR/CT studies documenting maximal T2–3 cord compression from OPLL/angulation (cord pathology best seen on the MR) [
Figure 4:
Dynamic CT sagittal image before revision surgery. CT sagittal images of forward and backward bending at the time of symptom recurrence. At the neutral position, the T1–4 kyphosis angle was 29.5° and OPLL thickness was 11.6 mm. Mobility was noted at the upper thoracic spine, which appeared to be fused. Dynamic T1–4 kyphosis angles were (a) 33.2° in forward bending and (b) 22.7° in backward bending. CT: Computed tomography, OPLL: Ossification of the posterior longitudinal ligament.
DISCUSSION
Epidemiologically
OPLL most commonly involves the T1 level in males and is frequently associated with cervical OPLL.[
Fusion for upper thoracic OPLL
Instrumented upper thoracic fusions for OPLL are 82.8–97.7% effective in achieving stabilization/avoidance of OPLL progression.[
CONCLUSION
Here, we presented a 64-year-old myelopathic male who underwent an initial a double-door laminoplasty from C3–7 and laminectomy between T1–4 for OPLL. Ten years later, with recurrent myelopathy and increased T2–3 motion with kyphosis/OPLL, he successfully underwent a C6–T5 instrumented fusion.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
This work was supported by JSPS KAKENHI Grant Number JP 18K09025 and The General Insurance Association of Japan.
Conflicts of interest
There are no conflicts of interest.
References
1. Ando K, Kobayashi K, Machino M, Ota K, Tanaka S, Morozumi M. Connection of discontinuous segments in early functional recovery from thoracic ossification of the posterior longitudinal ligament treated with posterior instrumented surgery. J Neurosurg Spine. 2019. 32: 200-6
2. Fujimori T, Okawa A, Matsumoto M, Iwasaki M, Kawaguchi Y.editors. OPLL: Disease entity, prevalence, literature research, and growth. OPLL Ossification of the Posterior Longitudinal Ligament. Singapore: Springer; 2020. p. 13-21
3. Fujiyoshi T, Yamazaki M, Kawabe J, Endo T, Furuya T, Koda M. A new concept for making decisions regarding the surgical approach for cervical ossification of the posterior longitudinal ligament: The K-line. Spine (Phila Pa 1976). 2008. 33: E990
4. Hirabayashi S, Kitagawa T, Yamamoto I, Yamada K, Kawano H. Surgical treatment for ossification of the posterior longitudinal ligament (OPLL) at the thoracic spine: Usefulness of the posterior approach. Spine Surg Relat Res. 2018. 2: 169-76
5. Hirai T, Yoshii T, Nagoshi N, Takeuchi K, Mori K, Ushio S. Distribution of ossified spinal lesions in patients with severe ossification of the posterior longitudinal ligament and prediction of ossification at each segment based on the cervical OP index classification: A multicenter study (JOSL CT study). BMC Musculoskelet Disord. 2018. 19: 107
6. Koda M, Furuya T, Okawa A, Aramomi M, Inada T, Kamiya K. Bone union and remodelling of the non-ossified segment in thoracic ossification of the posterior longitudinal ligament after posterior decompression and fusion surgery. Eur Spine J. 2015. 24: 2555-9
7. Matsumoto M, Chiba K, Toyama Y, Takeshita K, Seichi A, Nakamura K. Surgical results and related factors for ossification of posterior longitudinal ligament of the thoracic spine: A multi-institutional retrospective study. Spine (Phila Pa 1976). 2008. 33: 1034-41
8. Matsuyama Y, Sakai Y, Katayama Y, Imagama S, Ito Z, Wakao N. Indirect posterior decompression with corrective fusion for ossification of the posterior longitudinal ligament of the thoracic spine: Is it possible to predict the surgical results?. Eur Spine J. 2009. 18: 943-8