- Department of Orthopaedics, Seth G.S. Medical College and K.E.M. Hospital, Mumbai, Maharashtra, India.
DOI:10.25259/SNI_34_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Rudra Mangesh Prabhu, Tushar N. Rathod. Recurrent symptomatic vertebral hemangioma in pregnancy managed with decompression and vertebroplasty. 08-Apr-2021;12:150
How to cite this URL: Rudra Mangesh Prabhu, Tushar N. Rathod. Recurrent symptomatic vertebral hemangioma in pregnancy managed with decompression and vertebroplasty. 08-Apr-2021;12:150. Available from: https://surgicalneurologyint.com/surgicalint-articles/10693/
Abstract
Background: Vertebral hemangioma is a benign vascular tumor of the spine that occurs in the endothelial lining of blood vessels. The majority of these lesions are detected incidentally on routine magnetic resonance imaging scans. Rarely, lesions can increase in size and result in neurological deterioration.
Case Description: A 19-year-old post-partum female, presented with paraplegia due to a recurrent vertebral hemangioma with exophytic extension into the epidural space resulting in spinal cord compression. Early decompressive surgery facilitated adequate early recovery of neurological function.
Conclusion: Exophytic vertebral hemangiomas that have extended into the spinal canal resulting in cord compression require urgent surgical decompression.
Keywords: Epidural, Post-partum, Tumor, Vascular, Vertebral hemangioma
INTRODUCTION
Vertebral hemangiomas (VH) are the most common benign tumors of the spine. Based on a large autopsy series, and a large review of plain spine films, these lesions occur in about 10–12% of the general population. Middle aged females are most commonly affected.[
CASE REPORT
First surgery
A 19-year-old, 1-month postpartum female presented with a progressive paraparesis of two months’ duration. She had originally presented at the age of 13 years with paraparesis and back pain. The thoracic MR scan showed a T4 hemangioma that extended into the epidural space from T3 to T5 causing cord compression; a second hemangioma was localized to the T9 level without intraspinal extension. The patient was managed with arterial embolization of feeders from the thyrocervical trunk, and she neurologically recovered.
Secondary surgery
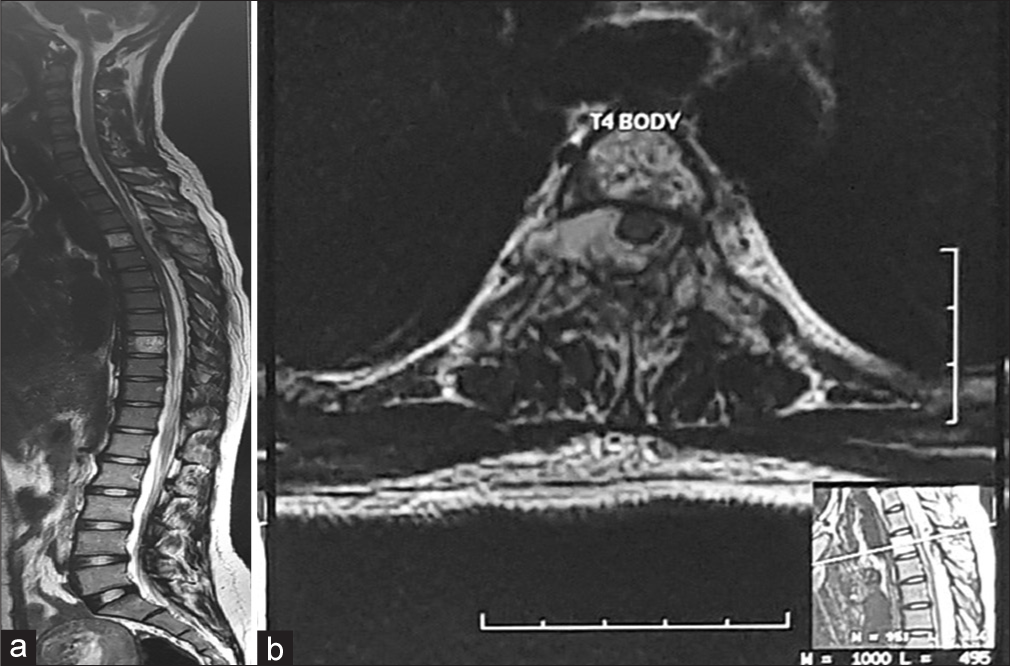
The patient had a symptom-free course for 6 years at which point she newly developed paraplegia (Frankel Grade A: Complete) in the eighth month of pregnancy. The thoracic magnetic resonance imaging (MRI) now showed a recurrent VH with exophytic extension, and cord compression at the T3-T5 levels [
Figure 1:
(a) T2-weighted MRI scan(sagittal cut) of the whole spine (b) T2-weighted MRI scan at the level of T4 (axial cut). (a) A well-defined extradural soft tissue mass is seen extending from the inferior end-plate of T3 to the inferior end-plate of T5. Hyperintensities noted at T4 and T9. (b) Lesion seen at the level of T4 with an epidural component surrounding the spinal cord and causing displacement of the cord from the midline.
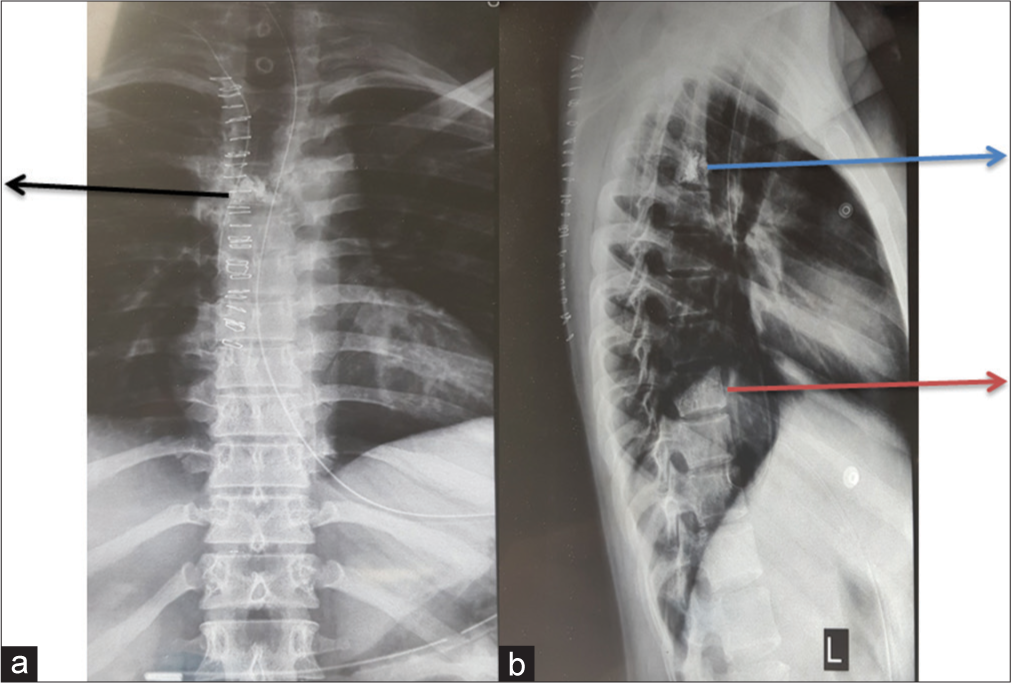
Figure 3:
Post-operative anteroposterior and lateral radiograph of the spine. (a)Anteroposterior radiograph demonstrates the radio-opaque cement injected into the T4 vertebral body (black arrow). (b) Cement can be seen in T4 on lateral view. A striated pattern can be demonstrated in the T9 vertebral body (red arrow), suggestive of a vertebral body hemangioma
DISCUSSION
Clinical presentation and etiology of neurological findings
Vertebral hemangioma is a malformed vascular lesion which is symptomatic in only 0.9–1.2% of cases. They may present with pain (54%) or neurological symptoms (45%).[
Radiographic findings
Plain radiographs demonstrate a vertically striated pattern. On MRI scan, they are hyper-intense to mottled/ starburst on T1 and T2 weighted images, or hyperintense on the T2-weighted study as was seen in our case.
Computed tomography (CT) findings of VH and guided biopsy
On axial CT scan cuts, VH will show a “polka-dotted” or “salt and pepper” appearance due to the thickened vertebral trabeculae. A percutaneous CT-guided biopsy should be performed in cases where there is a suspected malignant lesion.
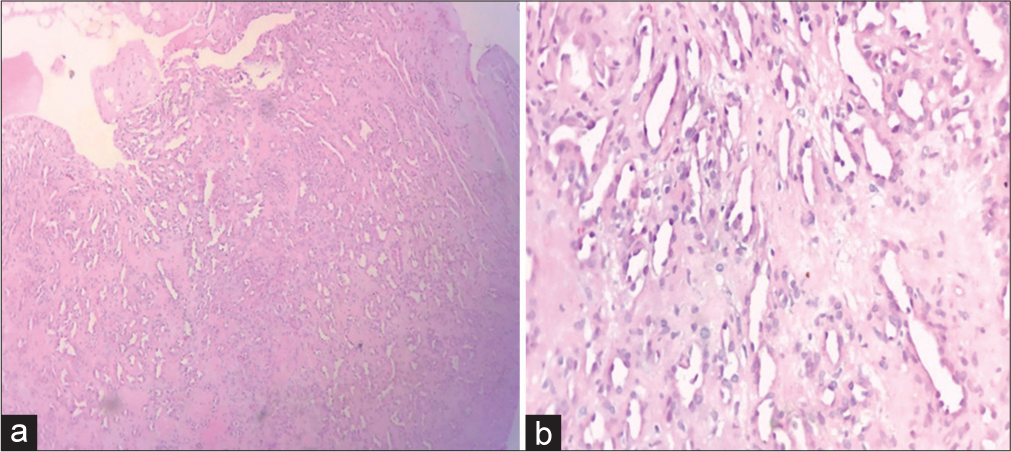
Pathology
There are three histological variants of VH: capillary, cavernous, and mixed type; the cavernous type is the most common. The lesion in this case was a capillary hemangioma [
Surgery for symptomatic VH
The main indication for surgical decompression is rapid and progressive neurologic deterioration. Noninvasive management with angioembolization or radiotherapy can be attempted when the lesion is just localized to the vertebral body in an asymptomatic patient. In our case, the patient had a vertebral lesion with exophytic extension into the spinal canal that was first managed non-invasively with embolization procedure, but ultimately recurred with significant intraspinal extension.
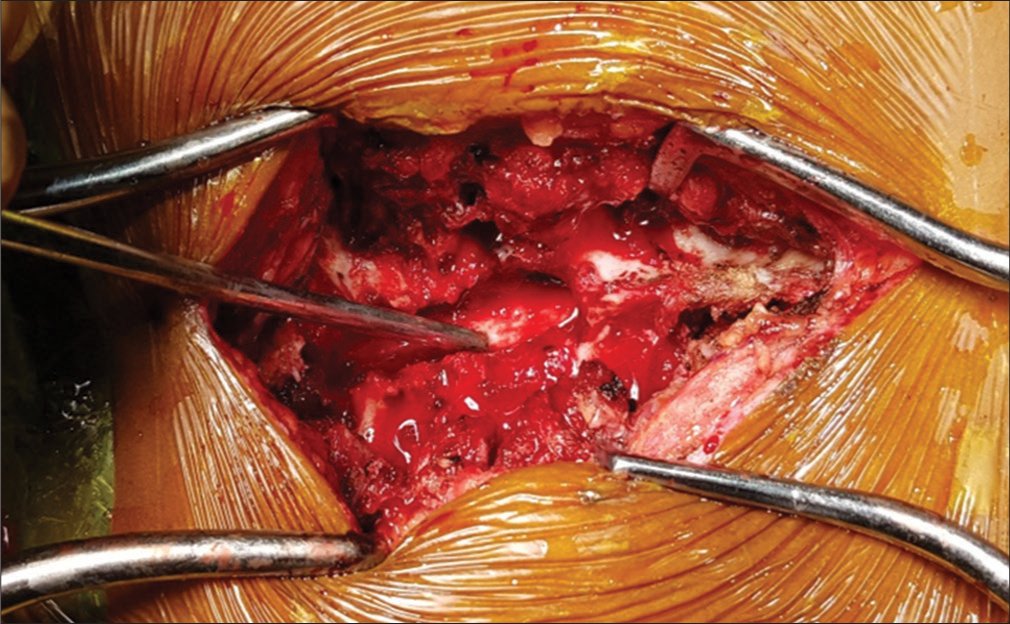
Embolization and radiotherapy were not appropriate options in our patient as the epidural tumor resulted in cord compression and a significant neurological deficit. Here, the patient underwent an emergent decompressive laminectomy from T3-T5 with T4 vertebroplasty.
Treatment of symptomatic VH with pregnancy
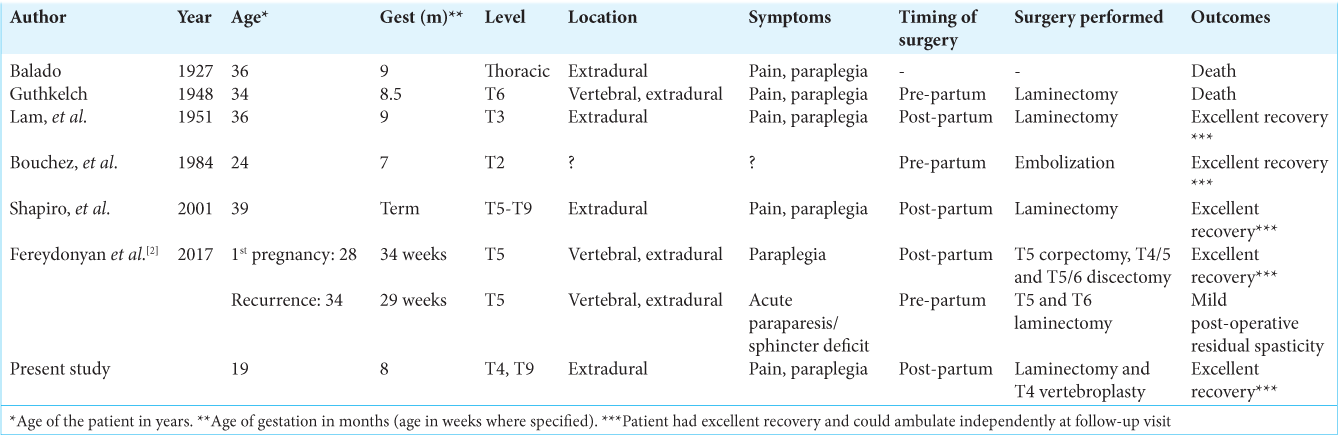
There are few reports in the literature reporting symptomatic VH in pregnancy [
CONCLUSION
The management of recurrent symptomatic, exophytic VH that extends into the spinal canal resulting in renewed cord compression should consist of laminectomy and vertebroplasty.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Chi JH, Manley GT, Chou D. Pregnancy-related vertebral hemangioma. Case report, review of the literature, and management algorithm. Neurosurg Focus. 2005. 19: E7
2. Fereydonyan N, Taheri M, Kazemi F. Recurrent symptomatic vertebral hemangioma during two consecutive pregnancies: Case report and review of the literature. Surg Neurol Int. 2017. 8: 105
3. Gupta M, Nayak R, Singh H, Khwaja G, Chowdhury D. Pregnancy related symptomatic vertebral hemangioma. Ann Indian Acad Neurol. 2014. 17: 120-2
4. Murugan L, Samson RS, Chandy MJ. Management of symptomatic vertebral hemangiomas: Review of 13 patients. Neurol India. 2002. 50: 300-5
5. Nair AP, Kumar R, Srivastav AK, Sahu RN, Kumar B. Outcome of dorsolumbar vertebral hemangiomas presenting with neuraxial compression. Indian J Orthop. 2012. 46: 536-41
6. Santagada DA, Perna A, Meluzio MC, Ciolli G, Proietti L, Tamburrelli FC. Symptomatic vertebral hemangioma during pregnancy period: A case series and systematic literature review. Orthop Rev (Pavia). 2020. 12: 8685