- Department of Neurosurgery, Faculty of Medical Sciences, University of Fukui, Eiheiji, Fukui,
- Department of Neurosurgery, Dokkyo University School of Medicine, Mibu, Japan
Correspondence Address:
Satoshi Kawajiri, Department of Neurosurgery, Faculty of Medical Sciences, University of Fukui, Eiheiji, Fukui, Japan
DOI:10.25259/SNI_1150_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Satoshi Kawajiri1, Ryu Kurokawa2, Tetsuro Shingo2. Redundant nerve root syndrome mimicking an intradural spinal cord tumor: A case report. 20-Jan-2023;14:19
How to cite this URL: Satoshi Kawajiri1, Ryu Kurokawa2, Tetsuro Shingo2. Redundant nerve root syndrome mimicking an intradural spinal cord tumor: A case report. 20-Jan-2023;14:19. Available from: https://surgicalneurologyint.com/surgicalint-articles/12112/
Abstract
Background: The redundant nerve root (RNR) syndrome is a pathological condition in which the cauda equina develops into a severely flexed/tortuous spiral mass above a level of severe lumbar stenosis.
Case Description: A 70-year-old male presented with bilateral neurogenic claudication attributed to a MRI-documented intradural extramedullary lesion at the L1 level with severe adjacent level/inferior L2/3 stenosis. At surgery, intradural exploration at L1 revealed an edematous cauda equina consistent with the diagnosis of the RNR syndrome.
Conclusion: The RNR syndrome should be included among the differential diagnostic considerations when non-enhancing lesions are encountered above levels of marked lumbar stenosis.
Keywords: Differential diagnosis, Extramedullary spinal cord tumor, Lumbar canal stenosis, Redundant nerve root syndrome
INTRODUCTION
Redundant nerve root (RNR) is a pathological condition in which the cauda equina presents as a mass lesion (i.e., flexed/tortuous with a spiral deformity) best seen on T2 MR studies above the level of severe lumbar spinal canal stenosis (LCS). It was first described by Verbiest in 1954, and named the “redundant nerve root” syndrome by Cressman and Pawl in 1968.[
CASE REPORT
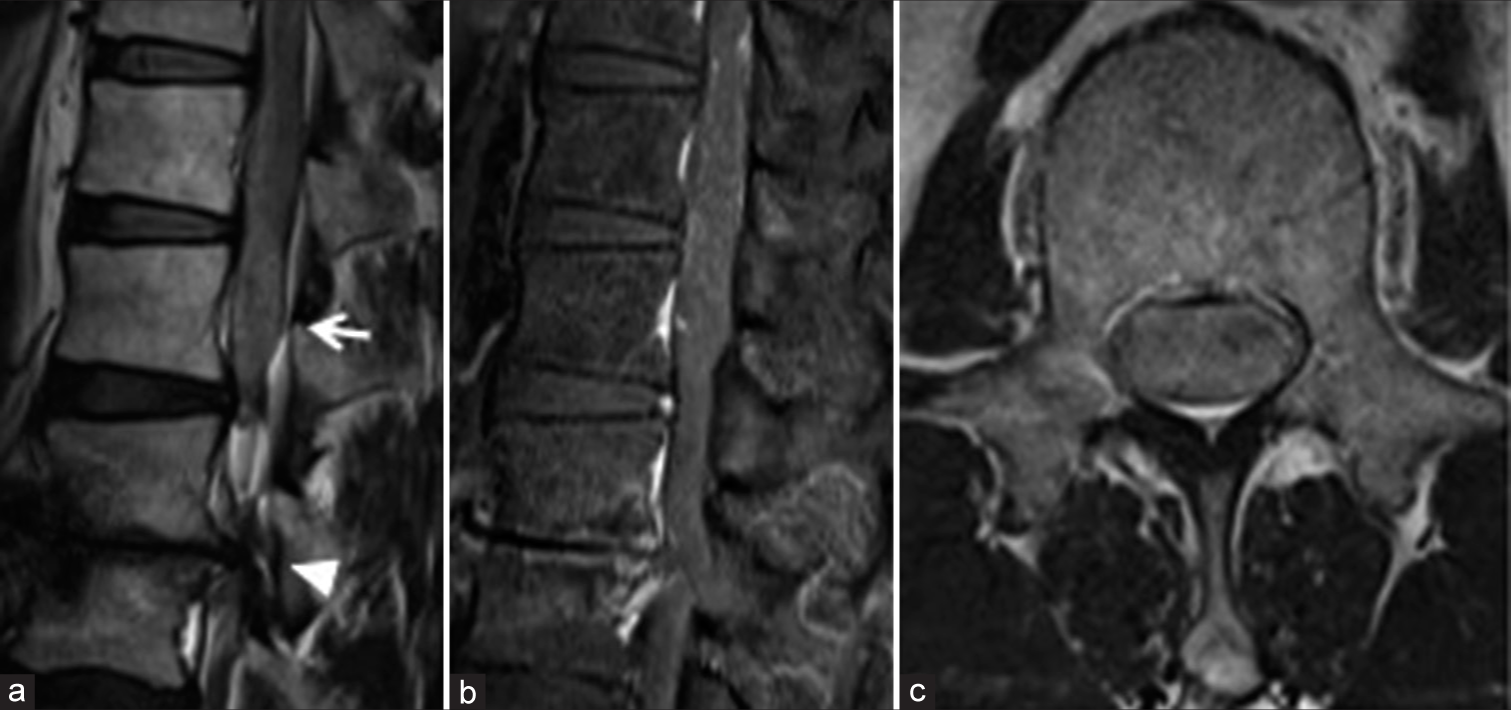
A 70-year-old male presented with 4 months of neurogenic claudication, ataxia of gait, and dysuria. His examination revealed left iliopsoas weakness and bilateral anterior thigh pain in the L3 distribution. The T2- MR showed severe stenosis at the L2/3 level due to degenerative changes along with a cephalad L1 hyperintense mass that did not enhance with contrast [
Surgery
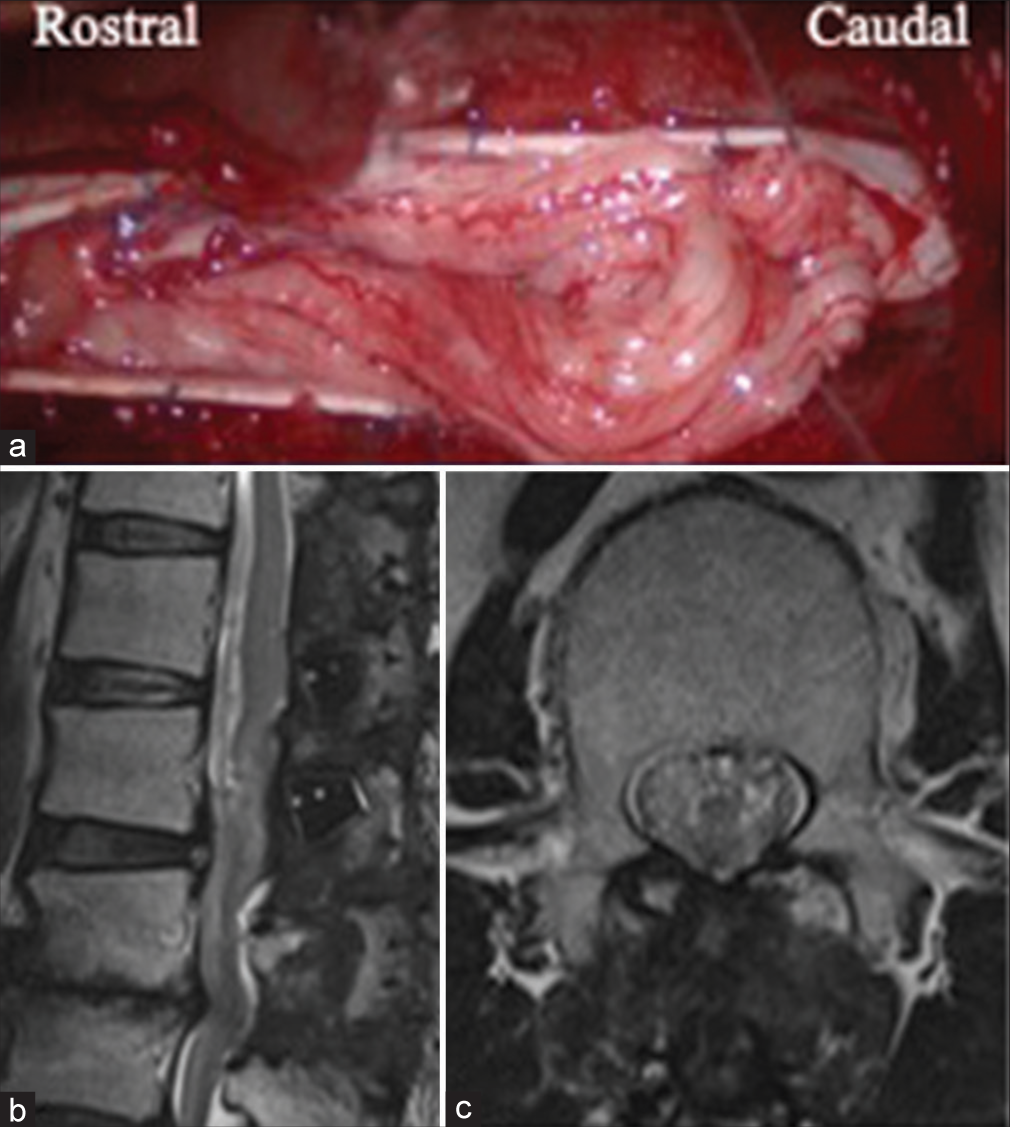
At surgery, a diffusely congested, swollen, and tortuous cauda equina herniated through the L1 durotomy; no accompanying cerebrospinal fluid was evident [
Figure 2:
A still image from the operative video shows congested and swollen cauda equina herniating out from the dural opening. Duraplasty with a Gore-Tex membrane was required to close the dura (a). Postoperative T2-weighted sagittal (b) and axial (c) images of the lumbar spine show disappearance of the hyperintense mass lesion.
Histology
The patient was diagnosed with the RNR syndrome as the histological examination revealed congested/edematous nerve root tissue without accompanying tumor.
Postoperative course
Within 1-week postoperatively, the patient’s lower extremity symptoms improved. The 3-month follow-up MRI showed no residual mass, but a residual, somewhat clumped, cauda equina at the L1 level [
DISCUSSION
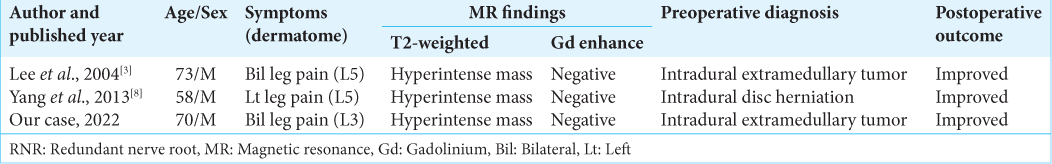
RNR occurs in 33.8–42.3% of severe LCS cases. It is common in males in their 50s and 60s who presents with the lower extremity symptoms attributed to L3-S1 root/cauda equina compression.[
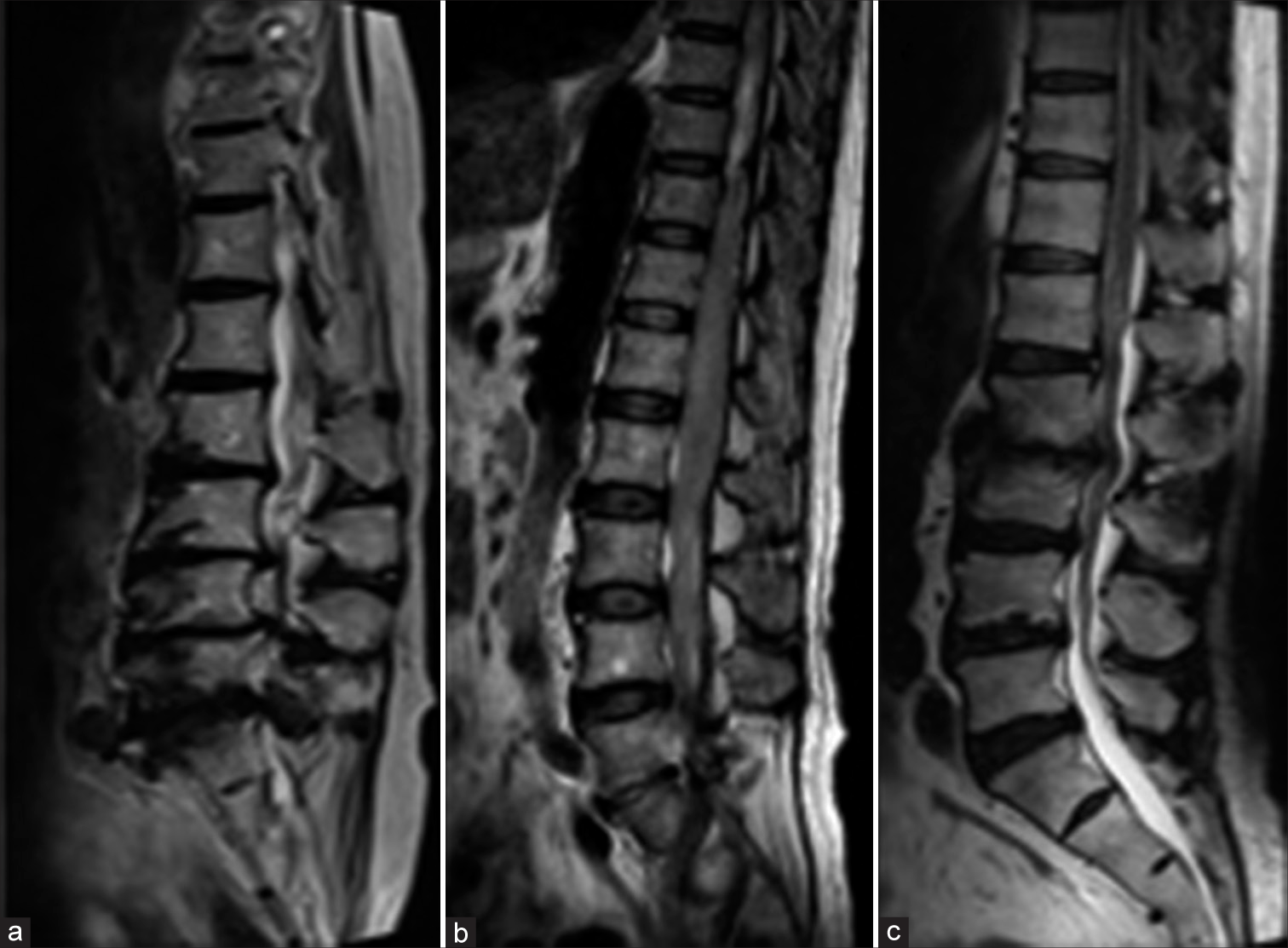
Figure 3:
T2-weighted sagittal images show a typical case of redundant nerve root (RNR) (a) and a case of malignant lymphoma (b). Comparing these images, it is clear that the MR findings in this case (c) are more similar to those of spinal tumor than to those of typical RNR, although the degree of enlargement of the cauda equina is different.
Treatment of RNR
Yokoyama et al.[
CONCLUSION
RNR can sometimes be difficult to diagnose with preoperative T2 MR images alone. However, the diagnosis of RNR should be considered when there is an intradural non-enhancing mass lesion adjacent to a level of severe lumbar stenosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Cressman MR, Pawl RP. Serpentine myelographic defect caused by a redundant nerve root. Case report. J Neurosurg. 1968. 28: 391-3
2. Kawasaki Y, Seichi A, Zhang L, Tani S, Kimura A. Dynamic changes of cauda equina motion before and after decompressive laminectomy for lumbar spinal stenosis with redundant nerve roots: Cauda equina activation sign. Global Spine J. 2019. 9: 619-23
3. Lee SH, Park SH, Hamm IS, Park YM. A case of the redundant nerve root syndrome mimicking intradural spinal tumor. J Korean Neurosurg Soc. 2004. 36: 160-2
4. Marques CJ, Hillebrand H, Papavero L. The clinical significance of redundant nerve roots of the cauda equina in T lumbar spinal stenosis patients: A systematic literature review and meta-analysis. Clin Neurol Neurosurg. 2018. 174: 40-7
5. Rengachary SS, McGregor DH, Watanabe I, Arjunan K, Kepes JJ. Suggested pathological basis of “redundant nerve root syndrome” of the cauda equina. Neurosurgery. 1980. 7: 400-11
6. Suzuki K, Ishida Y, Ohmori K, Sakai H, Hashizume Y. Redundant nerve roots of the cauda equina: Clinical aspects and consideration of pathogenesis. Neurosurgery. 1989. 24: 521-8
7. Verbiest H. A Radicular syndrome from developmental narrowing of the lumbar vertebral canal. J Bone Joint Surg Br. 1954. 36: 230-7
8. Yang SM, Park HK, Cho SJ, Chang JC. Redundant nerve roots of cauda equina mimicking intradural disc herniation: A case report. Korean J Spine. 2013. 10: 41-3
9. Yokoyama K, Kawanishi M, Yamada M, Tanaka H, Ito Y, Hirano M. Clinical significance of postoperative changes in redundant nerve roots after decompressive laminectomy for lumbar spinal canal stenosis. World Neurosurg. 2014. 82: 825-30