- Department of Neurosurgery, Nara Hospital Kindai University Faculty of Medicine, Ikoma, Nara, Japan
- Department of Laboratory Medicine, Nara Hospital Kindai University Faculty of Medicine, Ikoma, Nara, Japan
Correspondence Address:
Akira Watanabe
Department of Laboratory Medicine, Nara Hospital Kindai University Faculty of Medicine, Ikoma, Nara, Japan
DOI:10.4103/sni.sni_181_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Akira Watanabe, Kinya Nakanishi, Kazuo Kataoka, Tomoko Wakasa, Yoshio Ohta. Regrowth and progression of multiple calcifying pseudoneoplasms of the neuraxis: Case report. 04-Dec-2018;9:243
How to cite this URL: Akira Watanabe, Kinya Nakanishi, Kazuo Kataoka, Tomoko Wakasa, Yoshio Ohta. Regrowth and progression of multiple calcifying pseudoneoplasms of the neuraxis: Case report. 04-Dec-2018;9:243. Available from: http://surgicalneurologyint.com/surgicalint-articles/9104/
Abstract
Background:Calcifying pseudoneoplasms of the neuraxis (CAPNONs) are clinically rare, nonneoplastic, noninflammatory-calcified lesions of the central nervous system. Resection of a lesion usually indicates good prognosis without recurrence. However, we experienced a unique case of CAPNON that repeatedly recurred after resection.
Case Description:A 52-year-old woman with recurrence of an undiagnosed brain tumor, which was resected 12 years ago, was admitted to our institution. Three calcifying lesions along with perifocal edema were detected in the frontal interhemispheric fissure. We performed the second surgery for total removal of the lesions. The patient was diagnosed with CAPNON on the basis of the clinical features of the lesions and medical examination results. However, 14 months after the second surgery, recurrence occurred, and the patient has been followed up conservatively thereafter.
Conclusion:CAPNONs may indicate healing process associated with an unidentified agent. Maximum resection, including an unidentified agent, is necessary to prevent recurrence.
Keywords: Brain tumor, calcification, Calcifying pseudoneoplasms of the neuraxis, recurrence
INTRODUCTION
Calcifying pseudoneoplasms of the neuraxis (CAPNONs) are rare, heavily calcified lesions of the central nervous system. These lesions are nonneoplastic and noninflammatory. To the best of our knowledge, only 62 cases of CAPNON have been reported, including the present case (intracranial: 44; spinal: 18), since it was first identified in 1978.[
CASE HISTORY
Clinical course
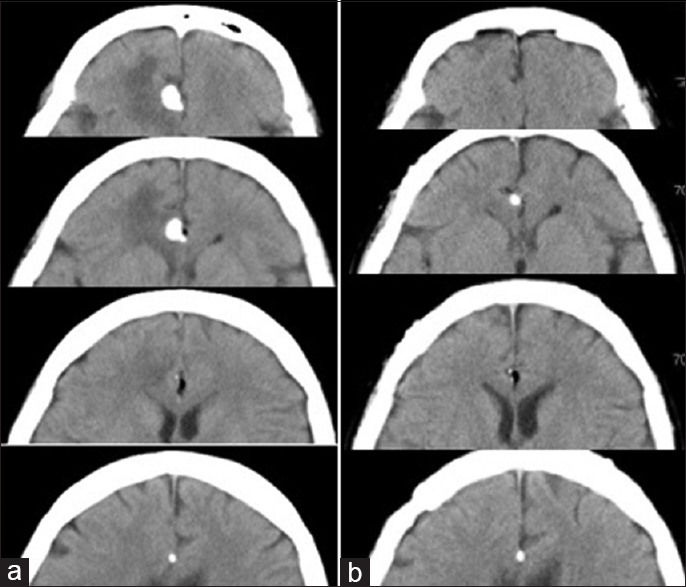
A 40-year-old woman presented to our institution with excessive somnolence. She was diagnosed with brain tumor in the right frontal lobe parenchyma following computed tomography (CT) scan of the head. The primary lesion was a high-density mass of approximately 11 mm in diameter. The mass had signs of calcification, and it was surrounded by low-density lipomas [
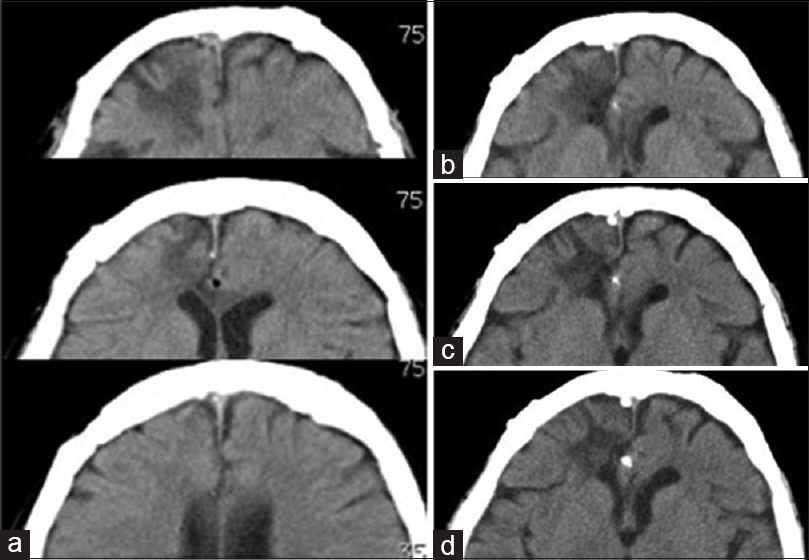
Figure 1
(a) Head computed tomography (CT) scan prior to the first surgery. A high-density calcification associated with a lipoma is seen in the frontal interhemispheric fissure. Swelling is also observed in the brain parenchyma surrounding the lesion. (b) Head CT-scan after the first surgery. The calcification and perifocal edema have resolved
We performed the first surgery to confirm the tumor diagnosis. Only the largest mass was removed. After surgery, CT scan revealed that the edema in the right frontal lobe had resolved [
After 12 years, the patient was admitted to our institution because of tumor recurrence. Head CT-scan revealed three highly dense mass lesions in the frontal interhemispheric fissure [
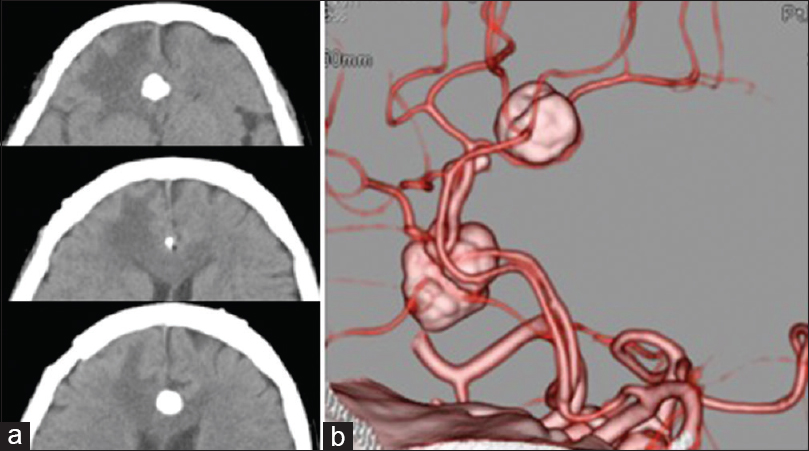
Figure 3
(a) Head computed tomography (CT) scan prior to the second surgery. Three high-density mass lesions are observed in the frontal interhemispheric fissure. Swelling is also observed in the brain parenchyma around the lesions. (b) 3D CT angiography reveals an area of calcification surrounding the anterior cerebral artery
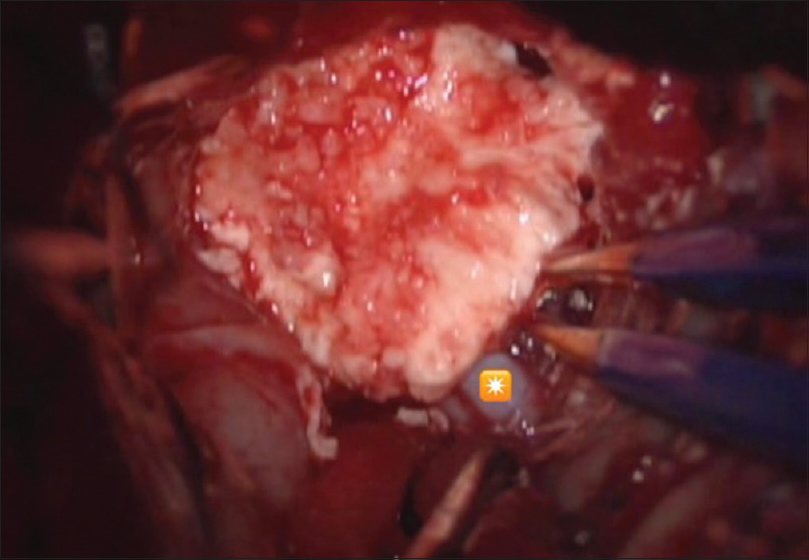
Second surgery
We performed bifrontal re-craniotomy and approached the lesion by tracing the right ACA from distal to proximal in the interhemispheric fissure and identified a calcifying mass lesion surrounding the ACA [
Figure 5
(a) Head computed tomography (CT) scan after the second surgery. Three high-density masses are removed without residual calcification. Edema around the lesions is reduced. (b–d) Head CT-scan 14, 18, and 24 months after the second surgery. A small high-density mass observed in the frontal interhemispheric cistern again. The mass lesion has grown to approximately 3.5 mm in diameter, and the size remains the same
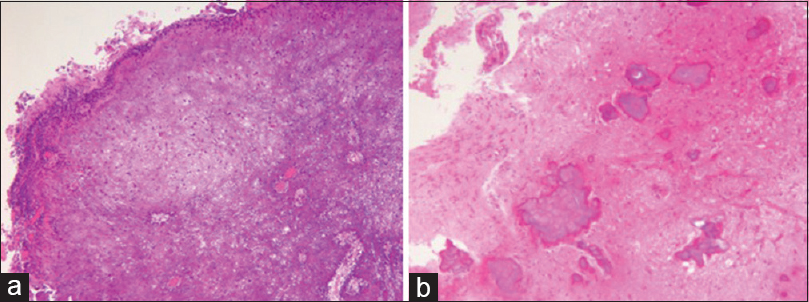
Histopathological examination revealed a hypocellular nodule with calcium deposition. The lymphocyte or plasma cells infiltrated into the margin of the mass. No malignant change occurred [Figure
Figure 6
(a) Specimens obtained during the second surgery. A strong nodular calcification observed in small vessels. Epithelioid or spindle cells are also observed at the margin of the nodule [hematoxylin–eosin (HE) staining ×40]. (b) Specimens obtained during the first surgery. Multiple calcifications are observed in the brain parenchyma (HE staining ×40)
DISCUSSION
CAPNONs are rare, calcified lesions of the central nervous system; they can occur in extra-axial, intra-axial, and intraosseous locations. Moreover, these lesions have been referred to as fibro-osseous lesions, cerebral calculi, brain stones, and calcifying pseudo-tumors. By exerting pressure on adjacent structures, they may cause various symptoms according to their anatomical location.
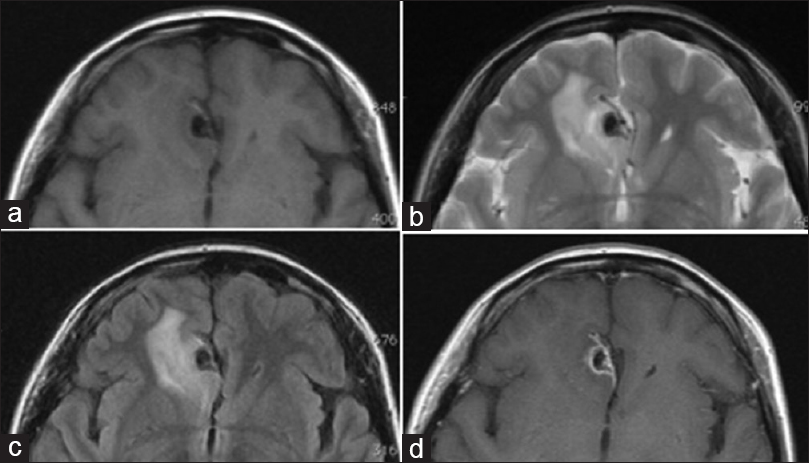
Typically, CT scan shows a CAPNON as a well-demarcated, densely calcified mass, whereas MRI shows uniform low-intensity signals on both T1- and T2-weighted images. Rim enhancement may also be observed on Gd-MRI. Shrier et al. have reported that gadolinium enhancement occurs when a lesion is associated with a highly vascular fibrous stroma.[
Considering the lack of mass effect, the presence of high-intensity areas around the lesions on T2-weighted images represents gliosis. However, in the present case, a high-intensity area was observed in the adjacent frontal lobe parenchyma prior to the first and second surgeries, which diminished after resection. High-intensity signal on T2-weighted images may indicate areas of edema. So far, six cases of perifocal edema associated with CAPNON have been identified, including the present case. Of them, two included extra-axial lesions that severely compressed the spinal cord and brain stem. Edema in these cases may be a result of the strong mass effect. However, in the present case, prior to the first surgery, no significant compression of the brain parenchyma had occurred. Therefore, an unidentified agent may have contributed to the lesion formation.
Histopathologically, CAPNON is typically characterized by hypocellular chondromyxoid matrix and variable amounts of fibrovascular stroma, which are often surrounded by palisading spindles or epithelioid cells and occasionally surrounded by multinucleate giant cells. Various states of calcification in the form of osseous metaplasia, scattered psammoma bodies, or calcium deposits have been observed in some cases; however, cellular proliferation and mitosis have not been reported. These features may be associated with the healing process that occurs in damaged tissues. Previous reports have indicated that epithelioid cells surrounding the lesion are positive for vimentin, possibly because of the presence of macrophages and lymphocytes and that most cells are positive for epithelial membrane antigen (EMA) and negative for glial fibrillary acidic protein and S-100. In the present case, epithelioid cells were only positive for vimentin.[
In the present case, CAPNONs were accompanied by lipomas. Salim et al. reported a similar case with agenesis of the corpus callosum, and other cases of lipomas were observed in the interhemispheric cistern.[
Calcifications are usually observed in the collagenous capsule or parenchyma surrounding the lipoma.[
Several authors have reported that CAPNONs progressed for 3–11 years.[
After the second surgery, we considered that the residual lesions may regrow in the future, and these lesions should be removed along with the affected tissue as much as possible. Although total resection was performed, regrowth occurred after the second surgery. Therefore, removing the tissues surrounding the calcifications may also be necessary in reducing the effect of the unknown agents that may cause regrowth. However, health-care professionals must be cautious during aggressive resection to avoid injury in the adjacent structures.
Stienen et al. have analyzed the association between residual tumors and recurrence based on previous cases. However, they have observed no significant difference in terms of recurrence between the patients who underwent complete resection and the patient who underwent incomplete resection.[
CONCLUSIONS
This study presented the case of a patient who required a second surgery to remove a CAPNON 12 years after the initial surgery. CAPNONs may be indicative of the healing process associated with an unidentified agent. Although surgery is typically associated with good prognosis, residual lesions may regrow. Thus, maximum resection must be performed, particularly in younger patients. Due to possible recurrence, patients should undergo periodic follow-ups. Moreover, further accumulation of cases is required to elucidate the underlying pathophysiology of CAPNON.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
No funding was received for this research.
Conflicts of interest
There are no conflicts of interest.
References
1. Aiken AH, Akgun H, Tihan T, Barbaro N, Glastonbury C. Calcifying pseudoneoplasms of the neuraxis: CT, MR imaging, and histologic features. AJNR Am J Neuroradiol. 2009. 30: 1256-60
2. Jun C, Burdick B. An unusual fibro-osseous lesion of the brain. Case report. J Neurosurg. 1984. 60: 1308-11
3. Kerr EE, Borys E, Bobinski M, Shahlaie K. Posterior fossa calcifying pseudoneoplasm of the central nervous system. J Neurosurg. 2013. 118: 896-902
4. Kwan MK, Abdelhai AM, Beng Saw L, Wei Chan CY. Symptomatic calcifying pseudotumor of the thoracic spine that resolved with the indomethacin treatment: A case report. Spine (Phila Pa 1976). 2012. 37: E1676-9
5. Rhodes RH, Davis RL. An unusual fibro-osseous component in intracranial lesions. Hum Pathol. 1978. 9: 309-19
6. Salim AA, Wilson PJ, Cherukuri RK, McKenzie S, Buckland ME. An unusual association of calcifying pseudoneoplasm of the neuraxis with interhemispheric lipoma and agenesis of corpus callosum. Pathology. 2012. 44: 657-9
7. Shrier DA, Melville D, Millet D, Qian J, Millet D, Nelson C. Fibro-osseous lesions involving the brain: MRI. Neuroradiology. 1999. 41: 18-21
8. Smith DM, Berry AD. Unusual fibro-osseous lesion of the spinal cord with positive staining for glial fibrillary acidic protein and radiological progression: A case report. Hum Pathol. 1994. 25: 835-8
9. Stienen MN, Abdulazim A, Gautschi OP, Schneiderhan TM, Hildebrandt G, Lucke S. Calcifying pseudoneoplasms of the neuraxis (CAPNON): Clinical features and therapeutic options. Acta Neurochir. 2013. 155: 9-17
10. Truwit CL, Barkovich AJ. Pathogenesis of intracranial lipoma: An MR study in 42 patients. AJR Am J Roentgenol. 1990. 155: 855-64
11. Yilmaz N, Unal O, Kiymaz N, Yilmaz C, Etlik O. Intracranial lipomas–a clinical study. Clin Neurol Neurosurg. 2006. 108: 363-8