- Department of Surgical Specialties, Neurosurgery Teaching and Assistance Unit, Pedro Ernesto University Hospital, Rio de Janeiro State University, Rio de Janeiro, Brazil,
- Department of Surgical Specialties, Thoracic Surgery Teaching and Assistance Unit, Pedro Ernesto University Hospital, Rio de Janeiro State University, Rio de Janeiro, Brazil.
Correspondence Address:
Julia Pereira Muniz Pontes, Department of Surgical Specialties, Neurosurgery Teaching and Assistance Unit, Pedro Ernesto University Hospital, Rio de Janeiro State University, Rio de Janeiro, Brazil.
DOI:10.25259/SNI_88_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Julia Pereira Muniz Pontes1, Pedro Henrique Costa Ferreira-Pinto1, Louise Ferreira Nascimento Pestana da Costa1, Bernardo Martins Rodrigues Martha1, Wellerson Novaes da Silva1, Maria Eduarda Freire Lopes Senior1, Tadeu Diniz Ferreira2, Elington Lannes Simoes1, Flavio Nigri1. Resection arthroplasty for isolated costotransverse joint osteoarthritis: A case report and literature review. 18-Feb-2022;13:62
How to cite this URL: Julia Pereira Muniz Pontes1, Pedro Henrique Costa Ferreira-Pinto1, Louise Ferreira Nascimento Pestana da Costa1, Bernardo Martins Rodrigues Martha1, Wellerson Novaes da Silva1, Maria Eduarda Freire Lopes Senior1, Tadeu Diniz Ferreira2, Elington Lannes Simoes1, Flavio Nigri1. Resection arthroplasty for isolated costotransverse joint osteoarthritis: A case report and literature review. 18-Feb-2022;13:62. Available from: https://surgicalneurologyint.com/surgicalint-articles/11397/
Abstract
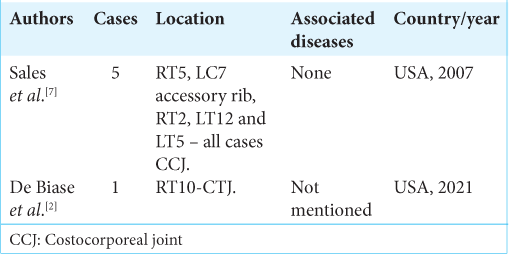
Background: Symptomatic isolated costovertebral joint (CVJ) osteoarthritis is rare, and establishing this diagnosis is often difficult. There are few reports in the literature about how to surgically manage these lesions. Our aim was to describe a case of isolated osteoarthritis of the costotransverse joint (CTJ) successfully treated with a resection arthroplasty.
Case Description: A 51-year-old female presented with 3 years of the right paravertebral T 10-level back and radiating pain. No conservative treatment modality effectively resolved this pain (i.e., these included anti-inflammatory medications, physiotherapy, and joint blockages). MRI, CT, and technetium-99m methylene diphosphonate bone scintigraphy demonstrated inflammatory changes involving the right T10 CTJ. Following resection arthroplasty, the patient’s symptoms abated.
Conclusion: Symptomatic osteoarthritis of the right T10 CVJ successfully resolved following costotransversectomy for joint resection arthroplasty.
Keywords: Costocorporeal joint, Costotransverse joint, Costotransversectomy, Costovertebral joint, Isolated osteoarthritis, Resection arthroplasty
INTRODUCTION
The costocorporeal joint (CCJ) and costotransverse joint (CTJ) are both typically grouped as costovertebral joints (CVJs).[
Although many patients may favorably respond to conservative treatment modalities, some refractory cases will require resection arthroplasty.[
CLINICAL PRESENTATION
A 51-year-old female presented with the right thoracic back pain at the T10 level of 3 years duration. Her neurological examination was normal. Prior unsuccessful treatment modalities had included B1, B6, and B12 replacement therapy, analgesics, nonsteroidal anti-inflammatory drugs, opioids, gabapentin, physiotherapy, acupuncture, and global posture reeducation. All laboratory tests for rheumatoid disease (antinuclear antibodies, rheumatoid factor and anticyclic citrullinated peptide antibodies, erythrocyte sedimentation rate, and C-reactive protein) were negative.
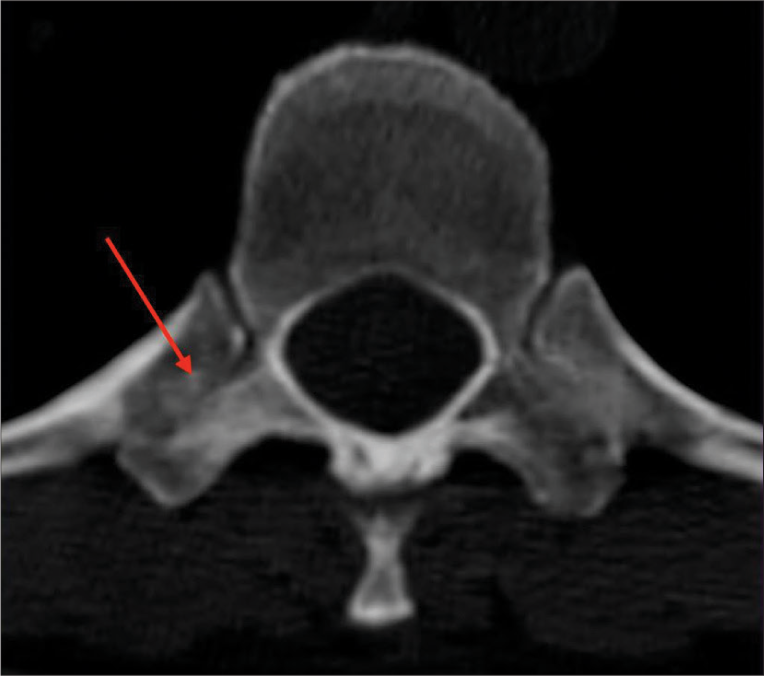
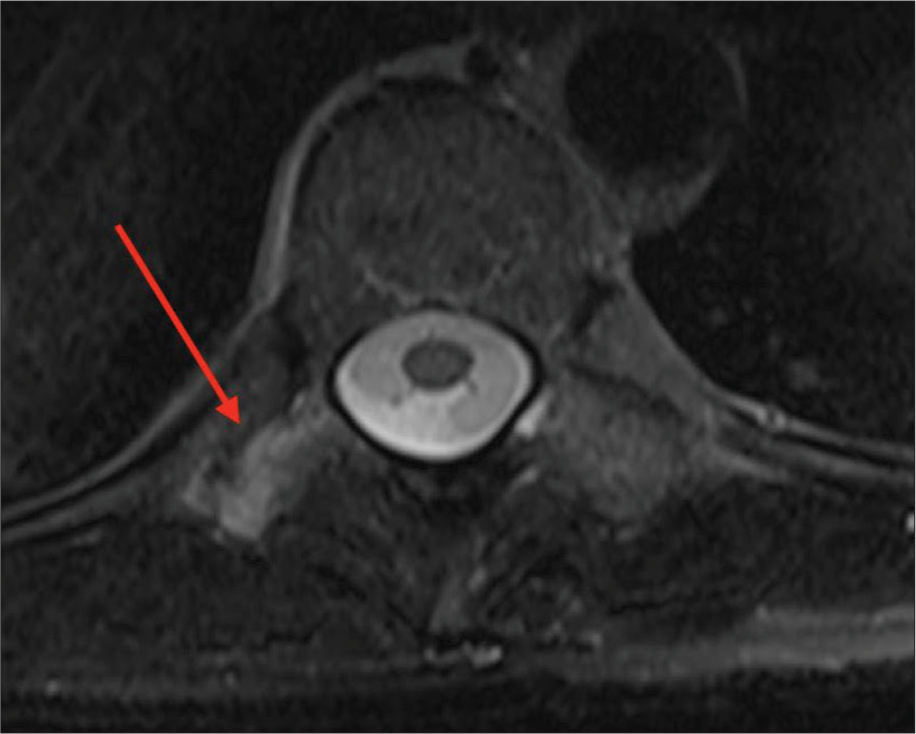
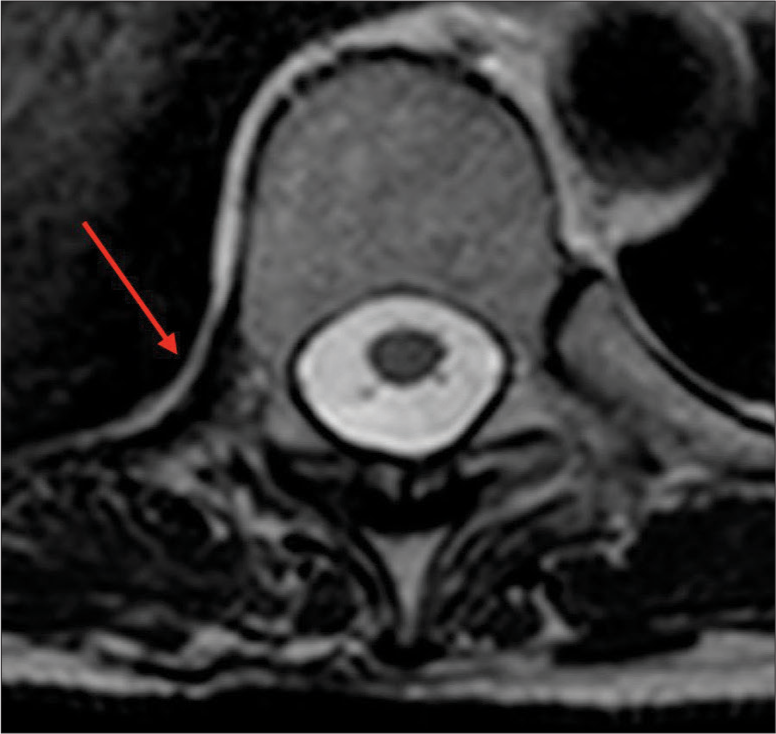
Magnetic resonance imaging (MRI) and computed tomography (CT) studies of the right T10 CTJ
The thoracic CT revealed subchondral sclerosis involving the right T10 transverse process, while the MRI demonstrated hyperintensity of the right T10 CTJ (i.e., on T2 weighted and STIR extending to adjacent muscle adipose planes and T10 nerve foramen [
Surgery and outcome
The patient underwent a right T10 CTJ resection arthroplasty.[
DISCUSSION
CVJ osteoarthritis is common, but often asymptomatic.[
CONCLUSION
The few case descriptions in the literature combined with this case indicate that resection arthroplasty of an osteoarthritis CVJ is the treatment of choice.
Ethics
This case report was conducted in accordance with ethical standards of our university hospital and the local ethics committee.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
The research was performed as part of the employment of the authors by Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ) and Center of High Complexity Neurosurgery Intern Patients (NIP-NAC) from Rio de Janeiro State Department of Health (SES-RJ).
Conflicts of interest
There are no conflicts of interest.
References
1. Cohen MJ, Ezekiel J, Persellin RH. Costovertebral and costotransverse joint involvement in rheumatoid arthritis. Ann Rheum Dis. 1978. 37: 473-5
2. De Biase G, Gassie K, Abode-Iyamah K, Nottmeier E. Image-guided right T10 costotransverse joint resection for costotransversitis: Operative technique and nuances: 2-Dimensional operative video. Oper Neurosurg (Hagerstown). 2021. 21: E254
3. Gazitt T, Nassrallah N, Zisman D. Erosive costovertebral joint arthritis-an uncommon manifestation of ankylosing spondylitis. Arthritis Rheumatol. 2021. 73: 179
4. Moore KL, Dalley AF, Agur AM.editors. Clinically Oriented Anatomy. Philadelphia, PA: Lippincott Williams and Wilkins; 2014. p. 79
5. Nathan H, Weinberg H, Robin GC, Aviad I. The costovertebral joints, anatomical-clinical observations in arthritis. Arthritis Rheum. 1964. 7: 228-40
6. Saker E, Graham RA, Nicholas R, D’Antoni AV, Loukas M, Oskouian RJ. Ligaments of the costovertebral joints iWncluding biomechanics, innervations, and clinical applicatio0ns: A comprehensive review with application to approaches to the thoracic spine. Cureus. 2016. 8: e874
7. Sales JR, Beals RK, Hart RA. Osteoarthritis of the costovertebral joints: The results of resection arthroplasty. J Bone Joint Surg Br. 2007. 89: 1336-9