- Department of Neurosurgery, Division of Surgery, Hospital Universitario Lauro Wanderley - UFPB, Joao Pessoa, Brazil.
- Department of Neurology and Neurosurgery, Hospital Sao Paulo, Sao Paulo, Brazil.
- Department of Neurology, State University of Campinas (UNICAMP), Campinas, Sao Paulo, Brazil.
- Department of Neurosurgery, Instituto de Assistencia Medica ao Servidor Publico do Estado de Sao Paulo, Sao Paulo, Brazil.
DOI:10.25259/SNI_322_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Alecio Cristino Evangelista Santos Barcelos1, Franz Jooji Onishi2, Andrei Fernandes Joaquim3, Ricardo Vieira Botelho4. Review of best classification systems for diagnosing and treating thoracolumbar spine trauma. 31-May-2021;12:242
How to cite this URL: Alecio Cristino Evangelista Santos Barcelos1, Franz Jooji Onishi2, Andrei Fernandes Joaquim3, Ricardo Vieira Botelho4. Review of best classification systems for diagnosing and treating thoracolumbar spine trauma. 31-May-2021;12:242. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10841
Abstract
Background: Improved thoracolumbar spine trauma classification (TLSTC) systems can better help diagnose and treat thoracolumbar spine trauma (TLT). Here, we identified the types of injury (rationale and description), instability criteria, and treatment guidelines of TLSTC.
Methods: We used the PubMed/MEDLINE database to assess TLSTC according to the following variables: injury morphology, injury mechanism, spinal instability criteria, neurological status, and treatment guidelines.
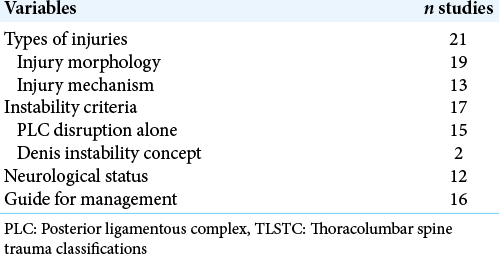
Results: Twenty-one studies, 18 case series and three reviews were included in the study. Treatment guidelines were proposed in 16 studies. The following three major parameters were identified in TLSTC studies: injury morphology (19/21 studies), posterior ligamentous complex (PLC) disruption alone as the main spinal instability criterion (15 studies), and neurological damage (12 studies). Most classification systems neglected the severity of vertebral body comminution.
Conclusion: We identified here the 3 main parameters for the evaluation of diagnosis and treatment of TLT: injury morphology, PLC disruption, and neurological damage. Based on our review, we may conclude that further clinical validation studies of TLSTC are warranted.
Keywords: Classifications, Management, Spinal fractures, Spinal instability, Thoracolumbar
INTRODUCTION
The present study is a systematic review of thoracolumbar spine trauma classifications (TLSTC). We specifically analyzed the types of injury (rationale and description), spinal instability criteria, and treatment guidelines. This led to the assessment of five main variables: injury morphology, injury mechanism, spinal instability criteria, neurological status, and treatment guidelines.
MATERIALS AND METHODS
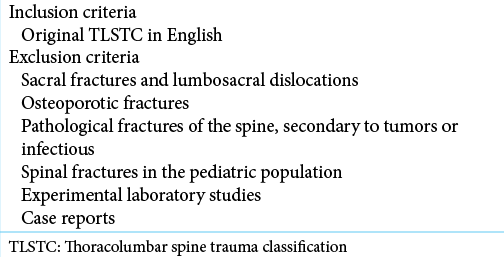
A systematic review was performed using multiple Eligibility criteria [
RESULTS
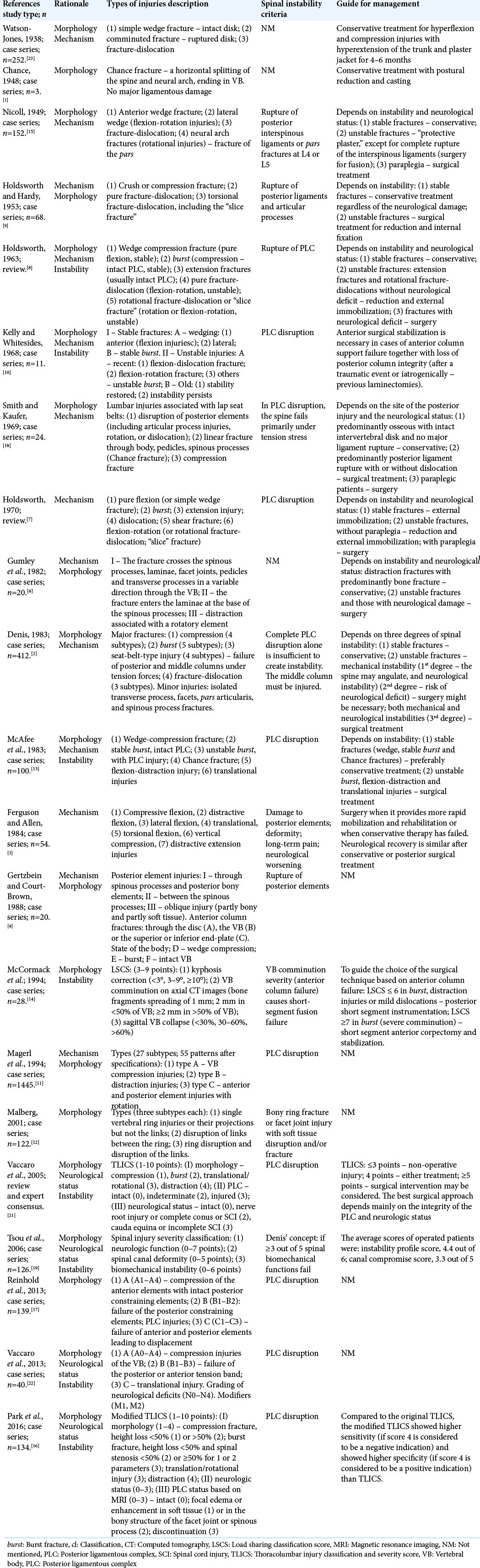
The characteristics of the 21 TLSTC studies and data description are summarized in [
Types of injuries – rationale and description
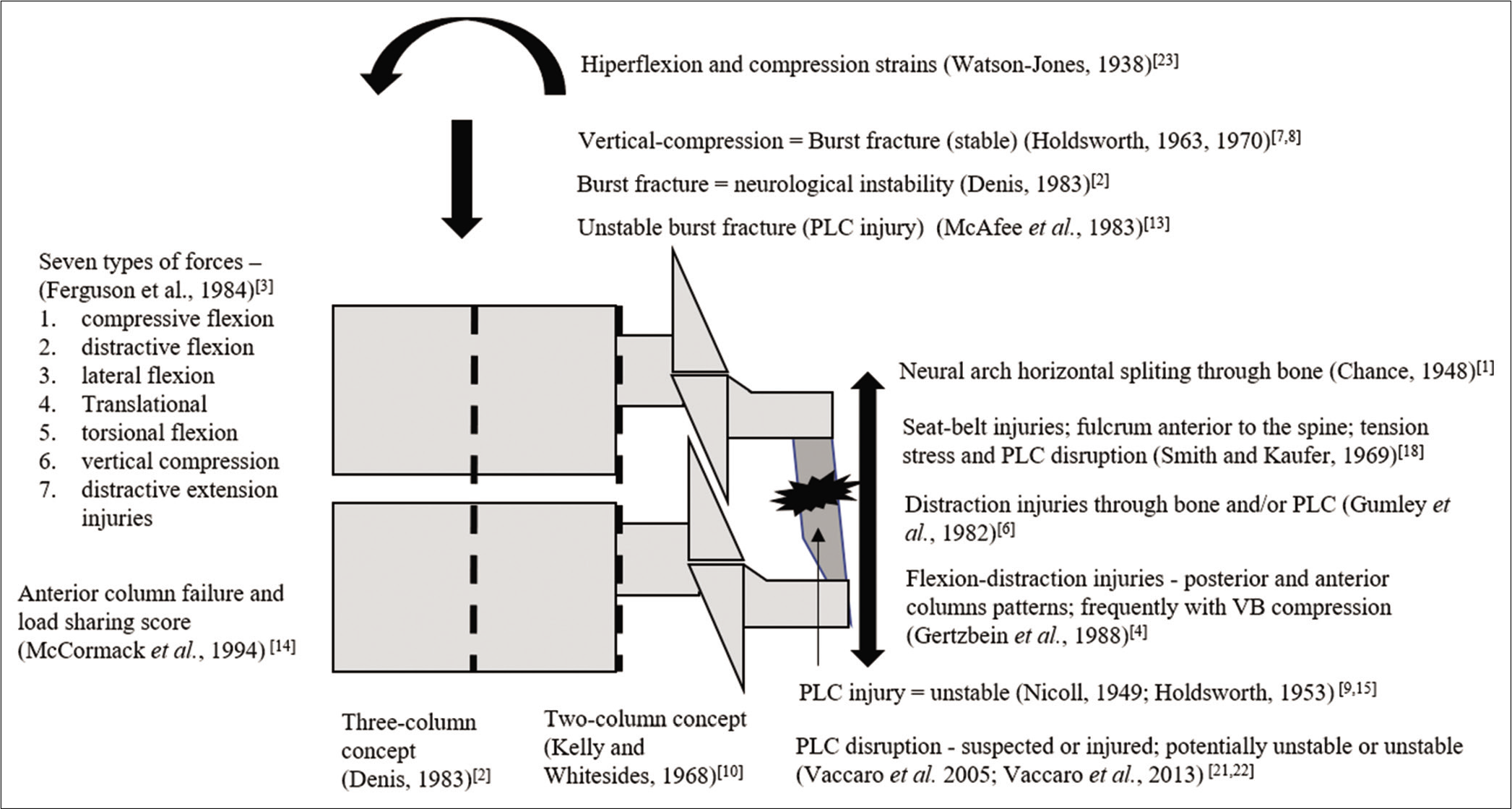
The types of injuries were based on injury morphology (19 studies) and/or injury mechanism (13 studies). Some studies also included spinal instability (8 studies)[
Vertebral body (VB) fractures
Watson-Jones described three types of VB fractures: simple wedge, comminuted, and dislocation. The comminuted fracture was later described as burst fracture.[
Trauma
Holdsworth initially described four forces or types of trauma that caused spinal fractures, that is, flexion, flexion/rotation, extension, and compression. They defined “burst fracture” as an injury caused by a vertical compression force. Pure fracture-dislocation occurred in the presence of posterior ligament rupture. Possible dislocation was limited by interlocking of the articular processes (Holdsworth).[
Flexion distraction injuries
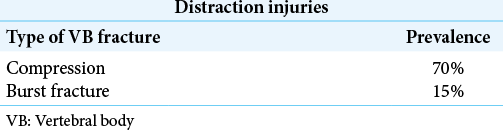
Four studies introduced the descriptions that define flexion-distraction injuries. Chance (1948) described three patients with horizontal splitting of the neural arch that reached the upper surface of the body without severe ligamentous damage.[
Table 4:
Prevalence and type of VB fracture in distraction injuries.[
All injuries
Nicoll’s classification was the first to embrace all types of fractures, including compression fractures, dislocations, and neural arch fractures, influenced by Watson-Jones and Chance.[
Spinal instability criteria
Seventeen studies defined spinal instability, 15 of them showing dependence only on disruption of the PLC elements [
Guide for management
Sixteen studies reported on surgery.[
PLC disruption
Nicoll and Holdsworth and Hardy were the first authors to divide TL injuries into stable, with intact posterior ligaments and unstable, with ruptured posterior ligaments and facet joints.[
Anterior column failure
Three studies related anterior column failure to spinal instability and provided surgical indication. Kelly and Whitesides indicated ventral stabilization when it is associated with loss of posterior column integrity.[
Neurological status
Surgical treatment was initially indicated for fractures of paraplegic patients to allow early mobilization, better nursing care, and prevention of pressure sores but was later also indicated for incomplete neurological injuries.[
DISCUSSION
This review demonstrated the evolution of concepts in the diagnosis and treatment of thoracolumbar spine trauma.
Three major parameters were included in TLSTC studies: injury morphology, spinal instability (especially PLC disruption), and neurological damage.
Injury morphology
There have been significant achievements in the understanding of the cause-effect relationship of the traumatic event between the 1960s and 1980s, with the descriptions of the mechanisms of injury.[
Spinal instability and PLC disruption
The fundamental role of posterior ligament rupture in spinal instability has been widely reported. Unstable injuries include (1) translational injury in the lateral, ventral, or dorsal directions, (2) torsional/rotational injury, with or without dislocation, which is often associated with proximal fracture of adjacent ribs, and (3) distraction injury. Holdsworth and Hardy stated that “displacements seen on radiological examinations were not necessarily an accurate indication of the actual displacement at the time of injury.”[
Frequently, VB fractures occur together with distraction and rotational injuries. If these fractures are secondary to distractive or torsional flexions, VB height is preserved or even increased. However, compression or burst fractures may also occur when there are combined forces such as compressive flexion or vertical compression, respectively.[
Neurological damage
Neurological deficit is the most debilitating sequela of TLT. Although the primary spinal cord injury is caused mainly by the traumatic event, ongoing neural compression further compromises the prognosis. Nicoll recommended surgical treatment for paraplegic patients to improve rehabilitation care.[
Guide for management
PLC injury has influenced most of the TLSTC as the main surgical indication since the 1940s and 1950s.[
PLC integrity, neurological status, and injury morphology are used in the TLICS system to guide treatment, creating a new methodological standard for TLSTC.[
However, there are still some limitations in differentiating between stable burst fractures (A3 and A4) and unstable burst fractures, also called B2 injuries associated with bursts.[
The LSCS introduced the evaluation of VB comminution severity as a relevant factor in the surgical decision-making process.[
This study has some limitations. The long period reviewed covered classifications based on their timely available radiological diagnostic tools. This may have influenced the identification of the type of injury and its treatment. The highest level of evidence among the studies was 4 (case series). Finally, we have included only peer-reviewed reports in the English language available in the MEDLINE database.
CONCLUSION
The three main parameters identified in TLSTC for diagnosis and treatment is injury morphology, PLC disruption, and neurological damage. Although VB comminution severity may affect spinal stability, it has been neglected by most classifications. Severity scores are used to standardize diagnosis and treatment. Based on our review, we may conclude that further clinical validation studies of TLSTC are warranted.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Chance GQ. Note on a type of flexion fracture of the spine. Br J Radiol. 1948. 21: 452
2. Denis F. The Three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983. 8: 817-31
3. Ferguson RL, Allen BL. A mechanistic classification of thoracolumbar spine fractures. Clin Orthop Relat Res. 1984. 189: 77-88
4. Gertzbein SD, Court-Brown CM. Flexion-distraction injuries of the lumbar spine mechanisms of injury and classification. Clin Orthop Relat Res. 1988. 227: 52-60
5. Gertzbein SD, Court-Brown CM. The rationale for the management of flexion-distraction injuries of the thoracolumbar spine based on a new classification. J Spinal Disord. 1989. 2: 176-83
6. Gumley G, Taylor TKF, Ryan MD. Distraction fractures of the lumbar spine. J Bone Joint Surg Ser B. 1982. 64: 520-5
7. Holdsworth F. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg Am. 1970. 52: 1534-51
8. Holdsworth FW. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg Br. 1963. 45: 6-20
9. Holdsworth FW, Hardy A. Early treatment of paraplegia from fractures of the thoraco-lumbar spine. J Bone Joint Surg Br. 1953. 35: 540-50
10. Kelly RP, Whitesides TE. Treatment of lumbodorsal fracture-dislocations. Ann Surg. 1968. 167: 705-17
11. Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994. 3: 184-201
12. Malberg MI. A new system of classification for spinal injuries. Spine J. 2001. 1: 18-25
13. McAfee PC, Yuan HA, Fredrickson BE, Lubicky JP. The value of computed tomography in thoracolumbar fractures. An analysis of one hundred consecutive cases and a new classification. J Bone Joint Surg Ser A. 1983. 65: 461-73
14. McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Phila Pa 1976). 1994. 19: 1741-4
15. Nicoll EA. Fractures of the dorso-lumbar spine. J Bone Joint Surg Br. 1949. 31: 376-94
16. Park HJ, Lee SY, Park NH, Shin HG, Chung EC, Rho MH. Modified thoracolumbar injury classification and severity score (TLICS) and its clinical usefulness. Acta Radiol. 2016. 57: 74-81
17. Reinhold M, Audigé L, Schnake KJ, Bellabarba C, Dai LY, Oner FC. AO spine injury classification system: A revision proposal for the thoracic and lumbar spine. Eur Spine J. 2013. 22: 2184-201
18. Smith WS, Kaufer H. Patterns and mechanisms of lumbar injuries associated with lap seat belts. J Bone Joint Surg Am. 1969. 51: 239-54
19. Tsou PM, Wang J, Khoo L, Shamie AN, Holly L. A thoracic and lumbar spine injury severity classification based on neurologic function grade, spinal canal deformity, and spinal biomechanical stability. Spine J. 2006. 6: 636-47
20. Vaccaro A, Schroeder G, Kepler C, Oner FC, Vialle L, Kandziora F. The surgical algorithm for the AOSpine thoracolumbar spine injury classification system. Eur Spine J. 2016. 25: 1087-94
21. Vaccaro AR, Lehman RA, Hurlbert RJ. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976). 2005. 30: 2325-33
22. Vaccaro AR, Oner C, Kepler CK, Dvorak M, Schnake K, Bellabarba C. AOSpine thoracolumbar spine injury classification system: Fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976). 2013. 38: 2028-37
23. Watson-Jones BY. The results of postural reduction of fractures of the spine. J Bone Joint Surg Am. 1938. 20: 567-86