- Department of Neurosurgery, All India Institute of Medical Sciences, Raipur, Chhattisgarh, India.
- Director and CEO (ENT Surgeon), All India Institute of Medical Sciences, Raipur, Chhattisgarh, India.
- Department of General Surgery, All India Institute of Medical Sciences, Raipur, Chhattisgarh, India.
- Department of ENT, All India Institute of Medical Sciences, Raipur, Chhattisgarh, India.
- Department of Paediatrics, All India Institute of Medical Sciences, Raipur, Chhattisgarh, India.
- Department of Pharmacology, All India Institute of Medical Sciences, Raipur, Chhattisgarh, India.
Correspondence Address:
Charandeep Singh Gandhoke, Department of Neurosurgery, All India Institute of Medical Sciences, Raipur, Chhattisgarh, India.
DOI:10.25259/SNI_1065_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Anil Kumar Sharma1, Nitin M. Nagarkar2, Charandeep Singh Gandhoke1, Siddharth Sharma1, Mohit Juneja1, Zijano M. Kithan3, Aakash Aggarwal4, Ripu Daman Arora4, Rupa Mehta4, Simran Syal5, Shailendra D. Anjankar1, Pugazhenthan Thangaraju6. Rhinocerebral mucormycosis (RCM): To study the clinical spectrum and outcome of 61 cases of RCM managed at a tertiary care center in India. 20-Jan-2023;14:15
How to cite this URL: Anil Kumar Sharma1, Nitin M. Nagarkar2, Charandeep Singh Gandhoke1, Siddharth Sharma1, Mohit Juneja1, Zijano M. Kithan3, Aakash Aggarwal4, Ripu Daman Arora4, Rupa Mehta4, Simran Syal5, Shailendra D. Anjankar1, Pugazhenthan Thangaraju6. Rhinocerebral mucormycosis (RCM): To study the clinical spectrum and outcome of 61 cases of RCM managed at a tertiary care center in India. 20-Jan-2023;14:15. Available from: https://surgicalneurologyint.com/surgicalint-articles/12118/
Abstract
Background: Mucormycosis is a life-threatening infection of the paranasal sinuses and nasal cavities that can easily spread to the orbit and the brain. It is caused by fungi of the family Mucoraceae. We present a case series of 61 patients diagnosed and treated for rhinocerebral mucormycosis (RCM) at a single tertiary health care center.
Methods: After obtaining ethical clearance, all patient files with a final diagnosis of RCM were thoroughly analyzed in departmental records and a master chart was prepared. The study evaluated the etiology, clinical spectrum, diagnosis, management, complications, and outcome at 3 months of RCM cases.
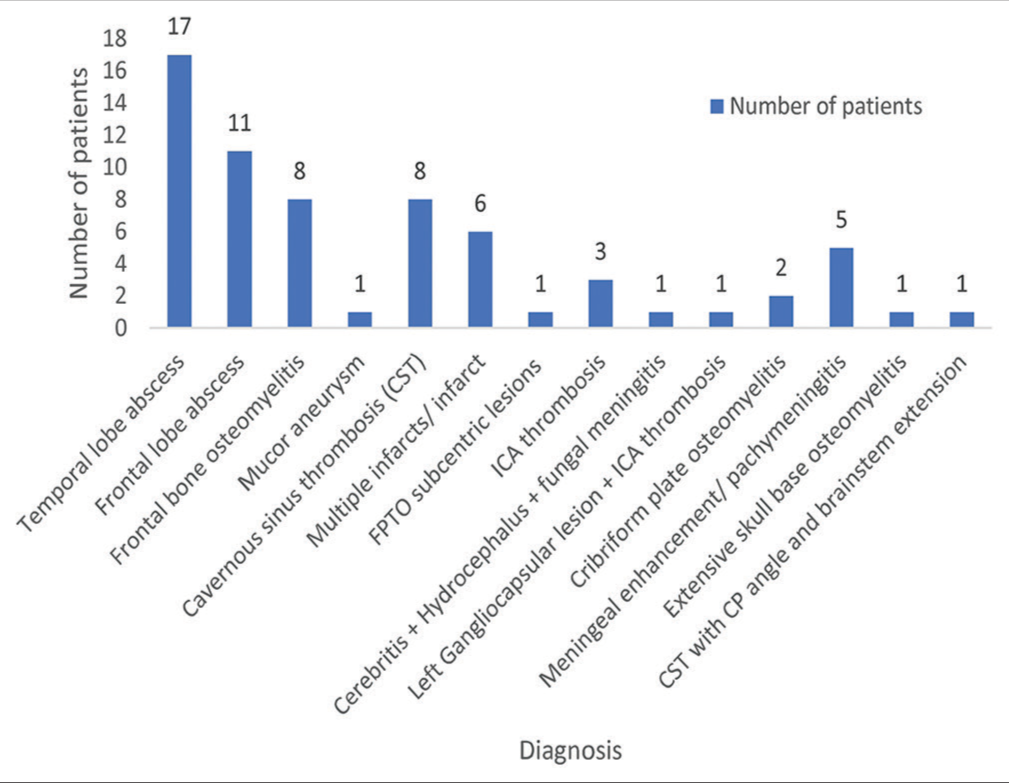
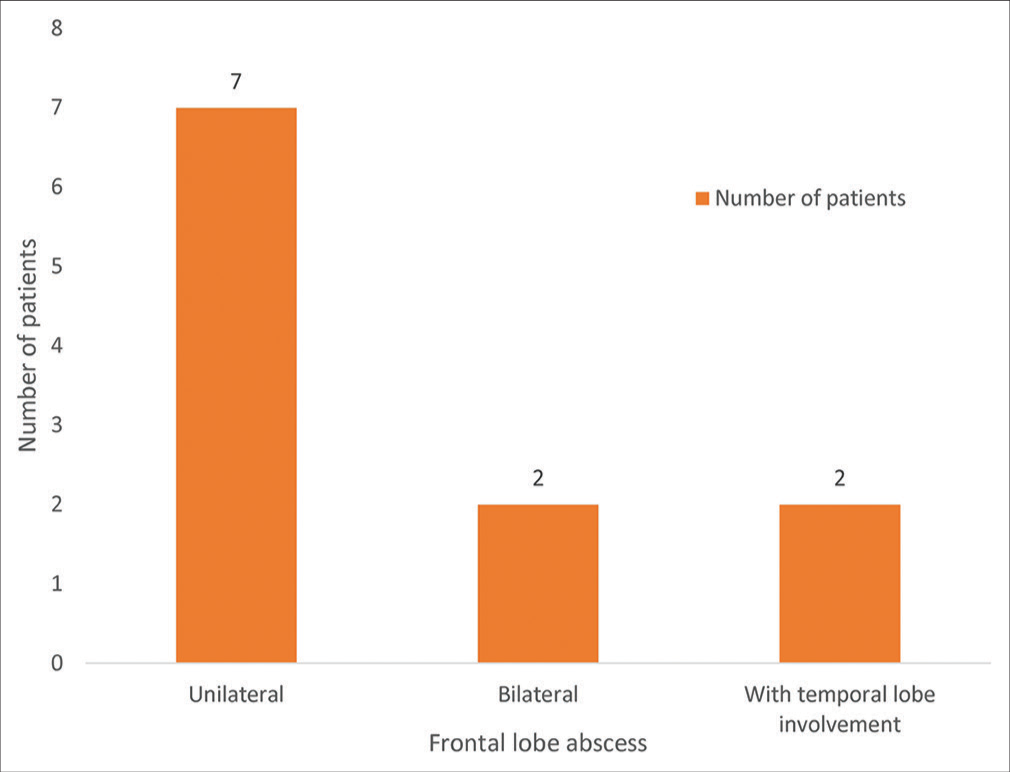
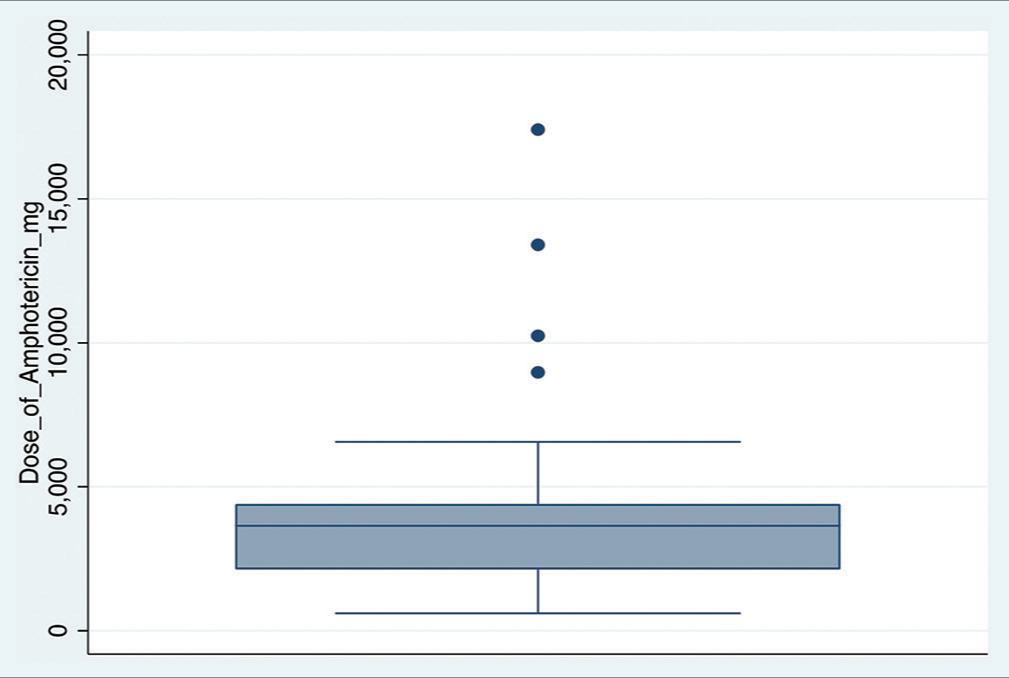
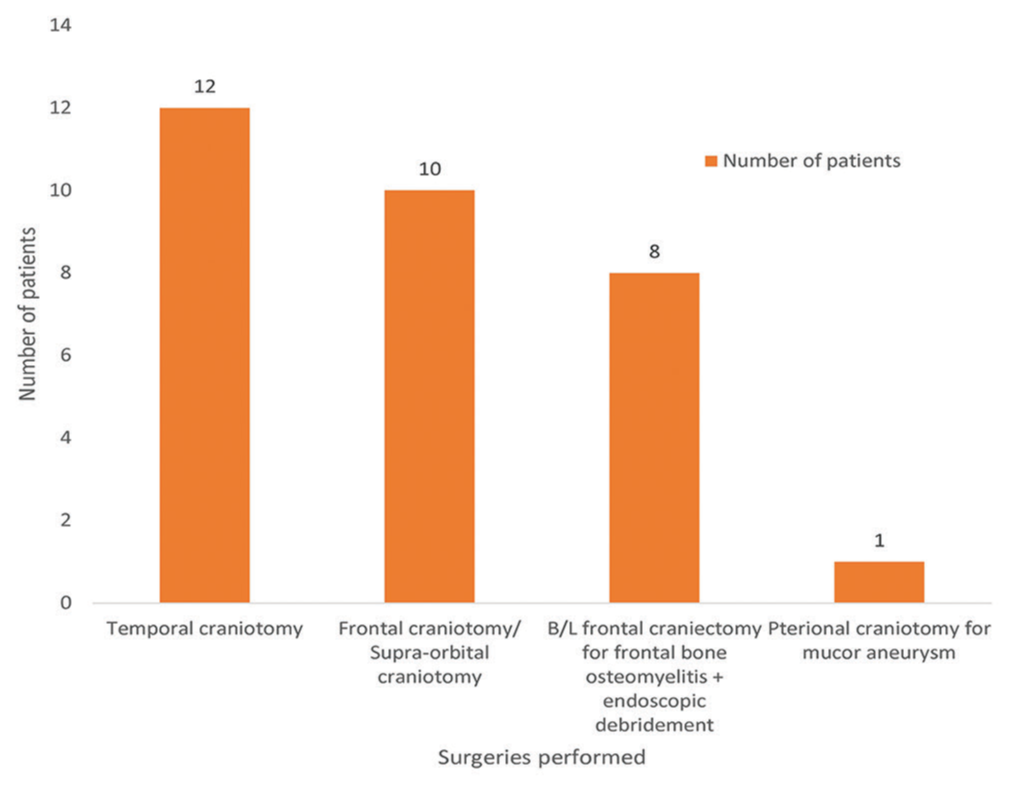
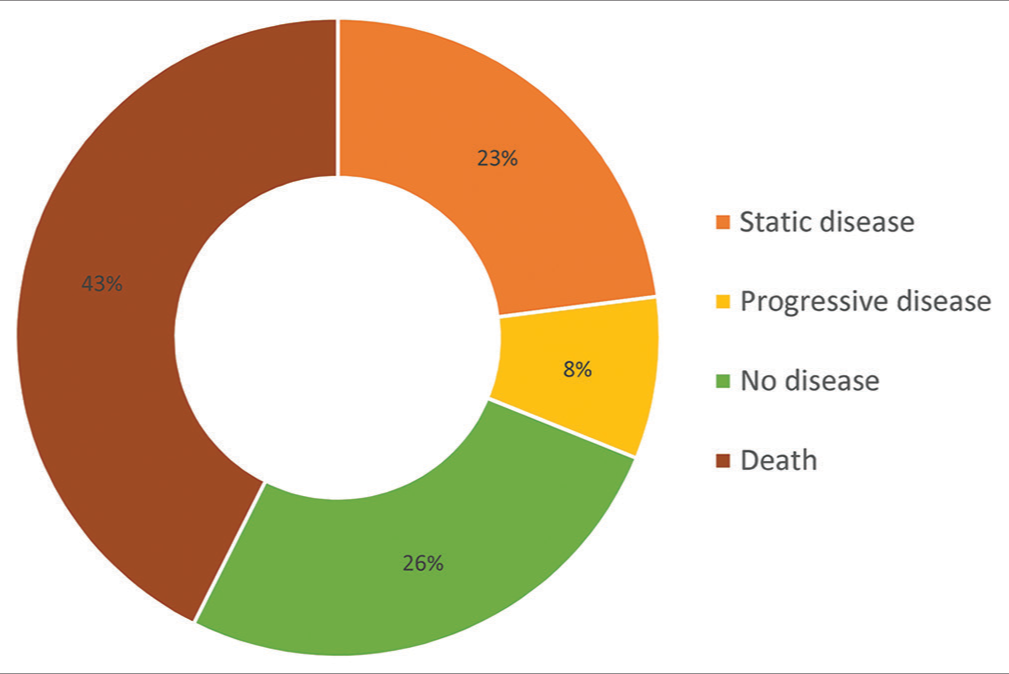
Results: About 93.4% of the RCM cases were diabetic and an equal number had a past history of COVID infection. About 85.2% had received steroids for the treatment of coronavirus disease 2019 infection. The most common presentation of RCM was temporal lobe abscess (25.7%) followed by frontal lobe abscess (16.6%). At 3 months post-diagnosis, mortality in our study was 42.6%. About 26.2 % of the RCM cases had no disease, 23% had a static disease, and 8.2% had progressive disease at the end of 3 months.
Conclusion: We report the largest single-center case series of RCM, comprising 61 patients. This case series underscores the importance of the early diagnosis and prompt treatment for a better prognosis for this dreadful disease. The three pillars of treatment for RCM cases include reversal of the immunosuppressive state, administration of antifungal drugs, and extensive surgical debridement. In spite of all this, mortality remains high.
Keywords: COVID-19, Diabetic, Mucormycosis, Rhinocerebral, Steroids
INTRODUCTION
Rhinocerebral mucormycosis (RCM) is a necrotizing, angioinvasive, life-threatening infection of the paranasal sinuses, and nasal cavities that can easily spread to the orbit and the brain. It is caused by fungi of the family Mucoraceae, the principal pathogens being Rhizopus, Lichtheimia, Apophysomyces, and Rhizomucor.[
MATERIALS AND METHODS
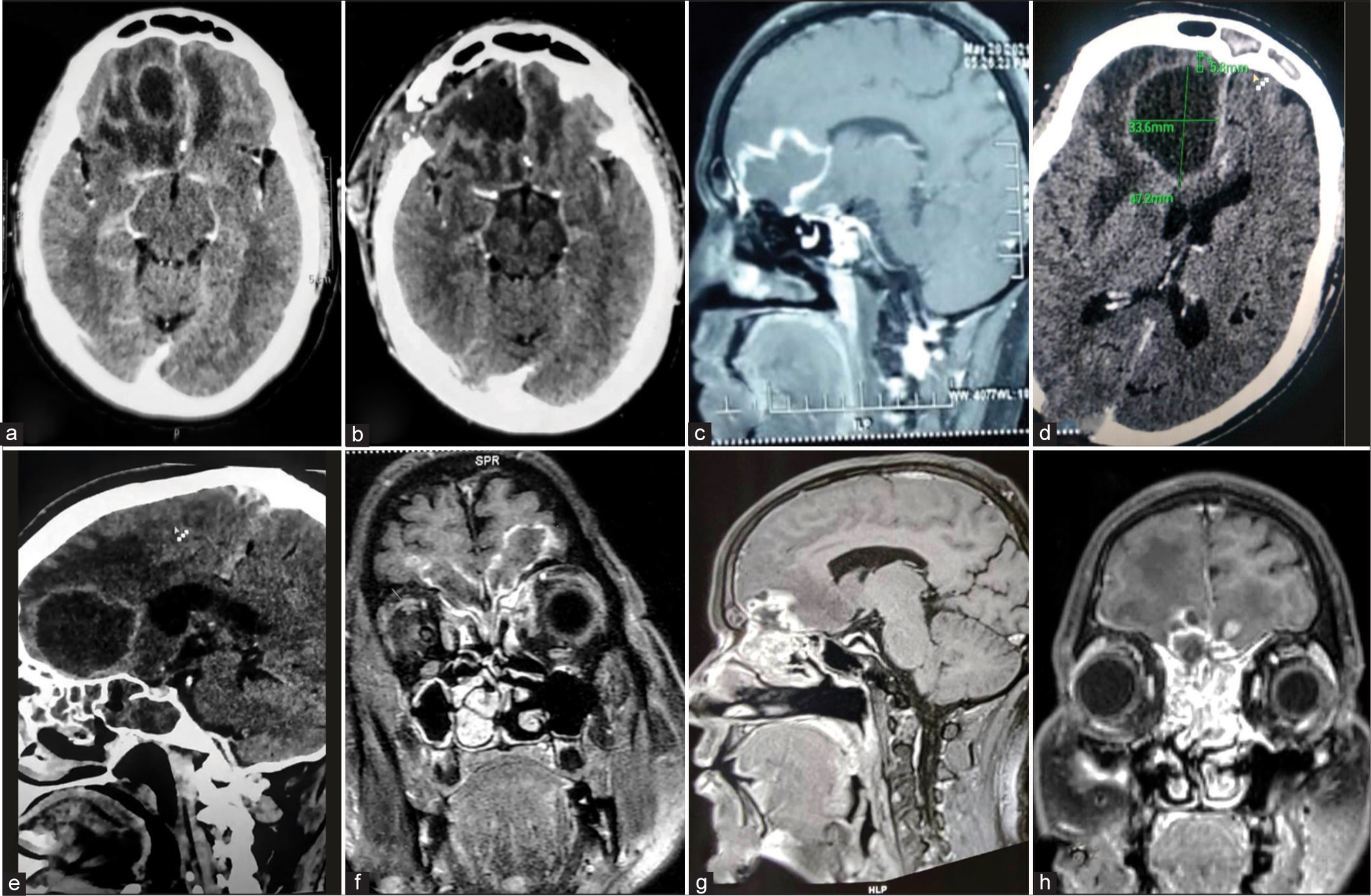
We conducted a prospective observational study of all patients admitted to our institute with a diagnosis of RCM after obtaining ethical clearance from the Institutional Review Board vide letter no. OW/RC/All India Institute of Medical Sciences – Raipur/2021/576 dated June 8, 2021. All patient files with a final diagnosis of RCM were thoroughly analyzed in departmental records and a master chart was prepared [
No disease – No contrast-enhancing lesion Static disease – Contrast enhancement is present but less than in the preoperative scans Progressive disease – Contrast enhancement is present which is more than in the pre-operative scans.
Data analysis was performed using the Statistical Package for the Social Sciences version 25:0 (International Business Machines Corporation, New York, United States of America).
RESULTS
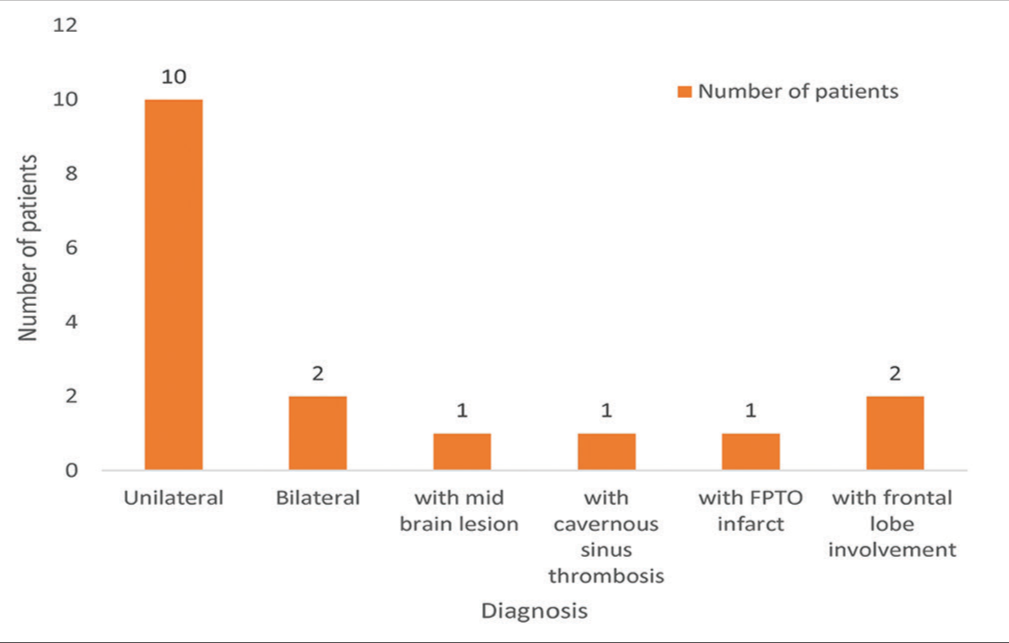
We analyzed all 251 cases of mucormycosis admitted with us to date and identified the 61 cases which had cerebral involvement. The first case of mucormycosis was presented to us on the May 2, 2021. Out of the 61 cases of RCM, 57 cases had a past history of COVID infection (93.4%). Out of these 57 cases, 52 patients had received steroids for the treatment of COVID in the past (85.2%). Fifty-seven out of the 61 cases of RCM were diabetic (93.4%). The most common presentation of RCM was temporal lobe abscess (25.7%) [
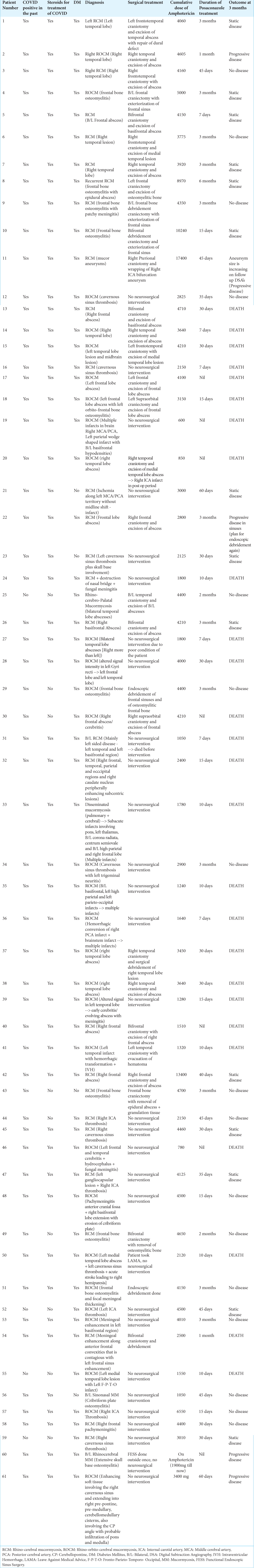
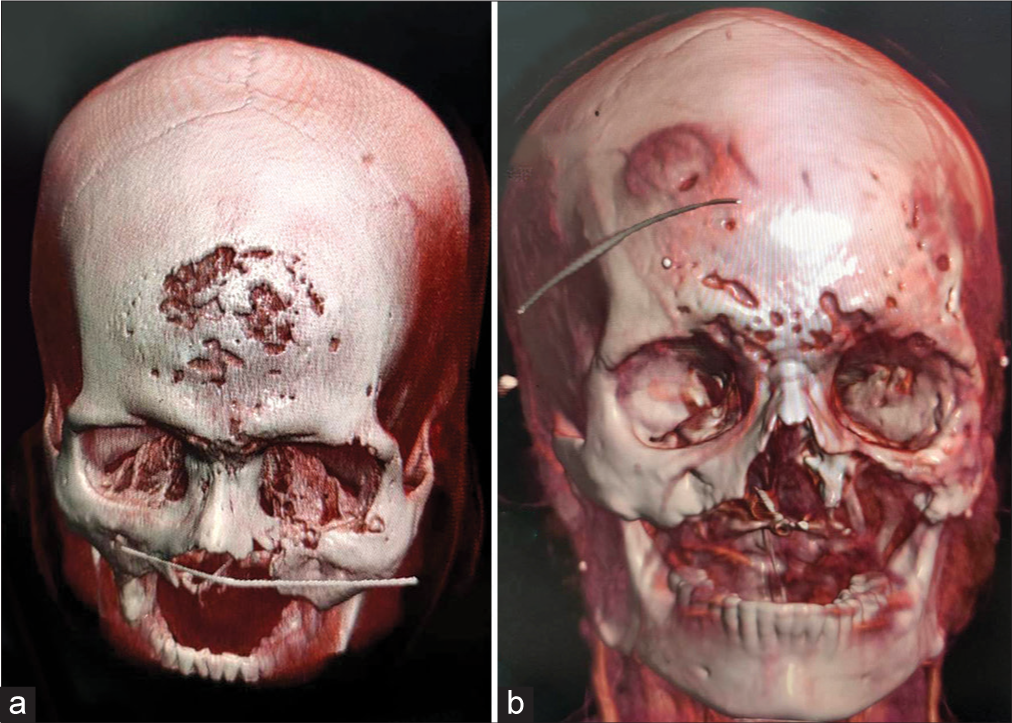
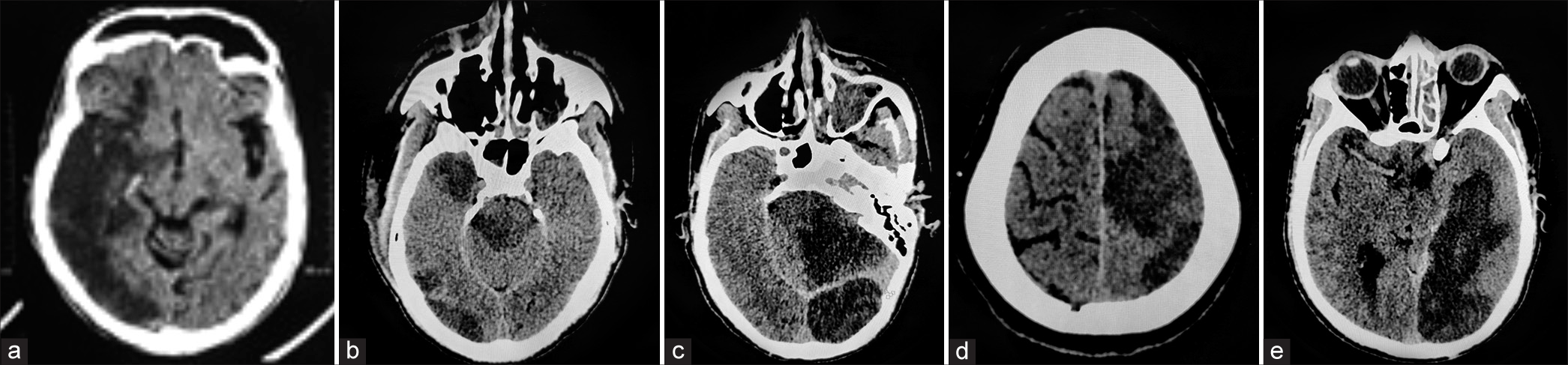
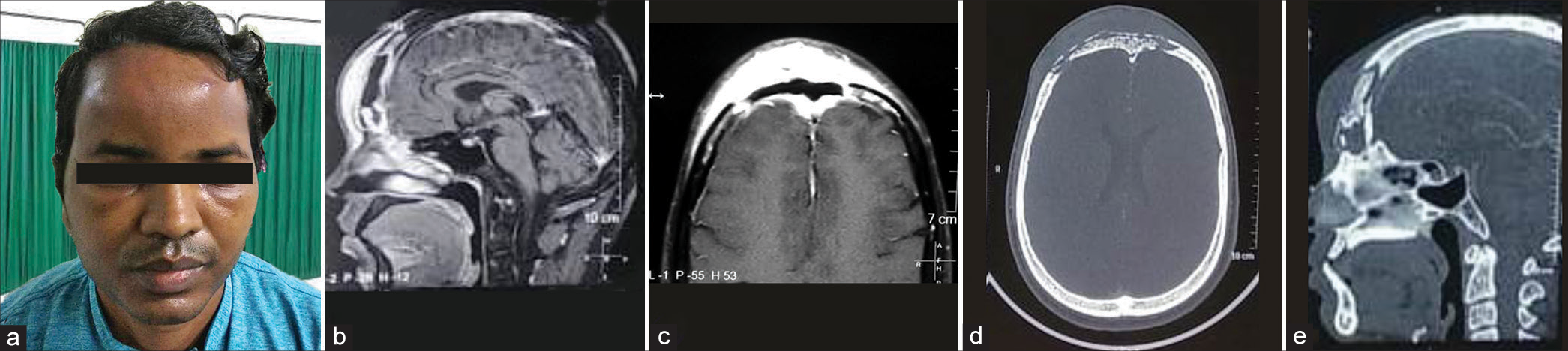
Figure 1:
(a and b) Preoperative and postoperative computed tomography (CT) scan images of the brain showing complete excision of bilateral temporal lobe abscesses. (c) CT scan image of the brain depicting left medial temporal lobe abscess. (d and e) In a case of rhino-orbito-cerebral mucormycosis (ROCM) with radiology which is suggestive of the involvement of all sinuses (pansinusitis), in the brain, a lesion is seen involving the right cavernous sinus and right medial temporal lobe with extension into the right cerebellopontine angle.
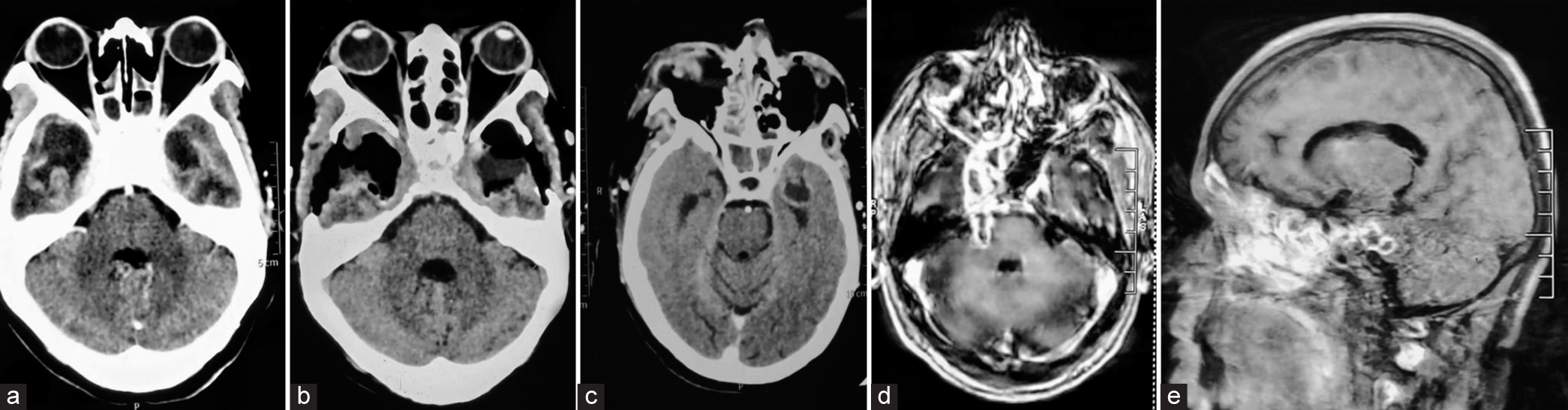
Figure 2:
(a-c) A case of rhino-cerebral mucormycosis (RCM) with the right frontal lobe abscess who underwent right frontal craniotomy and excision of abscess, along with combined (open plus endoscopic) debridement of sinuses. (d) Immediate postoperative computed tomography (CT) scan images showing complete excision of the abscess. (e) Postoperative contrast-enhanced CT (CECT) scan images at 3 months follow-up showing no residual lesion.
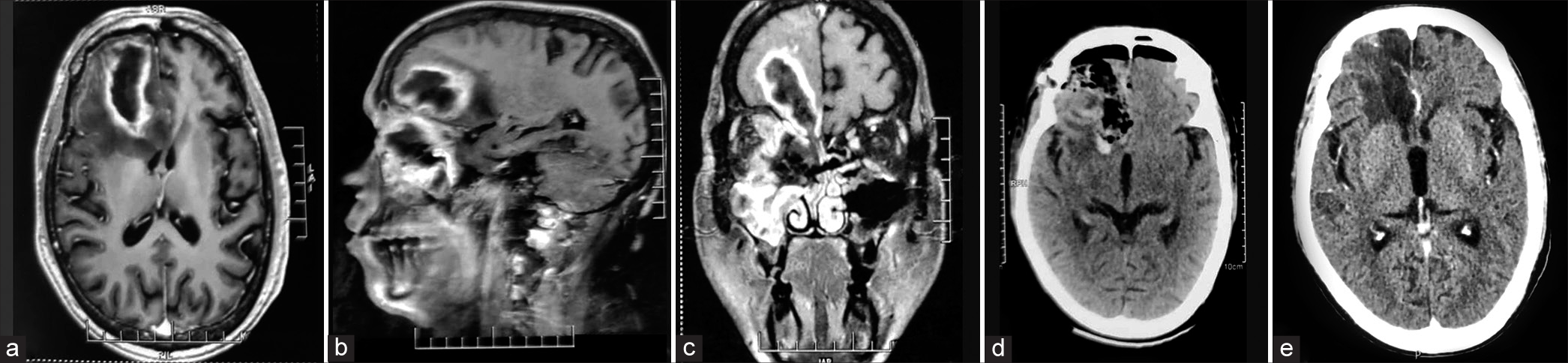
Figure 3:
(a and b) Preoperative and postoperative contrast-enhanced computed tomography (CECT) images of the brain showing complete excision of the right frontal lobe abscess. (c-e) Rhinocerebral mucormycosis (RCM) cases presented as huge unilateral frontal lobe abscesses. (f-h) Cases of RCM with bilateral basifrontal extension of the lesion through the cribriform plate.
Figure 10:
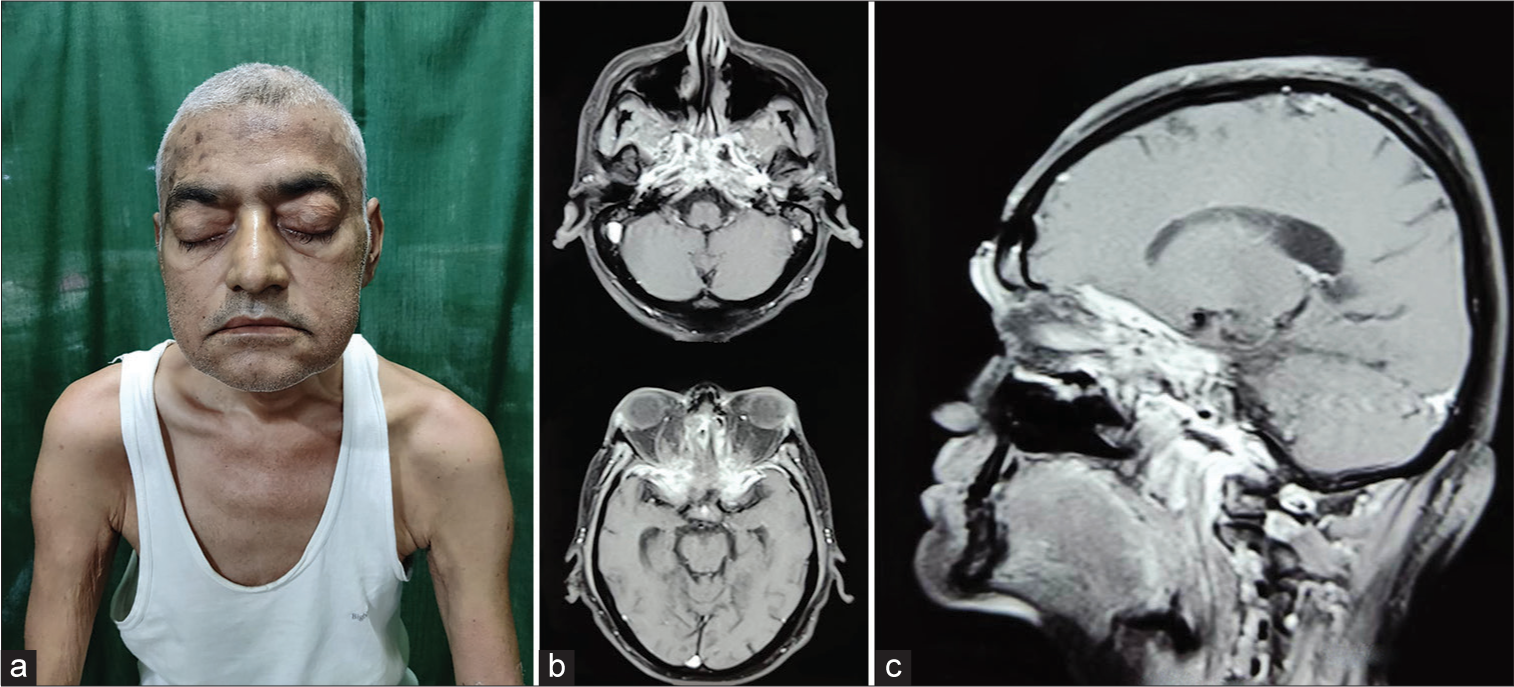
(a) Clinical photograph of a patient with bilateral Rhino-orbito-cerebral mucormycosis (ROCM) with extensive skull base osteomyelitis with multiple cranial nerve palsies bilaterally. (b and c) Radiology was suggestive of bilateral ethmoid sinusitis with involvement of bilateral infratemporal fossae, pterygopalatine fossae, inferior orbital fissure, superior orbital fissure, orbital apex, and bilateral cavernous sinuses with pachymeningitis. There was an erosion of the clivus, occipital condyles, basisphenoid, and anterior skull base.
CASE ILLUSTRATIONS
Case 1
A 52-year-old male patient presented with bilateral multiple cranial nerve palsies. On examination, he had bilateral perception of light (PL) negative, bilateral ptosis, bilateral restriction of eyeball movements, bilateral facial palsy, bilateral corneal reflex absent, gag reduced, presence of tongue fasciculations, and left vocal cord palsy. Radiology was suggestive of extensive skull base osteomyelitis [
Case 2
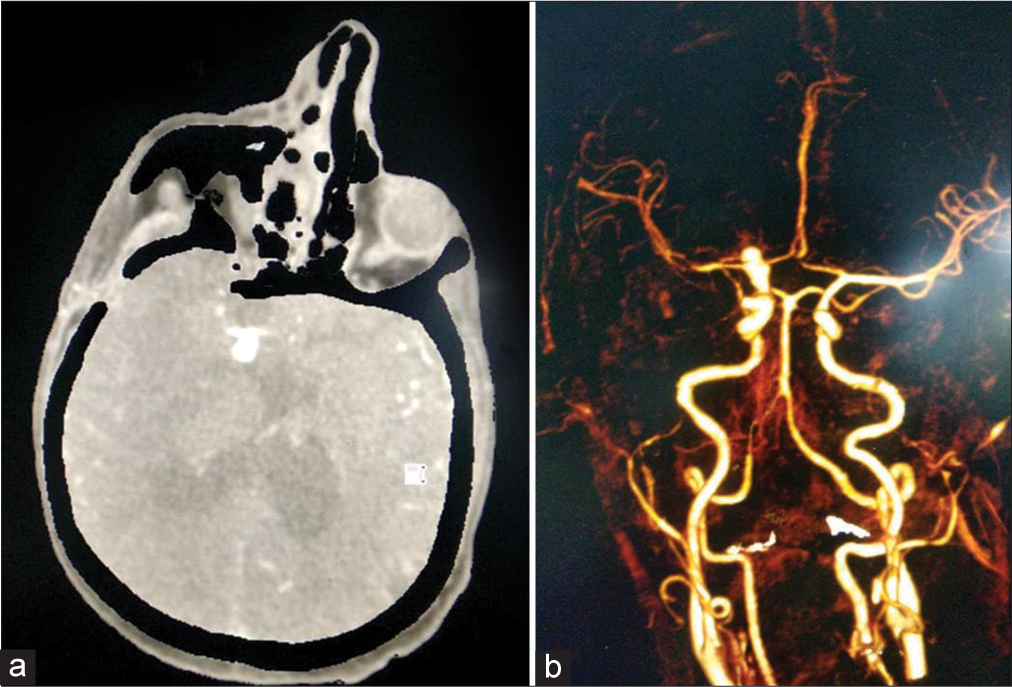
A 53-year-old male presented with sudden onset of left upper and lower limb weakness along with drowsiness. Non-contrast CT scan was suggestive of subarachnoid hemorrhage. CT angiography of the brain showed a right ICA bifurcation aneurysm [
Case 3
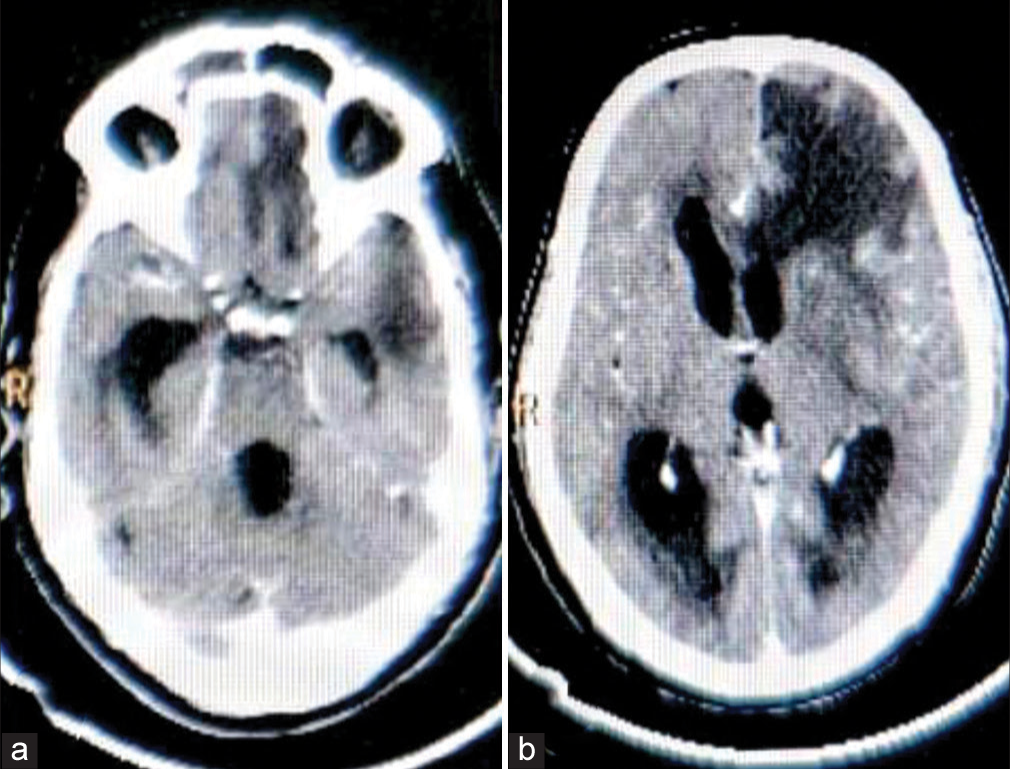
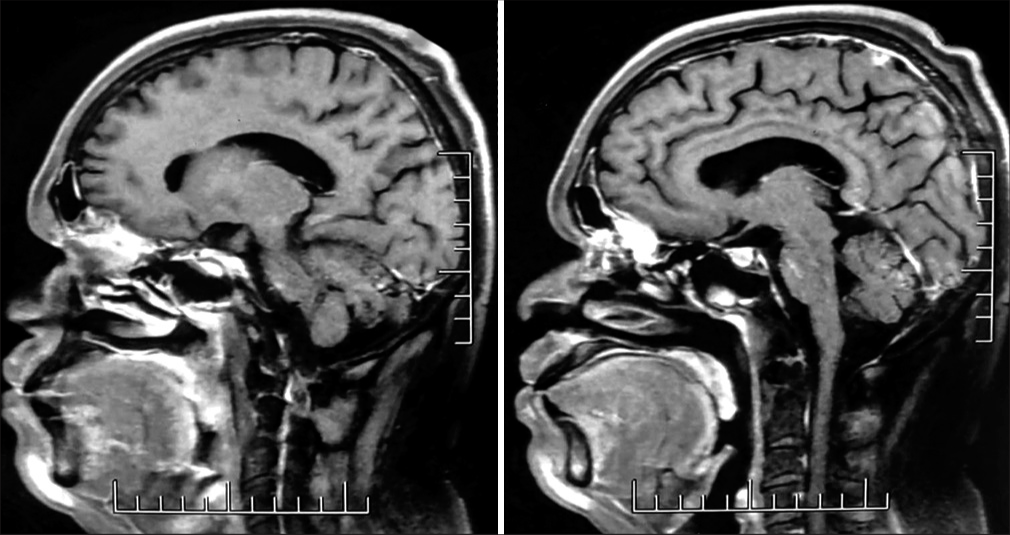
A 45-year-old female presented with purulent discharge from bilateral nostrils with headache and fever. She was diagnosed with post-COVID rhino-cerebro-palatal mucormycosis with bilateral temporal lobe abscesses [
Case 4
A 41-year-old male presented with right hemifacial pain, right eye swelling, and right-sided headache. He was diagnosed with post-COVID rhino-orbito-cerebral mucormycosis (ROCM) with a huge right frontal abscess. He underwent right frontal craniotomy and excision of abscess followed by debridement of the sinuses through combined approach (endoscopic and open). In the postoperative period, he received a cumulative amphotericin B dose of 8400 mg and also took oral posaconazole for 3 months. At 3 months follow-up, he had no fresh complaints and radiology was suggestive of no residual or recurrent disease [
Case 5
A 33-year-old male patient presented to us with swelling over the forehead and periorbital region. He was diagnosed case of post-COVID mucormycosis. He had undergone endoscopic debridement of sinuses for the same. His radiology was suggestive of frontal bone osteomyelitis with pachymeningitis with epidural and subgaleal abscesses [
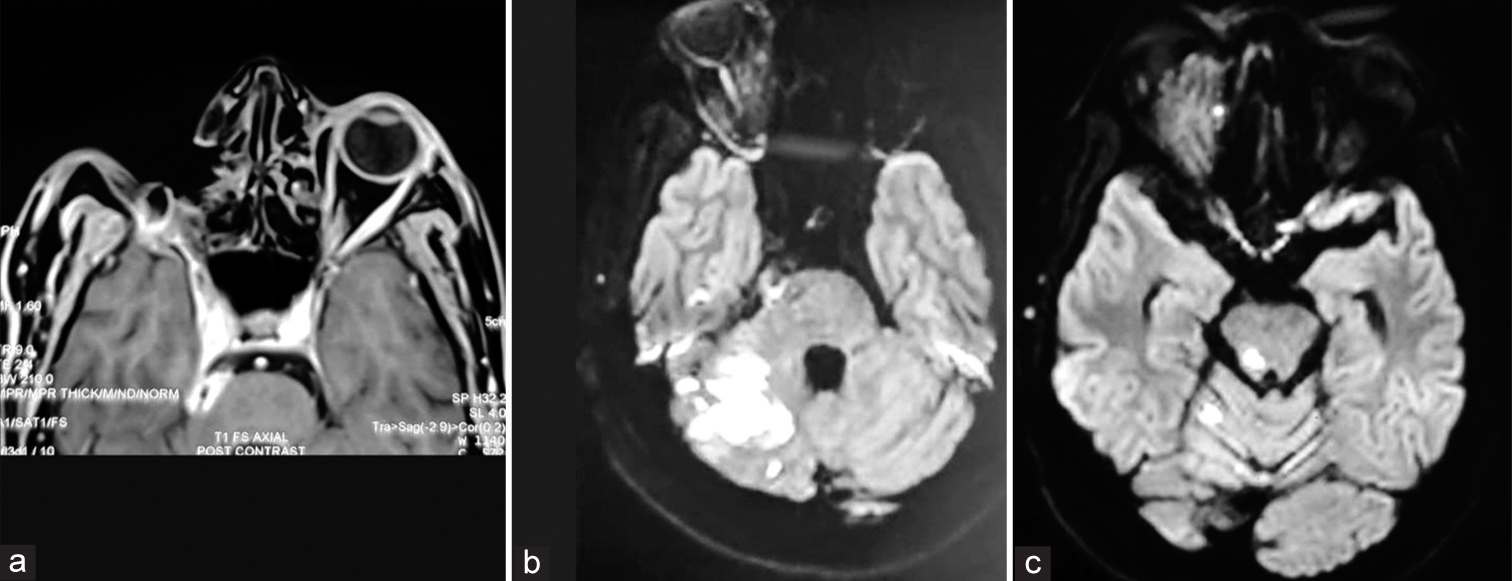
Case 6
A 44-year-old male patient presented to us with pus discharge from the right eye exenterated site. He was diagnosed case of post-COVID mucormycosis, for which he had undergone debridement of sinuses through combined approach (open + endoscopic), along with right orbital exenteration (right eye perception of light negative). He received a total dose of 3400 mg of amphotericin B and also took oral posaconazole for 2 months. At 3 months follow-up, his radiology was suggestive of progressive disease in the right cavernous sinus with extension into right pre-pontine, pre-medullary, and cerebellopontine angle cisterns. Diffusion-weighted images showed increased signal intensity in the right hemicerebellum, right brachium pontis, and the right lateral aspect of pons suggestive of an infarct. We have started him on a medical line of management (Amphotericin B and posaconazole) [
Figure 18:
(a) An operated case of right rhino-orbito-cerebral mucormycosis (ROCM) with progressive disease in the right cavernous sinus with extension into right pre-pontine, pre-medullary, and cerebellopontine angle cisterns as seen on magnetic resonance images of the brain taken 3 months post-surgery. (b and c) Diffusion-weighted images (DWI) of the same patient showed increased signal intensity in the right hemicerebellum, right brachium pontis, and the right lateral aspect of pons suggestive of an infarct.
Case 7
A 56-year-old male patient presented to us with the left-sided headache, left eye proptosis, restriction of all left eyeball movements, left eye ptosis, conjunctival chemosis, double vision, and cough with expectoration. He was diagnosed with ROCM with pulmonary involvement. He had no past history of Coronavirus Disease 2019 (COVID-19) infection. He had also received the first dose of COVID vaccination (Covishield). His radiology was suggestive of pansinusitis with the left orbital cellulitis and left CST. He also had multiple nodular lesions in both lungs, predominantly in the upper lobes with cavitary changes and halo sign, likely pulmonary mucormycosis. He underwent debridement of sinuses through a combined approach (open plus endoscopic) and medial orbitotomy. He had received a cumulative dose of amphotericin B of 1050 mg but succumbed to his illness and died on postoperative day 3.
Case 8
A 67-year-old female presented to us with complaints of headache, swelling of the left eye, decreased vision in both eyes (the left eye was affected first followed by the right eye), left conjunctival chemosis, and restriction of all movements of the left eye. She was diagnosed with post-COVID bilateral ROCM [
Case 9
A 48-year-old male presented to us with the right nasal discharge, right nasal stuffiness, and right visual loss. He was diagnosed as a case of post-COVID ROCM with cribriform plate osteomyelitis. Radiology was suggestive of pansinusitis, right orbital cellulitis (right eye perception of light negative) and pachymeningitis in the anterior cranial fossa with an erosion of the right cribriform plate [
Case 10
A 44-year-old male patient presented to us in a comatose state (M2 motor response according to Glasgow Coma Scale). He was diagnosed case of post-COVID disseminated mucormycosis. Non-contrast CT scan of the brain was suggestive of multiple infarcts involving the right side of the pons, left thalamus, centrum semiovale, bilateral high parietal lobes, and right frontal lobe. He was started on a medical line of management but succumbed to his illness.
DISCUSSION
Mucormycosis is a rapidly progressing infection caused by the angioinvasive fungi in the order of Mucorales.[
Mohindra et al., in his paper, reported ten cases of mucormycosis with intracranial extension in the form of CST (3), intracranial masses (3), brain abscesses (2), and ischemic infarcts (2).[
Patel et al., in their paper, have reported 187 cases of COVID-19 associated mucormycosis (CAM) of which 44 patients had rhino-orbito-cerebral involvement.[
In our study also, 93.4% of the RCM cases had a past history of COVID infection and were diabetic and 85.2% of cases had received steroids for the treatment of COVID-19 infection in the past. The overall mortality in our study was 42.6%.
CONCLUSION
We report the largest single-center case series of RCM, comprising 61 patients. This case series underscores the importance of the early diagnosis and prompt treatment for a better prognosis for this dreadful disease. The three pillars of treatment for RCM cases include reversal of the immunosuppressive state, administration of antifungal drugs, and extensive surgical debridement. In spite of all this, mortality remains high.
Declaration of patient consent
The Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ajith Kumar AK, Gupta V, editors. Rhino-orbital cerebral mucormycosis. StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. p.
2. Bakshi SS, Das S, Ramesh S, Gopalakrishnan S. Nasal mucormycosis: Our experience with 24 cases. Otolaryngol Pol. 2020. 74: 37-40
3. Balai E, Mummadi S, Jolly K, Darr A, Aldeerawi H. Rhinocerebral mucormycosis: A ten-year single centre case series. Cureus. 2020. 12: e11776
4. Bennett JE, Dolin R, Blaser MJ, editors. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases E-Book. Netherlands: Elsevier Health Sciences; 2019. p.
5. Hosseini SM, Borghei P. Rhinocerebral mucormycosis: Pathways of spread. Eur Arch Otorhinolaryngol. 2005. 262: 932-8
6. Kantarcioglu AS, Turgut M, Challa S, Akhaddar A, editors. Mucormycosis. Fungal Infections of the Central Nervous System. Champaign: Springer; 2019. p.
7. Mehta R, Nagarkar NM, Jindal A, Rao KN, Nidhin SB, Arora RD. Multidisciplinary management of COVID-associated mucormycosis syndemic in India. Indian J Surg. 2022. 84: 934-42
8. Mohindra S, Mohindra S, Gupta R, Bakshi J, Gupta SK. Rhinocerebral mucormycosis: The disease spectrum in 27 patients. Mycoses. 2007. 50: 290-6
9. Patel A, Agarwal R, Rudramurthy SM, Shevkani M, Xess I, Sharma R. Multicenter epidemiologic study of coronavirus disease-associated mucormycosis, India. Emerg Infect Dis. 2021. 27: 2349-59
10. Roushdy T, Hamid E. A case series of post COVID-19 mucormycosis-a neurological prospective. Egypt J Neurol Psychiatr Neurosurg. 2021. 57: 100