- Department of Neurological Surgery, Nippon Medical School Hospital, Bunkyo-ku, Tokyo,
- Department of Neurosurgery, Yokohama Shin-Midori General Hospital, Yokohama, Kanagawa,
- Department of Neurosurgery, The Jikei University School of Medicine, Minato-ku, Tokyo, Japan.
Correspondence Address:
Toshiki Nozaki
Department of Neurological Surgery, Nippon Medical School Hospital, Bunkyo-ku, Tokyo,
DOI:10.25259/SNI_789_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Toshiki Nozaki1,2, Masayuki Noda2, Toshihiro Ishibashi3, Akio Morita1. Ruptured hidden intracranial aneurysm during mechanical thrombectomy: A case report. 16-Dec-2020;11:446
How to cite this URL: Toshiki Nozaki1,2, Masayuki Noda2, Toshihiro Ishibashi3, Akio Morita1. Ruptured hidden intracranial aneurysm during mechanical thrombectomy: A case report. 16-Dec-2020;11:446. Available from: https://surgicalneurologyint.com/surgicalint-articles/10455/
Abstract
Background: Acute ischemic stroke (AIS) patients have a higher prevalence of cerebral aneurysm than a healthy reference population. However, it was recently reported that cases of an unknown hidden aneurysm in AIS patients with large-vessel occlusion are rare. We report a rare case of subarachnoid hemorrhage (SAH) during mechanical thrombectomy (MT) using a stent retriever for AIS.
Case Description: A 46-year-old patient with the right internal carotid artery terminal occlusion presented with the left-sided hemiparesis, hemispatial neglect, and dysarthria and underwent MT. Initial thrombectomy using a stent retriever and reperfusion catheter was unsuccessful. Angiography just before the second attempt showed SAH. Fortunately, we achieved recanalization of the thrombolysis in cerebral infarction 2b and hemostasis by lowering the blood pressure followed by coil embolization of the ruptured aneurysm. Only a few cases of ruptured aneurysms have been reported during MT using a stent retriever. Stent withdrawal is suspected to cause aneurysm rupture in cases with an unknown hidden middle cerebral artery bifurcation aneurysm.
Conclusion: Preinterventional detection of a hidden aneurysm is difficult. Therefore, surgeons must always consider the possibility of a hidden aneurysm rupture in vessels distal to the occlusion site and make adequate preparations for the prompt treatment of ruptured aneurysms after MT.
Keywords: Aneurysm, Ischemic stroke, Stent retriever, Subarachnoid hemorrhage, Thrombectomy
INTRODUCTION
Patients with cerebral aneurysm suffering from acute ischemic stroke (AIS) were found to have a prevalence of 5.6% according to a recent study (in a population of 127 AIS patients), which was higher than the worldwide prevalence, calculated in healthy reference populations (from over 20 countries with no comorbidities and an average age of 50 years).[
CASE DESCRIPTION
A 46-year-old female presented with the left-sided hemiparesis, hemispatial neglect, and dysarthria (National Institutes of Health Stroke Scale [NIHSS] score, 11). Right intracranial internal carotid artery (ICA) occlusion was suspected based on magnetic resonance angiography (MRA) at 343 min from the onset of these symptoms. We did not, however, detect a cerebral aneurysm on MRA. The patient was not eligible for IV tPA therapy due to the time constraints and subsequently received endovascular therapy by MT under local anesthesia.
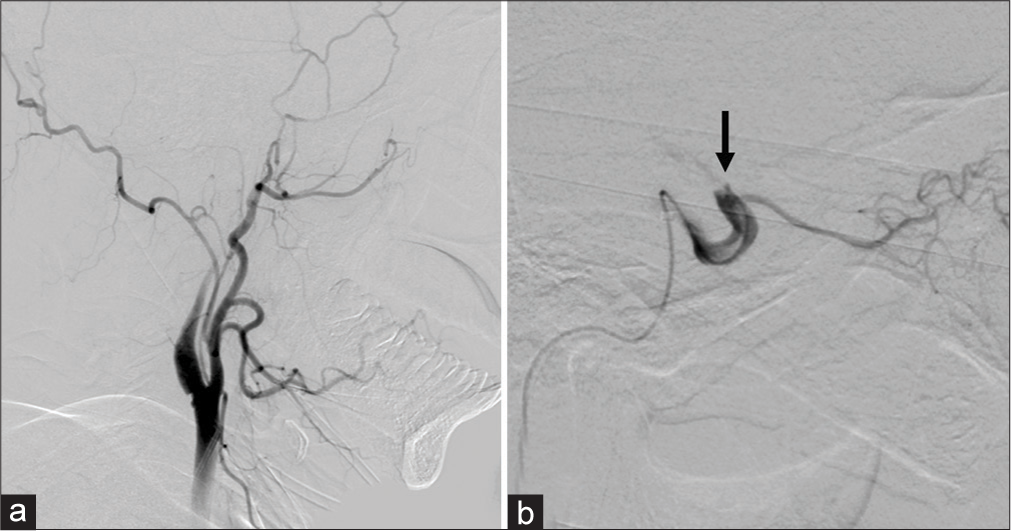
Conventional angiography revealed terminal occlusion of the ICA [
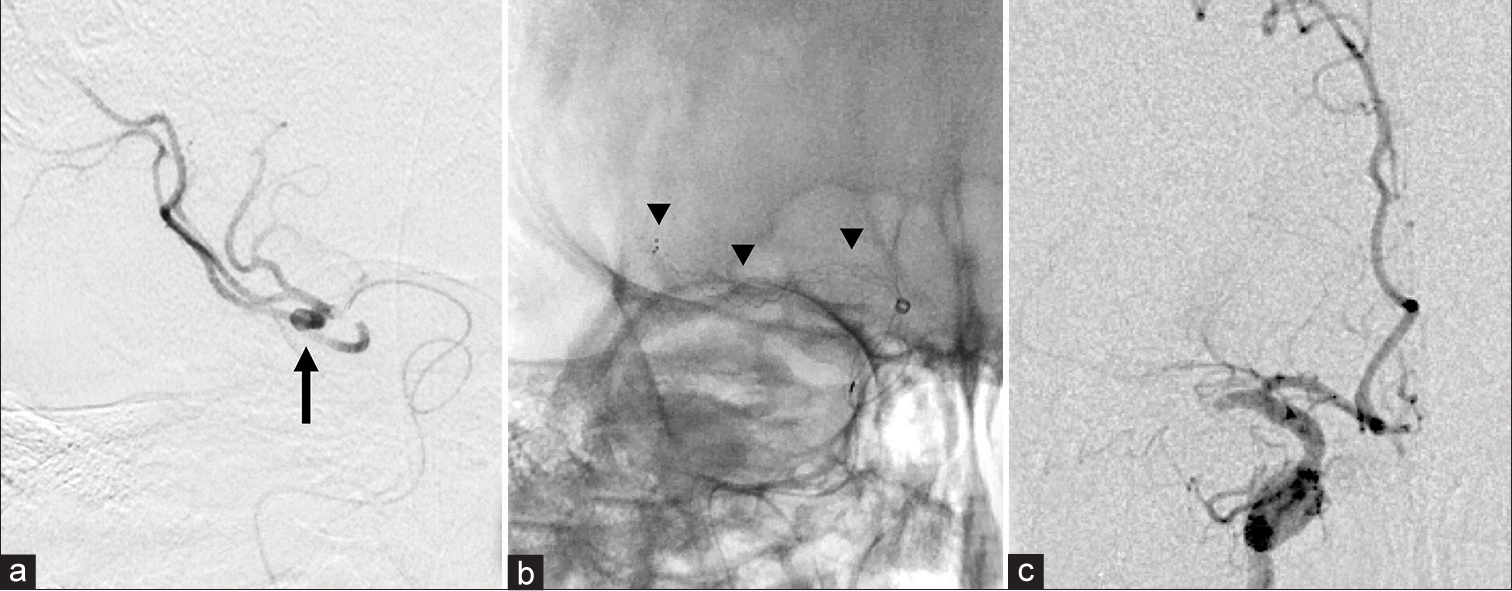
Figure 2:
(a) Contrast injection through microcatheter-guided distal to the occlusion site depicted a middle cerebral artery (MCA) bifurcation aneurysm. The black arrow indicates the aneurysm. (b) The stent retriever is deployed from the MCA M2 segment proximal to the internal carotid artery terminal (ICA-T), and the reperfusion catheter is placed at the ICA-T. The arrowheads show the stent retriever. (c) Angiography performed after the first attempt showing persistence of the MCA M1 proximal occlusion.
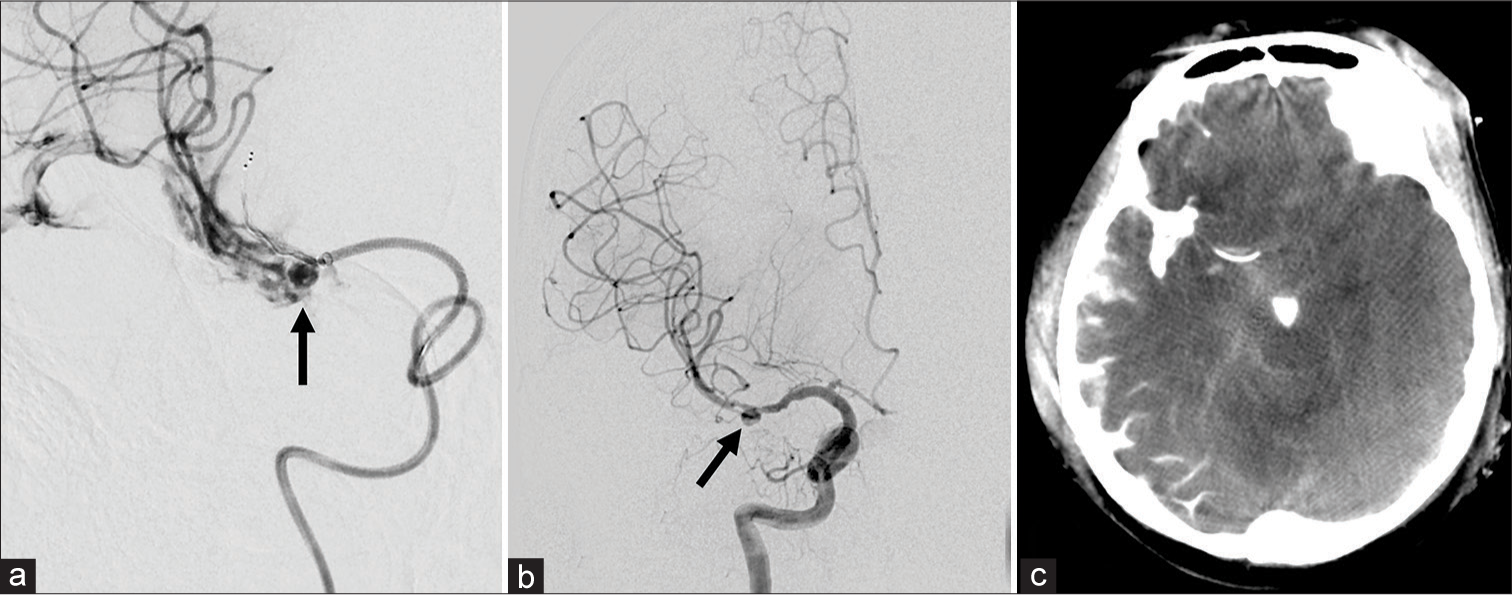
Figure 3:
(a) Angiography performed immediately before the second mechanical thrombectomy (MT) showing subarachnoid hemorrhage around the middle cerebral artery aneurysm. (b) Angiography performed after the second MT showing recanalization of the thrombolysis in the cerebral infarction 2b and hemostasis achievement. (c) Subarachnoid hemorrhage and extravasated contrast medium as seen on flat-panel detector computed tomography.
DISCUSSION
There are few reports about the prevalence of aneurysms in AIS patients who underwent MT[
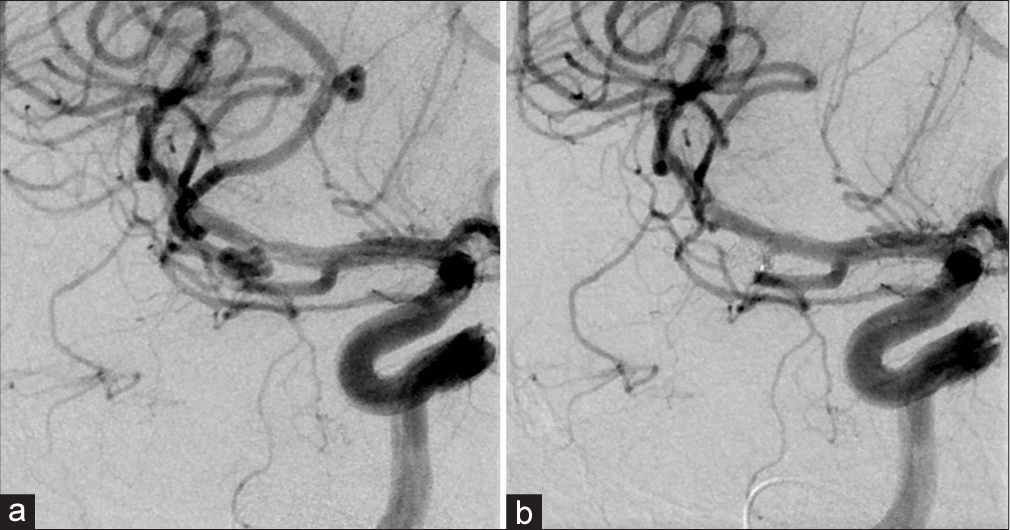
In our case, the rupture of the aneurysm was possibly caused by the withdrawal of the first stent or by the microguidewire manipulation until the second stent was deployed. By checking the recorded video of the operation, we confirmed that the microguidewire moved smoothly and seemed to keep the correct intra-arterial positioning. Only a few cases of ruptured aneurysms during MT using a stent retriever have been reported.[
It is concerning to note that there is no clear procedure to manage the rupture of a hidden aneurysm at vessels distal to the occlusion site (those that have not been recanalized). As reported by Zihold et al.,[
Preinterventional detection of a hidden aneurysm is difficult. It has been reported that the vasculature distal to the occlusion site can be detected by contrast-enhanced FDCT in the angiography suite.[
CONCLUSION
We must consider the possibility of a hidden aneurysm rupture in vessels distal to the occlusion site that has not been recanalized, and accordingly, preparation for the prompt treatment of that ruptured aneurysm after MT is necessary. In this case, had the aneurysm distal to the occlusion site been identified before MT, a safer therapy, an alternative to the MT method, might have been warranted.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Asai K, Nakamura H, Sakaguchi M, Kawano T, Ozaki T, Ima H. Direct aspiration first pass technique for a middle cerebral artery occlusion with a hidden aneurysm. Interv Neuroradiol. 2015. 21: 700-2
2. Blanc R, Pistocchi S, Babic D, Bartolini B, Obadia M, Alamowitch S. Intravenous flat-detector CT angiography in acute ischemic stroke management. Neuroradiology. 2012. 54: 383-91
3. Horiuchi T, Nitta J, Miyaoka Y, Nagm A, Tsutsumi K, Ito K. Open embolectomy of large vessel occlusion in the endovascular era: Results of a 12-year single-center experience. World Neurosurg. 2017. 102: 65-71
4. Singh J, Wolfe SQ. Stent retriever thrombectomy with aneurysm in target vessel: Technical note. Interv Neuroradiol. 2016. 22: 544-7
5. Suzuki M, Mizunari T, Iwamoto N, Morita A. Embolectomy through aneurysm wall for iatrogenic occlusion of M1 portion during coil embolization: Technical note for transaneurysmal embolectomy. World Neurosurg. 2018. 114: 113-6
6. Turk AS, Turner R, Spiotta A, Vargas J, Holmstedt C, Ozark S. Comparison of endovascular treatment approaches for acute ischemic stroke: Cost effectiveness, technical success, and clinical outcomes. J Neurointerv Surg. 2015. 7: 666-70
7. Vlak MH, Algra A, Brandenburg R, Rinkel GJ. Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period : A systematic review and meta-analysis. Lancet Neurol. 2011. 10: 626-36
8. Zeleňák K, Vorčák M, Sýkora J, Trabalková Z, Zeleňáková J, Kantorová E. Management of ruptured hidden mirror intracranial aneurysm during mechanical thrombectomy. Interdiscip Neurosurg. 2019. 17: 60-3
9. Zhou T, Li T, Zhu L, Wang Z, Bai W, Xue J. Endovascular thrombectomy for large-vessel occlusion strokes with preexisting intracranial aneurysms. Cardiovasc Interv Radiol. 2018. 41: 1399-403
10. Zibold F, Kleine JF, Zimmer C, Poppert H, Boeckh-Behrens T. Aneurysms in the target vessels of stroke patients subjected to mechanical thrombectomy: Prevalence and impact on treatment. J Neurointerv Surg. 2016. 8: 1016-20