- Department of Neurosurgery, Prasat Neurological Institute, Bangkok, Thailand.
- Department of Neuroradiology, Prasat Neurological Institute, Bangkok, Thailand.
- Department of Pathology, Prasat Neurological Institute, Bangkok, Thailand.
- Department of Radiology, Bumrungrad International Hospital, Bangkok, Thailand.
Correspondence Address:
Prasert Iampreechakul, Department of Neurosurgery, Prasat Neurological Institute, Bangkok, Thailand.
DOI:10.25259/SNI_980_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Prasert Iampreechakul1, Korrapakc Wangtanaphat1, Chonlada Angsusing2, Yodkhwan Wattanasen2, Punjama Lertbutsayanukul2, Samasuk Thammachantha3, Somkiet Siriwimonmas4. Sacral dural arteriovenous fistula of the filum terminale coexisting with partially thrombosed filum vein: A case report and literature review. 04-Mar-2022;13:78
How to cite this URL: Prasert Iampreechakul1, Korrapakc Wangtanaphat1, Chonlada Angsusing2, Yodkhwan Wattanasen2, Punjama Lertbutsayanukul2, Samasuk Thammachantha3, Somkiet Siriwimonmas4. Sacral dural arteriovenous fistula of the filum terminale coexisting with partially thrombosed filum vein: A case report and literature review. 04-Mar-2022;13:78. Available from: https://surgicalneurologyint.com/surgicalint-articles/11422/
Abstract
Background: Filum terminale arteriovenous fistulas (FTAVFs) are rare and usually classified as intradural ventral AVFs or Type IVa perimedullary fistulas, located on the pia surface along the course of filum terminale internum (FTI). We report an extremely rare case of sacral dural arteriovenous fistula of the FT. We also review the occurrence of FTAVFs in the sacral region.
Case Description: A 64-year-old man presented with progressive weakness of the lower extremities for 3 months and bowel/bladder dysfunction following long history of back pain radiating to both legs. Magnetic resonance imaging of the lumbosacral and thoracic spine showed spinal cord congestion, extending from the conus medullaris to the level of T3, and partial thrombosis within the abnormal tortuous and dilated flow void, running from the sacral area to conus medullaris. Further findings were compression fracture of L2 vertebra, Grade I degenerative spondylolisthesis at the level of L2-3, and L3-4, and spinal stenosis at L2-3, L3-4, and L4-5. Spinal angiography, maximum intensity projection reformatted image of angiographic computerized tomography, and three-dimensional reconstructed image clearly demonstrated dural AVF of the FT at the level of S2 supplied by bilateral lateral sacral and middle sacral arteries with cranial drainage to perimedullary vein through the enlarged vein of the filum. The patient was indirectly treated by transection of the filum terminale and the draining vein at the level of L5 rostral to the fistula.
Conclusion: Sacral DAVFs of the FT are extremely rare. In our case, the formation of fistula may cause by venous hypertension secondary to partial thrombosis within the filum vein, probably resulting from long-standing spinal canal stenosis. Sacral FTAVFs may be found on the pia surface of the terminal FTI, dural component at the area of dural sac termination, or dural extension covering the filum terminale externum.
Keywords: Fatty filum terminale, Filum terminale arteriovenous fistula, Filum terminale externum, Sacral dural arteriovenous fistula, Thrombosis of draining vein
INTRODUCTION
Filum terminale arteriovenous fistulas (FTAVFs), located below the conus medullaris along the course of the filum, are characterized by a single direct communication between the artery of the FT, distal termination of the anterior spinal artery (ASA), and the vein of the FT without intervening nidus.[
FTAVFs coexisting with spinal dysraphism, including tethered spinal cord and lipoma, may be found in the sacral region.[
We reported an extremely rare case of sacral DAVF of the FT coexisting with partially thrombosed filum vein. In addition, we reviewed the published case reports and series which have enough clinical description and clearly demonstrated figures of FTAVFs at the sacral region without spinal dysraphism.
CASE DESCRIPTION
A 64-year-old man was admitted to our institute due to a 3-month history of progressive paraparesis. Three years earlier, he experienced low back pain radiating to both legs, predominantly affecting the right side. He also had numbness in lower extremities, affecting the left more than right side. He was treated by medicine and physiotherapy at the local hospital. One month before the hospitalization, he was unable to walk without assistant. In addition, urine retention and constipation were noticed 2 weeks before admission. His back was injured by falling from a tree at a height of 3 m 4 years ago. The neurological examination revealed the evidence of spastic paraparesis (muscle strength 2/5), the lack of pinprick sensation below T10 level, hyperreflexia, and presence of Babinski sign in the lower extremities.
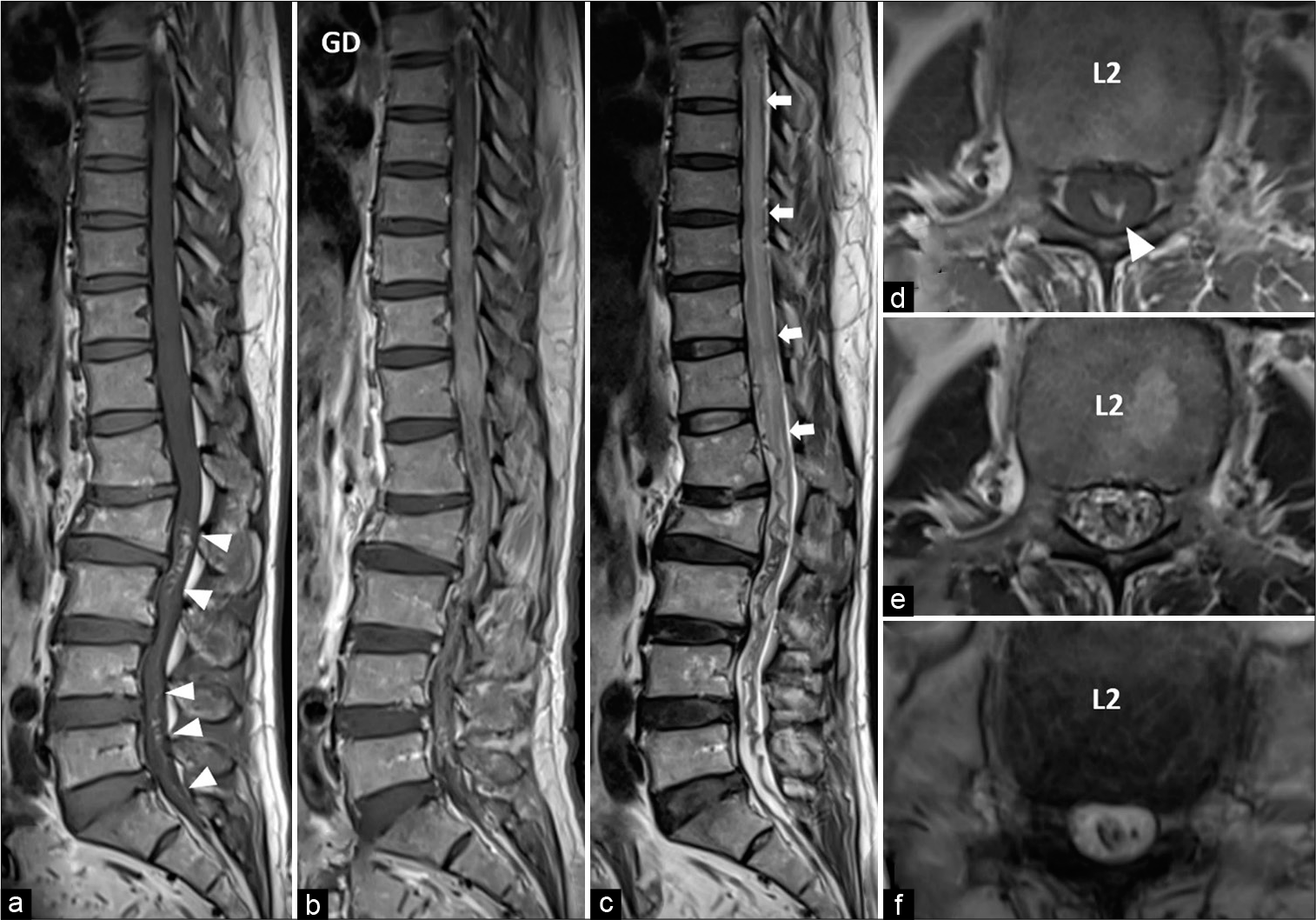
Magnetic resonance imaging (MRI) of the thoracolumbar spine showed hyperintense T1 signal, hypointense T2 signal with blooming on gradient-echo (GRE) T2*-weighted image in the abnormal flow void running from sacral level to the conus medullaris, probably representing subacute thrombosis. There were abnormal hyperintense T2 signal representing spinal cord congestion extending from the conus medullaris to the level of T3 and subtle perimedullary flow voids along the posterior surface of cord. After gadolinium contrast, diffuse enhancement of lower spinal cord and cauda equina nerve roots was observed [
Figure 1:
Preoperative magnetic resonance imaging of the thoracolumbar spine. Sagittal views of T1-weighted (a) without and (b) with gadolinium injection, (c) T2-weighted, and axial (d) T1-weighted, (e) T2-weighted, and (f) gradient-echo (GRE) T2*-weighted images at the level of L2 demonstrate hyperintense (arrowheads) T1 signal, hypointense T2 signal with blooming on GRE image in the flow void running from sacral level to the conus, probably representing subacute thrombosis. There is spinal cord congestion (arrows) extending from the conus to thoracic level. Enhancement of long segment spinal cord and cauda equina nerve roots are noted. Compression fracture of L2 vertebra is observed.
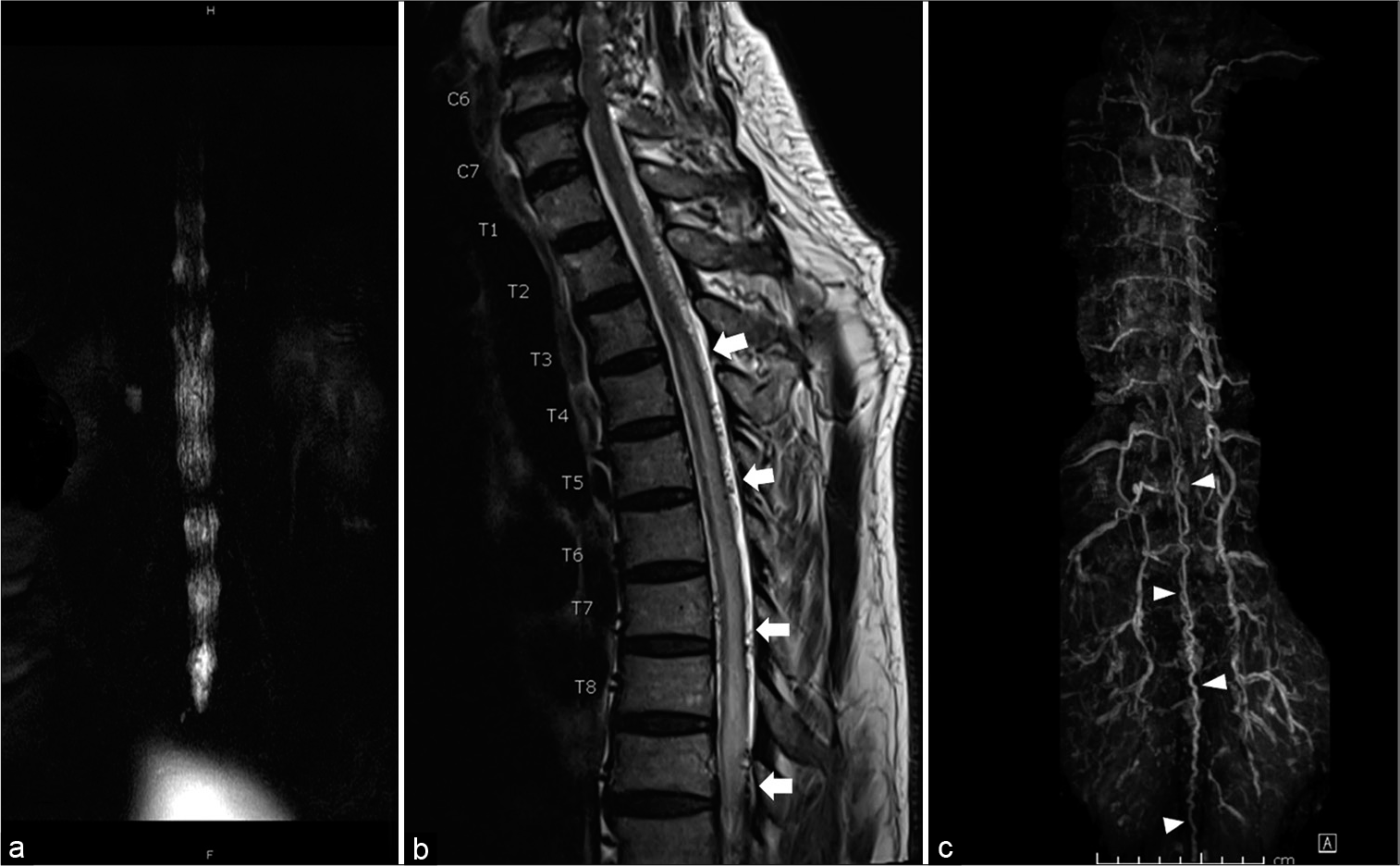
Figure 2:
(a) Coronal myelographic sequence reveals spinal canal stenosis corresponding with filling defect at the level of L2–3, L3-4, and L4–5. (b) Sagittal T2-weighted image of the cervicothoracic spine shows spinal cord congestion (arrows) extending up to T3 level and subtle intradural flow voids along the posterior surface of cord. (c) Contrast-enhanced magnetic resonance angiography of the thoracolumbar spine demonstrates tortuous and enlarged intradural vessels (arrowheads) in the midline location extending from the level of lower lumbar to thoracic level.
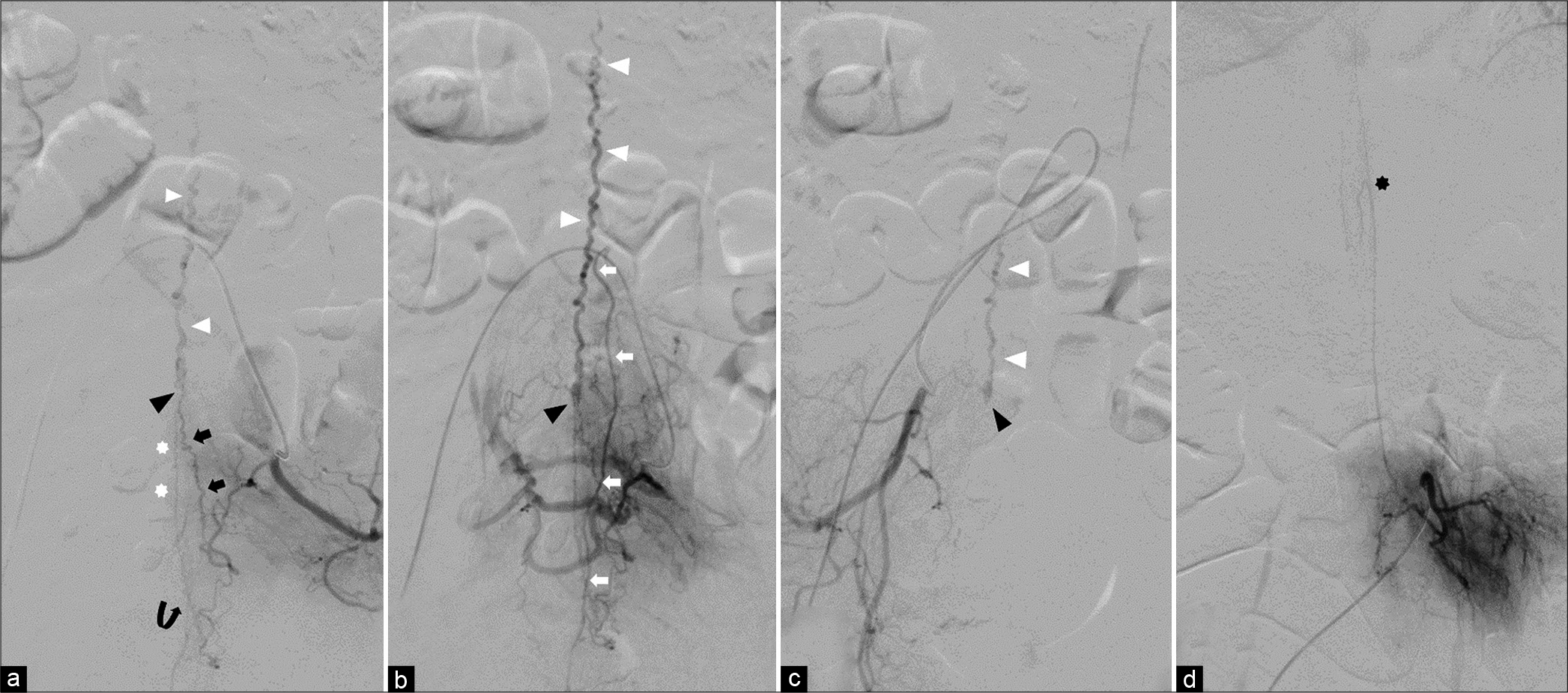
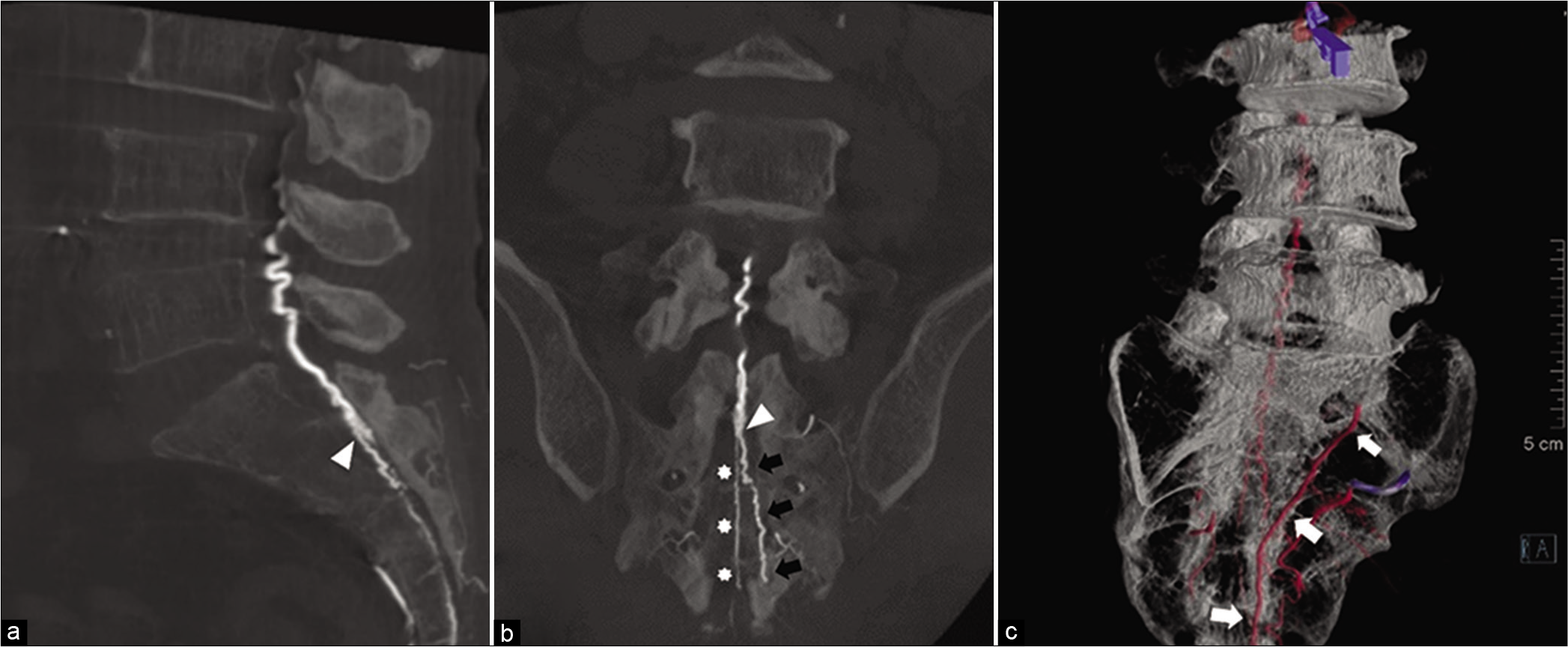
Spinal angiography demonstrated an AVF at the level of S2, which is supplied by the branches from bilateral lateral sacral arteries (LSA) with cranial drainage into the dilated vein of the FT. The middle sacral artery (MSA) anastomosing with the distal branch of left LSA was identified. The ASA arose from the left L3 segmental artery without supplying to the fistula. Maximum intensity projection (MIP) reformatted image of angiographic computerized tomography (CT) and three-dimensional reconstructed image clearly revealed the fistulous point at the level of S2. The fistula fed by two branches from the left LSA. One upper branch ran through the fourth sacral foramen. Another lower branch traveled through the sacral hiatus and then joins the straight artery along the filum terminale externum (FTE). The fistula was supplied by the right LSA through the right first sacral foramen [
Figure 3:
Preoperative spinal angiography. Arterial (a) and venous (b) phases of the left internal iliac artery injection show an arteriovenous fistula (black arrowheads) at the midline at the level of S2 supplied by the left lateral sacral artery (LSA) with cranial drainage into the dilated vein of the filum terminale (white arrowheads). There are two branches from the left LSA supplying to the fistula. One upper branch (black arrows) runs through the fourth sacral foramen. Another lower branch (curve arrow) travels through the sacral hiatus and then joins the straight artery (white asterisks) along the filum terminale externum. The middle sacral artery (white arrows) anastomosing with the distal branch of left LSA is identified. (c) The right internal iliac artery injection also reveals the same fistula (black arrowhead) with the dilated filum vein (white arrowheads) fed by the right LSA through the right first sacral foramen. (d) The left L3 segmental artery injection illustrates an anterior spinal artery with a characteristic hairpin turn (black asterisk).
Figure 4:
Sagittal (a) and coronal (b) maximum intensity projection reformatted images of angiographic computerized tomography of the left internal iliac artery clearly show the fistulous point (arrowheads) at the level of S2. The dural branch (black arrows) from the left lateral sacral artery runs through the left fourth sacral foramen and supplies to the fistula. Below the fistula, there is a straight artery (asterisks) run along the filum terminale externum at midline location. (c) Three-dimensional reconstructed image demonstrates the middle sacral artery (white arrows).
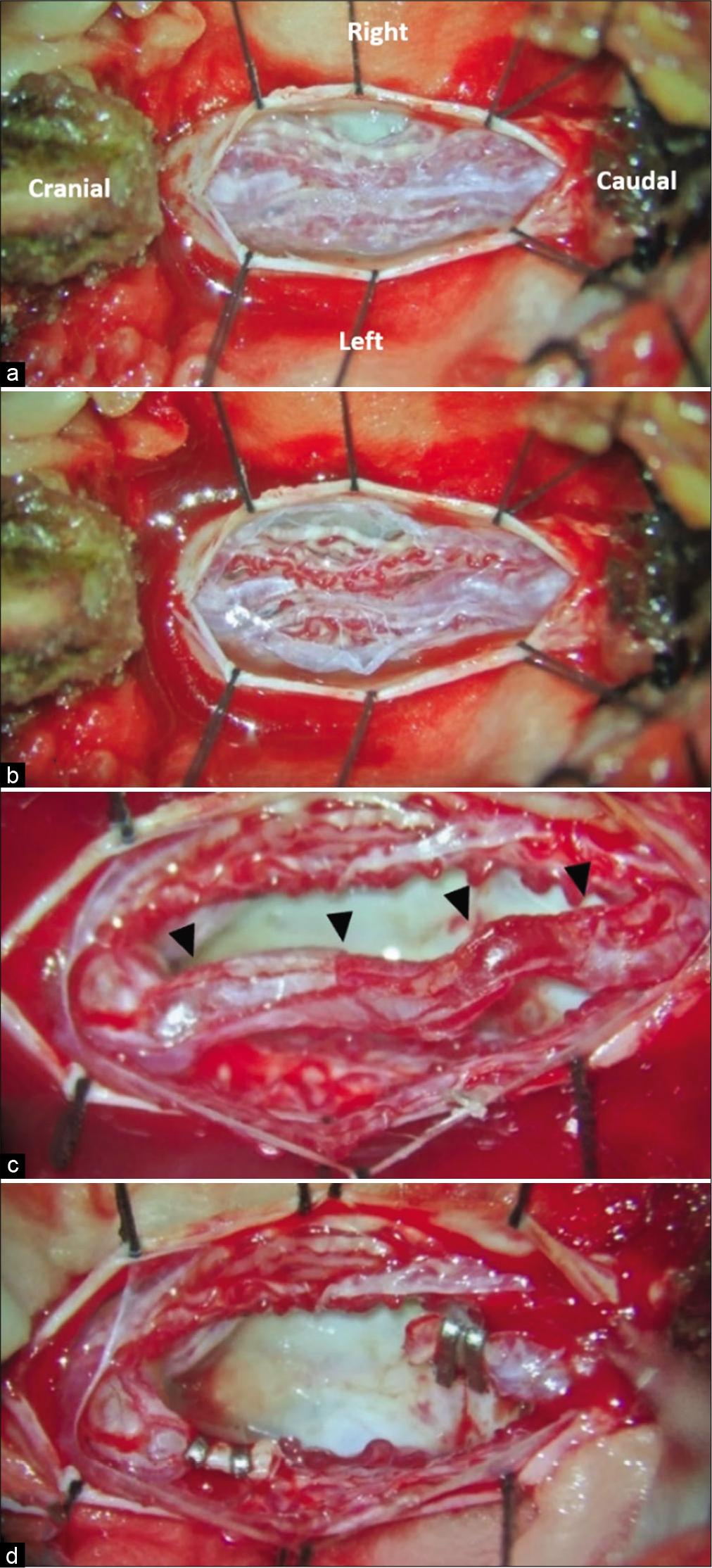
The patient underwent surgical treatment. To avoid invasive posterior sacrectomy, we decided to obliterate the dilated intradural draining vein rostral to the fistula. Laminotomy was performed at the level of L5. After durotomy, the arachnoid membrane was found to be thickened and opaque. The arachnoid was gently separated. The roots of the cauda equina were mattered together with adhesions. The FT was adhered within the clumping of the cauda equina. Lysis of adhesions between the nerve roots was performed. After lysis of adhesions, the engorged vein run parallel with the FT was identified. Part of the dilated vein was resected along with the FT [
Figure 5:
Intraoperative photograph during surgery on prone position after opening the dura at L5-S1 level. (a) the arachnoid membrane was found to be thickened and opaque. The roots of the cauda equina were mattered together. (b) After lysis of adhesions (c) The engorged vein run parallel with the filum terminale (arrowheads). (d) After clipping and resection of the filum terminale and dilated vein.
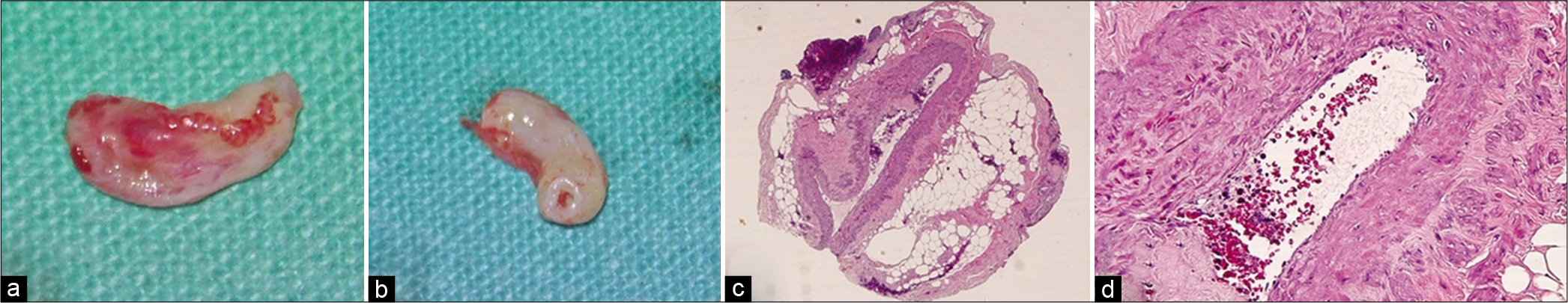
Figure 6:
(a and b) Gross specimens of the resected filum terminale and dilated vein of the filum. (c and d) The histopathological study shows dilated vessel and thickened vascular wall surrounded by fibroadipose tissue. Thick vascular wall consists of inner circular and outer longitudinal layer of smooth muscles (hematoxylin and eosin ×40 and ×200).
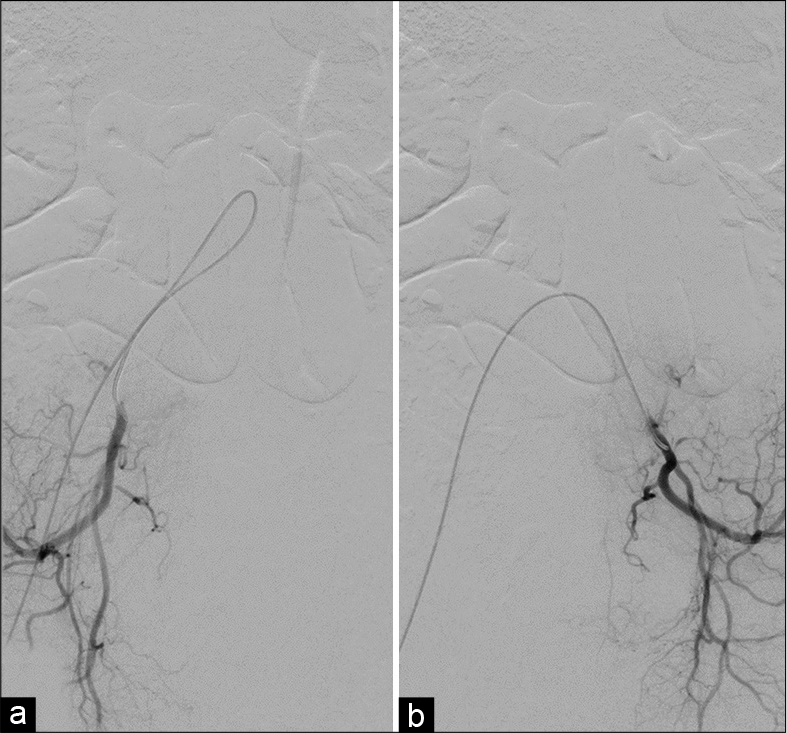
His postoperative course was uneventful. Follow-up spinal angiography obtained 1 week after the operation confirmed complete obliteration of an arteriovenous fistula [
Figure 8:
Magnetic resonance imaging of the thoracolumbar spine obtained 3 months after the operation. Sagittal views of T1-weighted (a and b) without and (c) with gadolinium injection and axial (d) T1-weighted, (e) T2-weighted, and (f) gradient-echo (GRE) T2*-weighted images at the level of L2 demonstrate hyperintense T1 (arrowheads) and T2 signal with blooming on GRE image along the flow void running from the level of L5 to L2, probably representing complete thrombosis of the vein of the filum terminale above the clipping point. There is only minimal persistent central cord enhancement.
Figure 9:
Sagittal T2-weighted image of the thoracolumbar spine obtained 3 months after the operation demonstrates the resolution of spinal cord congestion and disappearance of perimedullary flow voids. (b) Contrast-enhanced magnetic resonance angiography of the thoracolumbar spine confirms complete obliteration of the fistula.
DISCUSSION
The anatomy and blood supply of the FT
The FT is a thin fibrous band that attaches the tip of the conus medullaris to the dorsal surface of the coccyx.[
The artery of FT is the main feeding artery of the FTI from the tip of the conus medullaris to the area fused with the dural sac termination and can barely supply the FTE.[
The blood supply of the FTE remains unclear. The proximal FTE, junction with the dural sac termination, always contains remnants of meningothelial tissue.[
The MSA arises from the caudal end of the abdominal aorta at the dorsal surface. The branches of the LSA form numerous anastomoses with the lateral branches of the MSA.[
The vein of the FT, always larger than the artery of the FT, is located on the ventral aspect of the filum behind the artery of the FT throughout its course on the filum. The bidirectional venous drainage of this vein includes descending towards the sacral venous plexuses and ascending toward the perimedullary veins through anterior and posterior spinal veins or the juxtamedullary anastomoses at the level of the conus medullaris.[
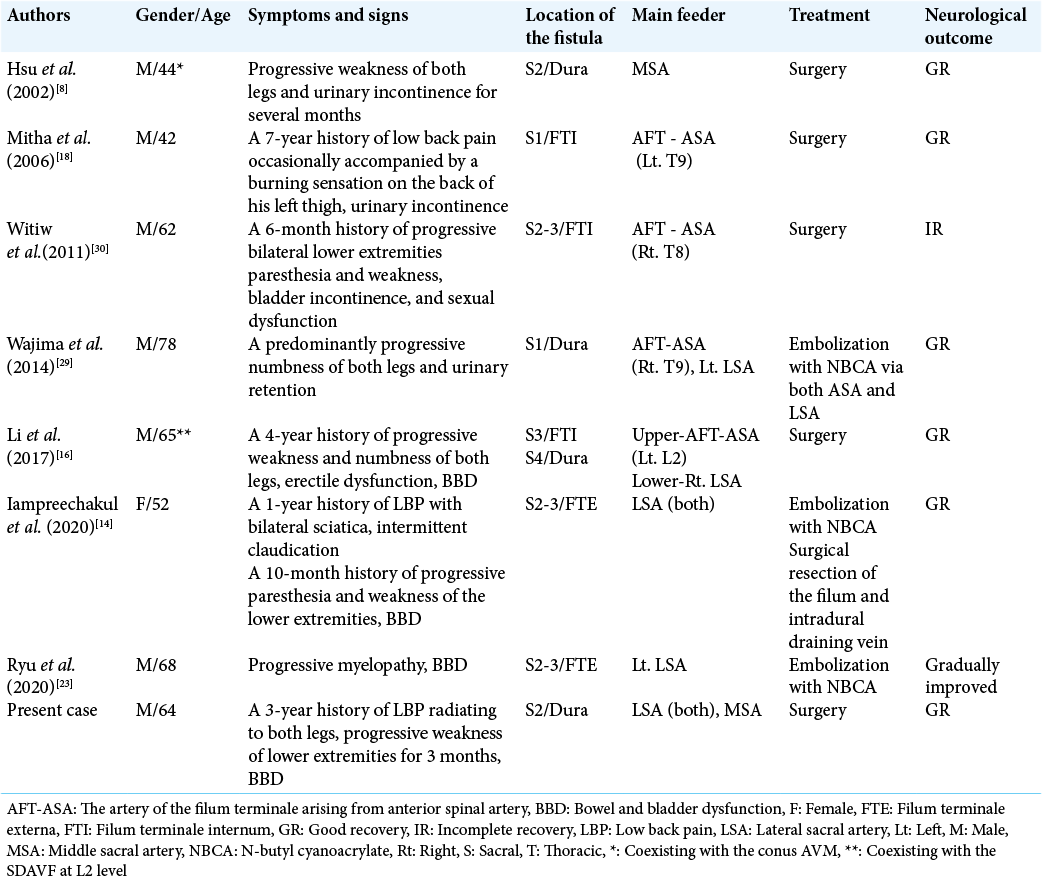
Literature review of sacral FTAVFs without spinal dysraphism
In our literature review, the collected data in this review include demographic data (i.e., gender and age of patient), symptoms and signs, location, and artery supply of the fistulas, treatment, and neurological outcome of the patients. There were eight cases, including our one case with nine sacral FTAVFs [
Spontaneous partial thrombosis of the vein of FT
Spontaneous thrombosis of spinal vascular malformations, including intramedullary arteriovenous malformation (AVM), perimedullary AVF, and DAVF, has been previously reported and is extremely rare. The mechanism of thrombosis remains unclear. Most thrombosed part of these lesions was the draining vein within spinal cord. No abnormal vessels on spinal angiography were identified. This condition is likely precipitate a rapid venous hypertension, leading to acute deterioration after a subacute myelopathic course, known as Foix-Alajouanine syndrome.[
Regarding signal intensities of MRI, hyperintense changes in the flow void or draining vein on T1-weighted sequences usually represent subacute thrombosis.[
Sacral DAVF of the FT
Sacral DAVF of the FT should be differentiate from cauda equina AVF, which was supplied from dural branches of the internal iliac and/or lateral sacral arteries. However, the drainage veins are radicular veins and usually follow the nerve roots, which locate more laterally and near the region of the sacral foramen.[
Ryu et al.[
The pathogenesis of FTAVF at the sacral region
The exact mechanism of formation of FTAVFs remains controversial. Scullen et al.[
Since 2002, Hsu et al.[
The relationship of the fatty FT and FTAVF
FT derived from involution of caudal neural tube. Histologic components of the normal filum may include fibroconnective tissue, neuroglial tissue, peripheral nerve twigs, and adipose tissue.[
Since 1989, Djindjian et al.[
In the present study, the findings of transected FT were consistent with the fatty FT. The association between the fatty filum terminale and fistulous formation is not well understood. Recently, Shimizu et al.[
Management of sacral DAVF of the FT
FTAVFs can be treated by surgery, endovascular treatment, or both. The goal of treatment is complete obliteration of the fistula with preservation of normal arterial supply to spinal cord. The key to complete occlusion is obliteration of the proximal vein.[
To avoid a longer and more invasive posterior sacrectomy, FTAVF at the sacral region may be treated indirectly by transection of the FT and vessels at lumbar segment rostral to the fistula.[
CONCLUSION
Sacral DAVFs of the FT are extremely rare. In our case, the formation of fistula may cause by venous hypertension secondary to partial thrombosis within the filum vein, probably resulting from long-standing spinal canal stenosis. Sacral FTAVFs may be found on the pia surface of the terminal FTI, dural component at the area of dural sac termination, or dural extension covering the FTE.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Cummings TJ, George TM. The immunohistochemical profile of the normal conus medullaris and filum terminale. Neuroembryology. 2003. 2: 43-9
2. Djindjian M, Ayache P, Brugieres P, Poirier J. Sacral lipoma of the filum terminale with dural arteriovenous fistula. Case report. J Neurosurg. 1989. 71: 768-71
3. Djindjian M, Ribeiro A, Ortega E, Gaston A, Poirier J. The normal vascularization of the intradural filum terminale in man. Surg Radiol Anat. 1988. 10: 201-9
4. Genevay S, Palazzo E, Huten D, Fossati P, Meyer O. Lumboradiculopathy due to epidural varices: Two case reports and a review of the literature. Joint Bone Spine. 2002. 69: 214-7
5. Giordan E, Brinjikji W, Ciceri E, Lanzino G. Arteriovenous fistulae of the filum terminale. J Neurointerv Surg. 2018. 10: 191-7
6. Gupta V, Rizvi T, Garg A, Gaikwad SB, Mishra NK. Postangiographic thrombosis of a spinal arteriovenous malformation: Case report. J Neurosurg Spine. 2005. 2: 486-90
7. Hansasuta A, Tubbs RS, Oakes WJ. Filum terminale fusion and dural sac termination: Study in 27 cadavers. Pediatr Neurosurg. 1999. 30: 176-9
8. Hsu SW, Rodesch G, Luo CB, Chen YL, Alvarez H, Lasjaunias PL. Concomitant conus medullaris arteriovenous malformation and sacral dural arteriovenous fistula of the filum terminale. Interv Neuroradiol. 2002. 8: 47-53
9. Iampreechakul P, Jitpun E, Wangtanaphat K, Lertbutsayanukul P, Khunvutthidee S, Siriwimonmas S. Filum terminale arteriovenous fistula coexisting with a large L2-L3 disc sequestration and associated diffuse lumbar arachnoiditis. Asian J Neurosurg. 2021. 16: 412-7
10. Iampreechakul P, Lertbutsayanukul P, Siriwimonmas S. Cauda equina arteriovenous fistula supplied by proximal radicular artery and concomitant sacral dural arteriovenous fistula: A case report and literature review. Surg Neurol Int. 2021. 12: 405
11. Iampreechakul P, Liengudom A, Wangtanaphat K, Narischat P, Lertbutsayanukul P, Siriwimonmas S. Intramedullary hemorrhage caused by lumbosacral epidural arteriovenous fistula with dual retrograde perimedullary venous draining routes: A case report and review of the literature. World Neurosurg. 2020. 143: 295-307
12. Iampreechakul P, Tangviriyapaiboon T, Liengudom A, Lertbutsayanukul P, Thammachantha S, Siriwimonmas S. Sacral extradural angiolipoma associated with tight filum terminale and spina bifida coexisting with spinal arteriovenous fistula. World Neurosurg. 2020. 140: 37-45
13. Iampreechakul P, Tirakotai W, Lertbutsayanukul P, Khunvutthidee S, Thammachantha S, Siriwimonmas S. Spinal sparganosis coexisting with acquired arteriovenous fistula of the filum terminale. World Neurosurg. 2020. 136: 341-7
14. Iampreechakul P, Tirakotai W, Wangtanaphat K, Lertbutsayanukul P, Siriwimonmas S. Filum terminale arteriovenous fistula in association with degenerative lumbosacral spinal canal stenosis: Report of 3 cases and review of the literature. World Neurosurg. 2020. 138: 231-41
15. Iampreechakul P, Yaisarn N, Wangtanaphat K, Lertbutsayanukul P, Siriwimonmas S, Techataweewan N. Filum terminale arteriovenous fistula with additional arterial supply by the posterior spinal artery: A report of two cases. Asian J Neurosurg. 2021. 16: 423-30
16. Li J, Li G, Bian L, Hong T, Yu J, Zhang H. Concomitant lumbosacral perimedullary arteriovenous fistula and spinal dural arteriovenous fistula. World Neurosurg. 2017. 105: 1041.e7-14
17. McLendon RE, Oakes WJ, Heinz ER, Yeates AE, Burger PC. Adipose tissue in the filum terminale: A computed tomographic finding that may indicate tethering of the spinal cord. Neurosurgery. 1988. 22: 873-6
18. Mitha AP, Murphy EE, Ogilvy CS. Type A intradural spinal arteriovenous fistula. Case report. J Neurosurg Spine. 2006. 5: 447-50
19. Mourier KL, Gobin YP, George B, Lot G, Merland JJ. Intradural perimedullary arteriovenous fistulae: Results of surgical and endovascular treatment in a series of 35 cases. Neurosurgery. 1993. 32: 885-91
20. Muthukumar N, Srisaravanan J. Intramedullary dermoid in a low lying conus tethered by a fatty filum-embryological implications. Acta Neurochir (Wien). 2007. 149: 1173-5
21. Namba K. Vascular anatomy of the cauda equina and its implication on the vascular lesions in the caudal spinal structure. Neurol Med Chir (Tokyo). 2016. 56: 310-6
22. Rodesch G, Hurth M, Alvarez H, Tadié M, Lasjaunias P. Classification of spinal cord arteriovenous shunts: Proposal for a reappraisal-the Bicêtre experience with 155 consecutive patients treated between 1981 and 1999. Neurosurgery. 2002. 51: 374-9
23. Ryu B, Sato S, Mochizuki T, Niimi Y. Spinal arteriovenous fistula located in the filum terminale externa: A case report and review of the literature. Interv Neuroradiol. 2021. 27: 451-5
24. Scullen T, Mathkour M, Amenta PS, Dallapiazza RF. Arteriovenous fistula of the filum terminale: A case report and review of the literature. World Neurosurg. 2019. 130: 42-9
25. Shimizu K, Mitsuhara T, Takeda M, Yamaguchi S. Spinal arteriovenous fistula in the lipoma of the filum terminale: A report of two cases and literature review. Surg Neurol Int. 2021. 12: 103
26. Takai K, Komori T, Taniguchi M. Angioarchitecture of filum terminale arteriovenous fistulas: Relationship with a tethered spinal cord. World Neurosurg. 2019. 122: e795-804
27. Takai K, Usui M. Spontaneous thrombosis of a spinal conus perimedullary arteriovenous fistula. Case report. Neurol Med Chir (Tokyo). 2012. 52: 103-6
28. Tubbs RS, Murphy RL, Kelly DR, Lott R, Salter EG, Oakes WJ. The filum terminale externum. J Neurosurg Spine. 2005. 3: 149-52
29. Wajima D, Nakagawa I, Park HS, Haku T, Wada T, Kichikawa K. A case of filum terminale arterial venous fistula needed a long arterial access for trans-arterial shunt obliteration. Interv Neuroradiol. 2017. 23: 221-7
30. Witiw CD, Fallah A, Radovanovic I, Wallace MC. Sacral intradural arteriovenous fistula treated indirectly by transection of the filum terminale: Technical case report. Neurosurgery. 2011. 69: E780-4
31. Zimmerman GA, Weingarten K, Lavyne MH. Symptomatic lumbar epidural varices. Report of two cases. J Neurosurg. 1994. 80: 914-8