- Department of Neurosurgery, Rush University Medical Center, Chicago, United States.
- Section of Otolaryngology, Northshore University HealthSystem, Evanston, Illinois, United States.
- Department of Neurosurgery, NorthShore University HealthSystem, Evanston, Illinois, United States.
Correspondence Address:
Ricky H. Wong
Department of Neurosurgery, NorthShore University HealthSystem, Evanston, Illinois, United States.
DOI:10.25259/SNI_6_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Andrew K. Wong, Joseph Raviv, Ricky H. Wong. Sellar trough technique for endoscopic endonasal transclival repair. 09-May-2020;11:99
How to cite this URL: Andrew K. Wong, Joseph Raviv, Ricky H. Wong. Sellar trough technique for endoscopic endonasal transclival repair. 09-May-2020;11:99. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10018
Abstract
Background: Endoscopic endonasal transclival approaches provide direct access to the ventral skull base allowing the treating of clival and paraclival pathology without the manipulation of the brain or neurovascular structures. Postoperative spinal fluid leak, however, remains a challenge and various techniques have been described to reconstruct the operative defect. The “gasket seal” has been well-described, but has anatomic challenges when applied to clival defects. We describe a modification of this technique for use in endonasal transclival approaches.
Methods: Two patients who underwent an endoscopic endonasal transclival approach for tumor resection with an intraoperative spinal fluid leak underwent a modified “gasket seal” closure technique for skull base reconstruction.
Results: A 71-year-old woman with a petroclival meningioma and a 22 year old with a clival chordoma underwent endoscopic endonasal transclival resection with the modified repair. No new postoperative deficits occurred and no postoperative spinal fluid leak was seen with a follow-up of 17 and 23 months, respectively.
Conclusion: We describe the successful use of a simple, low risk, and technique modification of the “gasket seal” technique adapted to the clivus that allows for hard reconstruction and facilitates placement of the nasoseptal flap.
Keywords: Cerebrospinal fluid leak, Endoscopic endonasal approach, Endoscopic endonasal transclival, Skull base, Transclival
INTRODUCTION
The endonasal approach has increasingly moved beyond the sellar region. These expanded approaches can involve larger dural defects, high-flow cerebrospinal fluid (CSF) leaks, and local anatomy that can make dural repair and reconstruction challenging. The postoperative CSF leak rate in this setting has been reported to be as high as 30% when nonvascularized flap repair was used.[
METHODS
The charts of two patients who underwent an endoscopic endonasal transclival approach for tumor resection utilizing the modified “gasket seal” closure were reviewed and results reported. One patient was treated for a clival chordoma while the other for a petroclival meningioma.
Operative technique
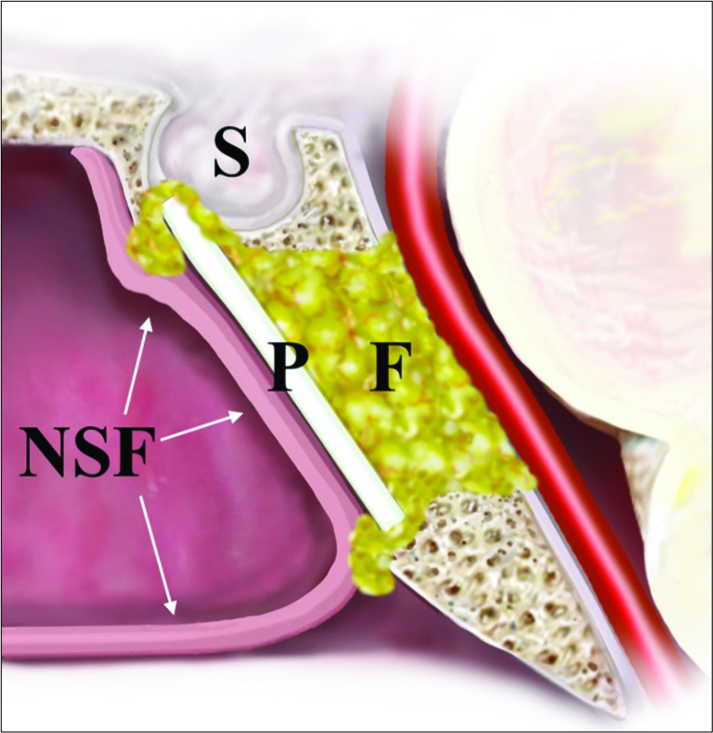
The patient is placed supine on the operating table with the head on a gel donut headrest in mild extension and turned toward the operator. A two operator, four handed, and bi-nostral approach are employed. A nasal septal flap is elevated on the right and a submucosal, subperiosteal dissection for a transseptal approach is taken in the left nare. The sphenoid sinus is then opened widely and the ventral skull base closely inspected. The clival recess is skeletonized from paraclival carotid to paraclival carotid and from the sella to the inferior extent of the tumor. Once the tumor has been resected, attention is directed at closure. Using a high-speed drill and kerrison rongeur, a transverse trough along the ventral most aspect of the sella is prepared. A periumbilical fat graft obtained at the beginning of the surgery is sized appropriately and placed into the prepontine space extending through the clival defect with some mild extrusion into the sphenoid sinus. The PP implant (Medpor; Stryker; Kalamazoo, MI) is shaped and sized and advanced into the region of the defect. The inferior edge of the implant is seated into the caudal end of the clival defect that then acts as a fulcrum as the superior edge of the implant is advanced posteriorly until it snaps into the trough – the plate rests between the sellar dura and the sellar face [
RESULTS
Patient 1
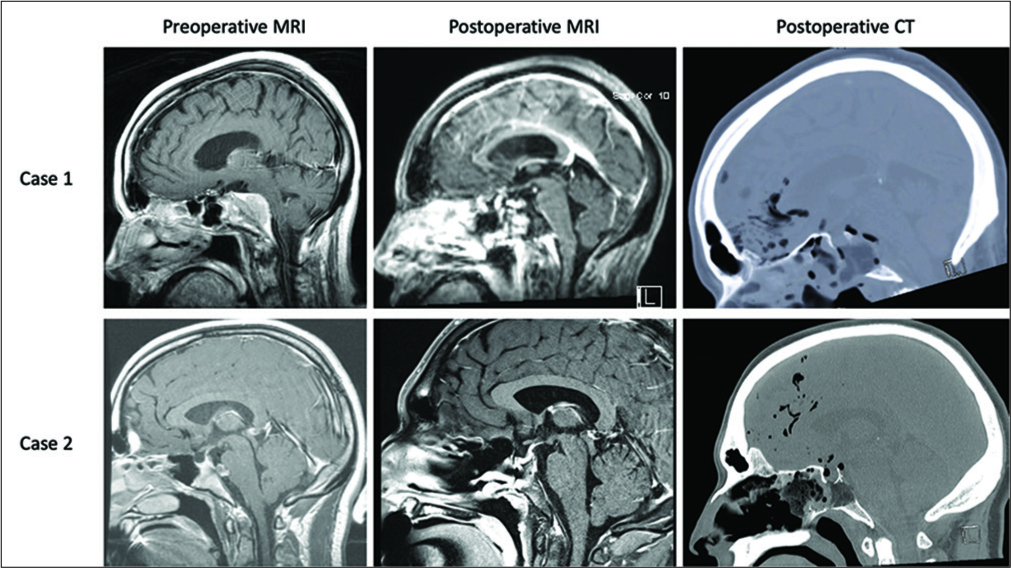
A 71 year-old female with a right-sided petroclival meningioma presented with a right abducens nerve palsy. Near-total resection was achieved with residual tumor left adherent on the right abducens nerve. The modified “gasket seal” closure technique was used. The operative duration was 178 min. Hospital length of stay was 6 days. No postoperative CSF leak was noted with a follow-up of 17 months.
Patient 2
A 22-year-old male with incidentally found clival chordoma with noted growth and intradural invasion on follow-up imaging. This patient was without cranial nerve deficits before surgery. Gross total resection was achieved. An expected intraoperative CSF leak was observed. The modified “gasket seal” closure technique was used. The operative duration was 171 min. Hospital length of stay was 4 days. No postoperative CSF leak was noted with a follow up of 23 months [
DISCUSSION
The endoscopic endonasal approach to the clivus allows for access to the ventral skull base and the epicenter of these lesions without the need for brain retraction. Postoperative CSF leak is a known complication of endoscopic endonasal approaches with reported rates in transclival approaches as high as 25–35%.[
Typical prevention strategies include CSF diversion through a lumbar drain, utilizing a multilayered closure, use of an abdominal fat graft, and buttressing of the closure. Some have proposed primary dural closure, though the depth and dural condition generally make it technically challenging.[
The use of hard reconstruction has some potential concerns. When countersunk into the depth, in an immediate intradural or extradural location, the abducens nerve running along the petroclival fissure bilaterally can be placed at risk. When placed within the clival defect, depending on the degree of exposure, the paraclival carotids could be placed at risk. This has led some to avoid hard reconstruction in all transclival cases, instead of relying on nasal splints or Foley balloons. In a large retrospective study on multilayer closure with the use of a nasoseptal flap without hard reconstruction, there was a 13.6% of posterior fossa anatomic abnormalities including pontine encephaloceles.[
One of the most significant advances in the endonasal skull base closure technique is the Hadad-Bassagasteguy vascularized nasoseptal flap.[
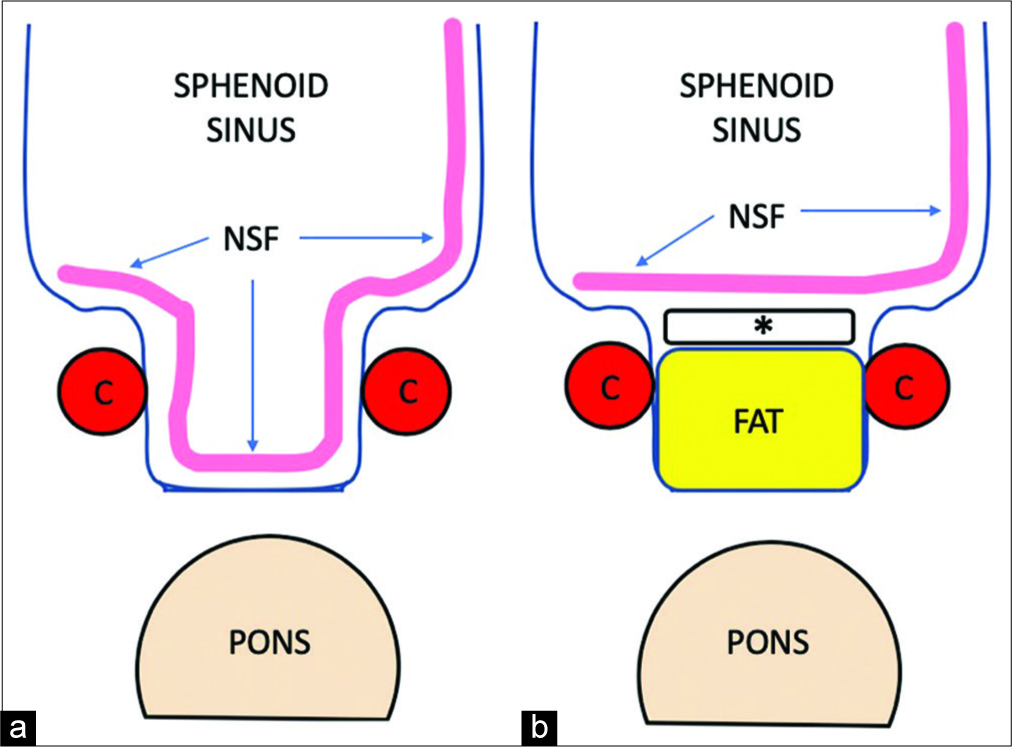
Our modification of the “gasket seal” technique utilizes the effectiveness of the nasoseptal flap by eliminating the need for a free fascial graft incorporated into the hard reconstruction. Since the initial description of the “gasket seal” predates the vascularized nasoseptal flap, it necessitated a fascial watertight layer in the technique. We use the autologous fat graft to achieve a watertight seal within the clival defect and still maintain a “gasket” effect at the superficial aspect of the fat graft by creating a slight overflow of fat into the sphenoid sinus cavity. This also allows tethering of the fat graft that prevents shifting or migration. We also translate the hard reconstruction to a more ventral location in-line with the sellar face. This obviates the risk to the abducens nerve and the paraclival arteries. We also tailor the width of the plate to be slightly less than the width of the defect, using only the upper sellar bone ledge and inferior clivus as a two-point anchor system. The absence of critical neurovascular structures superior and inferior allows a simple and safe rigid layer that acts as a bridge between the two sides of the clival recess. This adaptation also shortens the length of nasoseptal flap required as it eliminates the need for the flap to traverse the depth of the clival defect, thus making the likelihood of an insufficient flap size much lower [
Figure 3:
Schematic demonstrating the effect of the modified “gasket seal” technique on nasoseptal flap placement. (a) A normal “gasket seal” requires the flap to traverse the depth of the defect; (b) The modification allows the flap to lay flat across the hard reconstruction. NSF: Nasoseptal flap, C: Paraclival carotid.
While this report is limited by its number of cases, the purpose is to describe a technique that would theoretically provide a system of low-risk hard reconstruction while facilitating the use of a nasoseptal flap. More definitive assessment of the risks and benefits of this modification will require more experience. In addition, since the plate is held in place rostrally and caudally, a small amount of sellar face is required in addition to a portion of the inferior clivus.
The endoscopic endonasal transclival approach is an attractive option to surgically treating various clival and paraclival pathologies. Postoperative CSF leak remains a significant risk despite the development of various closure methods. We describe the successful use of a simple, low risk, and technique modification of the “gasket seal” technique adapted to the clivus that allows for hard reconstruction and facilitates placement of the nasoseptal flap.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Acerbi F, Genden E, Bederson J. Circumferential watertight dural repair using nitinol U-clips in expanded endonasal and sublabial approaches to the cranial base. Neurosurgery. 2010. 67: 448-56
2. D’Anza B, Tien D, Stokken JK, Recinos PF, Woodard TR, Sindwani R. Role of lumbar drains in contemporary endonasal skull base surgery: Meta-analysis and systematic review. Am J Rhinol Allergy. 2016. 30: 430-5
3. Dehdashti AR, Karabatsou K, Ganna A, Witterick I, Gentili F. Expanded endoscopic endonasal approach for treatment of clival chordomas: Early results in 12 patients. Neurosurgery. 2008. 63: 299-307
4. Dehdashti AR, Stofko D, Okun J, Obourn C, Kennedy T. Endoscopic endonasal reconstruction of skull base: Repair protocol. J Neurol Surg B Skull Base. 2016. 77: 271-8
5. Eloy JA, Choudhry OJ, Friedel ME, Kuperan AB, Liu JK. Endoscopic nasoseptal flap repair of skull base defects: Is addition of a dural sealant necessary?. Otolaryngol Head Neck Surg. 2012. 147: 161-6
6. Eloy JA, Kuperan AB, Choudhry OJ, Harirchian S, Liu JK. Efficacy of the pedicled nasoseptal flap without cerebrospinal fluid (CSF) diversion for repair of skull base defects: Incidence of postoperative CSF leaks. Int Forum Allergy Rhinol. 2012. 2: 397-401
7. Fraser JF, Nyquist GG, Moore N, Anand VK, Schwartz TH. Endoscopic endonasal minimal access approach to the clivus: Case series and technical nuances. Neurosurgery. 2010. 67: ons150-8
8. Hadad G, Bassagasteguy L, Carrau RL, Mataza JC, Kassam A, Snyderman CH. A novel reconstructive technique after endoscopic expanded endonasal approaches: Vascular pedicle nasoseptal flap. Laryngoscope. 2006. 116: 1882-6
9. Ishii Y, Tahara S, Teramoto A, Morita A. Endoscopic endonasal skull base surgery: Advantages, limitations, and our techniques to overcome cerebrospinal fluid leakage: Technical note. Neurol Med Chir (Tokyo). 2014. 54: 983-90
10. Koutourousiou M, Filho FV, Costacou T, Fernandez-Miranda JC, Wang EW, Snyderman CH. Pontine encephalocele and abnormalities of the posterior fossa following transclival endoscopic endonasal surgery. J Neurosurg. 2014. 121: 359-66
11. Leng LZ, Brown S, Anand VK, Schwartz TH. “Gasket-seal” watertight closure in minimal-access endoscopic cranial base surgery. Neurosurgery. 2008. 62: ONSE342-3
12. Patel MR, Stadler ME, Snyderman CH, Carrau RL, Kassam AB, Germanwala AV. How to choose? Endoscopic skull base reconstructive options and limitations. Skull Base. 2010. 20: 397-404
13. Peris-Celda M, Pinheiro-Neto CD, Funaki T, Fernandez-Miranda JC, Gardner P, Snyderman C. The extended nasoseptal flap for skull base reconstruction of the clival region: An anatomical and radiological study. J Neurol Surg B Skull Base. 2013. 74: 369-85
14. Rahme RJ, Arnaout OM, Sanusi OR, Kesavabhotla K, Chandler JP. Endoscopic approach to clival chordomas: The Northwestern experience. World Neurosurg. 2018. 110: e231-8
15. Soudry E, Turner JH, Nayak JV, Hwang PH. Endoscopic reconstruction of surgically created skull base defects: A systematic review. Otolaryngol Head Neck Surg. 2014. 150: 730-8
16. Stippler M, Gardner PA, Snyderman CH, Carrau RL, Prevedello DM, Kassam AB. Endoscopic endonasal approach for clival chordomas. Neurosurgery. 2009. 64: 268-77
17. Zanation AM, Carrau RL, Snyderman CH, Germanwala AV, Gardner PA, Prevedello DM. Nasoseptal flap reconstruction of high flow intraoperative cerebral spinal fluid leaks during endoscopic skull base surgery. Am J Rhinol Allergy. 2009. 23: 518-21