- College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia.
- King Abdullah International Medical Research Center, Riyadh, Saudi Arabia.
- Division of Neurosurgery, Department of Surgery, King Abdulaziz Medical City, Ministry of National Guard - Health Affairs, Riyadh, Saudi Arabia.
- Department of Pathology and Laboratory Medicine, King Abdulaziz Medical City, Ministry of National Guard - Health Affairs, Riyadh, Saudi Arabia.
Correspondence Address:
Ali Alkhaibary, College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia.
DOI:10.25259/SNI_1180_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ahoud Alharbi1,2,3, Ali Alkhaibary1,2,3, Abeer Alaglan1,2,3, Sami Khairy1,2,3, Zahra Alkhunaizi2,4, Fahd AlSufiani2,4, Ali H. Alassiri1,2,4, Ahmed Alkhani2,3. Sellar xanthogranuloma: A diagnostic challenge. 04-Mar-2022;13:76
How to cite this URL: Ahoud Alharbi1,2,3, Ali Alkhaibary1,2,3, Abeer Alaglan1,2,3, Sami Khairy1,2,3, Zahra Alkhunaizi2,4, Fahd AlSufiani2,4, Ali H. Alassiri1,2,4, Ahmed Alkhani2,3. Sellar xanthogranuloma: A diagnostic challenge. 04-Mar-2022;13:76. Available from: https://surgicalneurologyint.com/surgicalint-articles/11425/
Abstract
Background: Sellar xanthogranulomas are rare intracranial lesions comprising
Case Description: A 43-year-old female, known to have diabetes, hypothyroidism, and polycystic ovarian syndrome, presented with a 2-week history of sudden right-sided facial deviation, periorbital pain, and moderate-intensity headache. The patient also reported amenorrhea not improving with polycystic ovarian syndrome treatment. Neurologic examination showed bilateral visual field defects and impaired visual acuity. Computed tomography scan, without contrast, revealed a hypodense sellar lesion with areas of hyperdensity. Magnetic resonance imaging showed a well-defined sellar lesion, exhibiting high signals on T1-weighted and T2-weighted images. The patient underwent microscopic trans-nasal trans-sphenoidal excision of the lesion. Histological sections of the sellar lesion revealed fibrous connective tissue with chronic inflammatory cells and cholesterol clefts, suggestive of xanthogranuloma. The patient is currently followed up at neurosurgery, endocrinology, and ophthalmology clinics with periodic laboratory/radiological investigations.
Conclusion: Sellar xanthogranulomas remain rare intracranial lesions with few cases reported in the literature. Patients mostly present with severe hypopituitarism and visual dysfunction. They show no characteristic radiological features. The diagnosis is confirmed histopathologically, and the prognosis is generally favorable.
Keywords: Adenohypophysis, Cholesterol, Fibrous, Foamy, Granuloma, Pituitary
INTRODUCTION
Sellar xanthogranulomas, also known as cholesterol granulomas, are rare brain lesions comprising 0.6% of all sellar tumors.[
Because of the paucity of sellar xanthogranuloma cases reported in the literature, they remain a diagnostic challenge with indefinite origin, clinical course, and outcome. The present study reports a case of sellar xanthogranuloma by describing the clinical presentation, radiological/pathological characteristics, and outcome.
CASE DESCRIPTION
Clinical presentation
A 43-year-old female was known to have diabetes, hypothyroidism, and polycystic ovarian syndrome. The patient was in her usual state of health until 2 weeks before her presentation when she developed a sudden right-sided facial deviation, periorbital pain, and moderate-intensity headache. The patient acknowledged chronic history of mild bifrontal headache for the past 3 years, for which she did not seek medical attention. Furthermore, the patient reported amenorrhea for the same duration, not improving with polycystic ovarian syndrome treatment. On further inquiry, the patient reported difficulties in visualizing objects located in her peripheral fields. There was no history of galactorrhea, cold/heat intolerance, weight gain/loss, or hirsutism.
Physical examination
The patient was alert and oriented with a Glasgow Coma Scale of 15/15. The pupils were 3 mm reactive to light and accommodation bilaterally. The extraocular muscles movement was intact with no ptosis. The color vision test was normal. The corneas and anterior chambers were clear. Fundoscopy revealed healthy discs and maculae bilaterally. The 24-2 Humphrey test revealed bilateral visual field defects. The visual acuity was impaired bilaterally (right eye: 20/30 and left eye: 20/50). Otherwise, the patient was neurologically intact.
Neuroradiological imaging
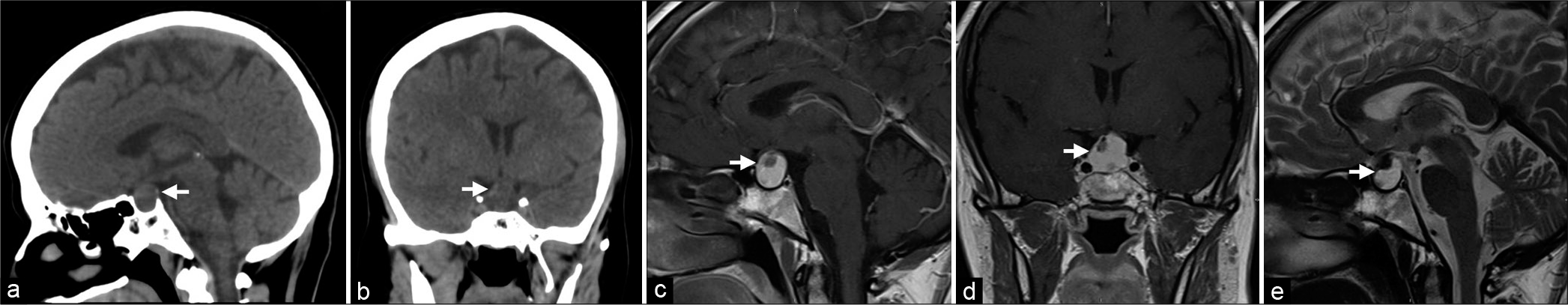
Computed tomography (CT) scan without contrast revealed a hypodense sellar lesion with areas of hyperdensity [
Figure 1:
(a and b) Sagittal and coronal brain CT without contrast showing a hypodense lesion with areas of hyperdensities (Arrow). (c and d) Sagittal and coronal T1-weighed images with contrast of the pituitary gland. (e) Sagittal T2-weighted image. (c-e) The images demonstrate a well-defined, rounded sellar mass which exhibit a high signal on T1- and T2-weighted images (Arrow). The lesion causes deviation of the pituitary stalk to the left side and abuts the optic chiasm. It measures 19 × 20 × 12 mm in anteroposterior, transverse, and craniocaudal diameters.
Surgical intervention
Considering the brain CT and MRI findings, surgical resection of the lesion was performed to establish the diagnosis. The patient underwent microscopic trans-nasal trans-sphenoidal excision of the pituitary gland. Intraoperatively, the tumor was readily visualized. Multiple samples were obtained and sent for permanent histopathology. Most of the visualized parts of the tumor were removed. Grossly, the tumor consisted of multiple pieces of tan, soft-tissue measuring, in aggregate, 1 × 1 × 0.5 cm.
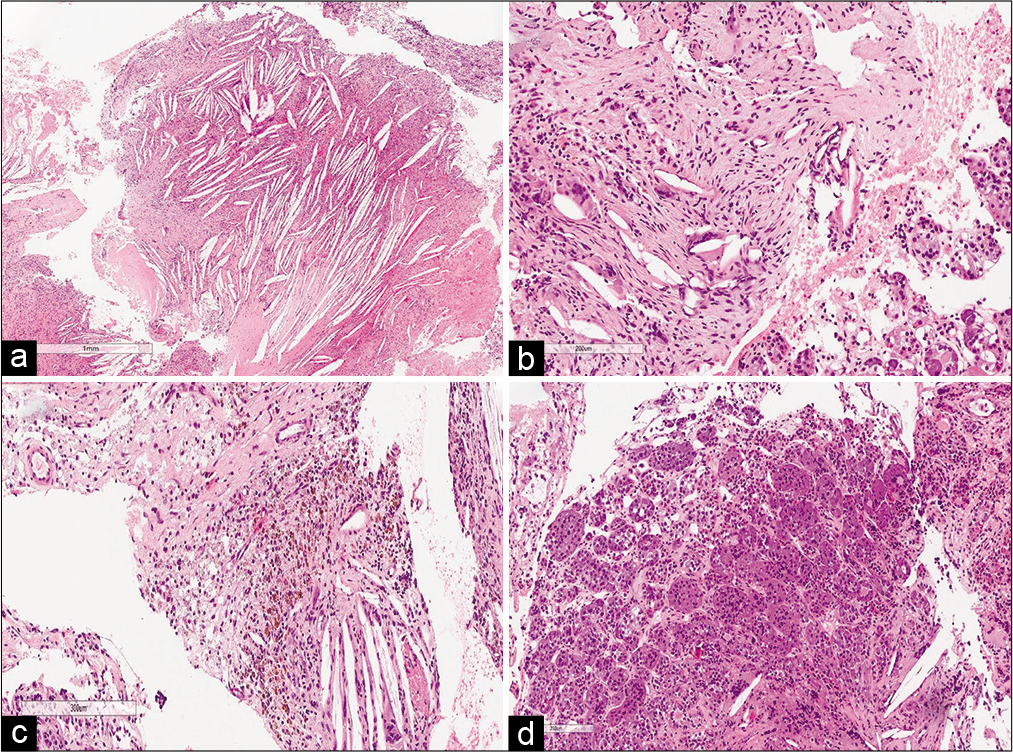
Histopathological findings
Histological sections of the sellar lesion revealed fibrous connective tissue with chronic inflammatory cells and cholesterol clefts. Scattered foreign body giant cells were noticed with focal hemosiderin deposits and foamy histiocytes [
Outcome and follow-up
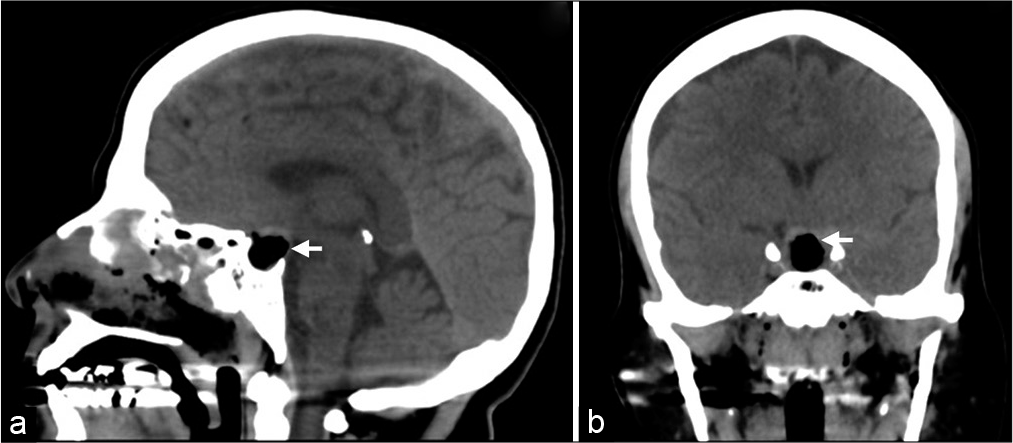
The patient tolerated the surgery well without complications. She was kept in the intensive care unit for 2 days for close monitoring. Serum sodium, serum osmolality, and urine osmolality levels were all within normal limits. There was no clinical or laboratory evidence suggestive of diabetes insipidus. Apart from her preexisting hypothyroid state, the pituitary hormonal profile was within normal during her hospital stay. Brain CT scan, 1 day following surgery, confirmed resection of the lesion [
DISCUSSION
Sellar xanthogranulomas are rare intracranial lesions with few cases reported on review of the literature. We hereby report an additional case of such uncommon sellar lesion encountered in our tertiary care center.
The origin of sellar xanthogranulomas is yet undetermined. Sellar xanthogranulomas were first considered as a variant of adamantinomatous craniopharyngioma.[
Xanthogranulomas with squamous epithelium and calcifications have been reported to arise from adamantinomatous craniopharyngioma.[
Pituitary xanthogranulomas are radiologically indistinct and show mixed intensities due to the complex histologic components of the lesions. It has been speculated that hemosiderin deposits show hypointense signals on T2WI.[
Surgical resection remains the mainstay of treatment of sellar xanthogranulomas with gross total resection as the gold standard.[
Considering the rarity of sellar xanthogranuloma, the clinical presentation, and radiological features of the present case, other differential diagnoses of sellar lesions were initially considered. The patient underwent near total resection of the lesion due to its adherence to the diaphragma sellae. The diagnosis of sellar xanthogranuloma was confirmed histopathologically, and the patient had an excellent outcome.
CONCLUSION
Sellar xanthogranulomas remain rare intracranial lesions with few cases reported in the literature. Patients mostly present with severe hypopituitarism and visual dysfunction. They show no characteristic radiological features. The diagnosis is confirmed histopathologically, and the prognosis is generally favorable.
Authors’ contributions
Ahoud Alharbi: Writing – Original Draft, Writing – Review and Editing. Ali Alkhaibary: Conceptualization, Investigations – Radiological and Pathological images, Writing – Original Draft, Writing – Review and Editing. Abeer Alaglan: Conceptualization, Investigations – Radiological and Pathological images, Writing – Original Draft, Writing – Review and Editing. Sami Khairy: Conceptualization, Supervision, Writing – Review and Editing. Zahra Alkhunaizi: Investigations –Pathological images, Microscopic Description, Writing – Review and Editing. Fahd AlSufiani: Conceptualization, Investigation – Microscopic Description, Supervision, Writing – Review and Editing. Ali H. Alassiri: Conceptualization, Investigation – Microscopic Description, Supervision, Writing – Review and Editing. Ahmed Alkhani: Surgical Management, Supervision, Writing – Review and Editing. All authors have critically reviewed and approved the final version of the manuscript.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to express their gratitude to King Abdullah International Medical Research Center, Ministry of National Guard - Health Affairs, Riyadh, Saudi Arabia for approving the study. The assigned protocol number for approval is NR21R/358/09.
References
1. Agarwal A, Agarwal K, Lee HK. Xanthogranuloma of the sellar region: A case report. Neuroradiol J. 2012. 25: 181-4
2. Amano K, Kubo O, Komori T, Tanaka M, Kawamata T, Hori T. Clinicopathological features of sellar region xanthogranuloma: Correlation with Rathke’s cleft cyst. Brain Tumor Pathol. 2013. 30: 233-41
3. Fujio S, Takajo T, Kinoshita Y, Hanaya R, Arimura H, Sugata J. Sellar xanthogranuloma: A quest based on nine cases assessed with an anterior pituitary provocation test. World Neurosurg. 2019. 130: e150-9
4. Hernández-Estrada RA, Kshettry VR, Vogel AN, Curtis MT, Evans JJ. Cholesterol granulomas presenting as sellar masses: A similar, but clinically distinct entity from craniopharyngioma and Rathke’s cleft cyst. Pituitary. 2017. 20: 325-32
5. Kleinschmidt-DeMasters BK, Lillehei KO, Hankinson TC. Review of xanthomatous lesions of the sella. Brain Pathol. 2017. 27: 377-95
6. Le BH, Towfighi J, Kapadia SB, Lopes MB. Comparative immunohistochemical assessment of craniopharyngioma and related lesions. Endocr Pathol. 2007. 18: 23
7. Nishiuchi T, Murao K, Imachi H, Kushida Y, Haba R, Kawai N. Xanthogranuloma of the intrasellar region presenting in pituitary dysfunction: A case report. J Med Case Rep. 2012. 6: 1-7
8. Paulus W, Honegger J, Keyvani K, Fahlbusch R. Xanthogranuloma of the sellar region: A clinicopathological entity different from adamantinomatous craniopharyngioma. Acta Neuropathol. 1999. 97: 377-82
9. Rahmani R, Sukumaran M, Donaldson AM, Akselrod O, Lavi E, Schwartz TH. Parasellar xanthogranulomas. J Neurosurg. 2015. 122: 812-7
10. Shao X, Wang C, Min J. Xanthogranuloma of the sellar region: A case report. Medicine (Baltimore). 2020. 99: e22619
11. Shirataki K, Okada S, Matsumoto S. Histopathological study of the “cholesterol granuloma reaction” in the sellar and juxtasellar tumors. No To Shinkei. 1988. 40: 133-9
12. Ved R, Logier N, Leach P, Davies JS, Hayhurst C. Pituitary xanthogranulomas: Clinical features, radiological appearances and post-operative outcomes. Pituitary. 2018. 21: 256-65
13. Yang B, Yang C, Fang J, Li G, Wang J, Jia G. Clinicoradiologic features and surgical outcomes of sellar xanthogranulomas: A single-center 10-year experience. World Neurosurg. 2017. 99: 439-7