- Department of Neurological Surgery, Rutgers - Robert Wood Johnson Medical School, New Jersey, United States
- Fetal Centre, Department of Obstetrics and Gynecology, University of Texas McGovern Medical School, Houston, Texas, United States
- Department of Neurological Surgery, New Jersey Medical School, RUTGERS, Newark, New Jersey, United States.
Correspondence Address:
Gaurav Gupta, Department of Neurological Surgery, Rutgers - Robert Wood Johnson Medical School, New Jersey, United States.
DOI:10.25259/SNI_828_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sanjeev A. Sreenivasan1, Neha Agarwal2, Sudipta Roychowdhury1, Priyank Khandelwal3, Anil Nanda1, Gaurav Gupta1. Sequential aneurysms with incidental persistent primitive trigeminal artery: Is this association purely coincidental? A case study and review of the literature in search for a pathobiological mechanism. 04-Nov-2022;13:508
How to cite this URL: Sanjeev A. Sreenivasan1, Neha Agarwal2, Sudipta Roychowdhury1, Priyank Khandelwal3, Anil Nanda1, Gaurav Gupta1. Sequential aneurysms with incidental persistent primitive trigeminal artery: Is this association purely coincidental? A case study and review of the literature in search for a pathobiological mechanism. 04-Nov-2022;13:508. Available from: https://surgicalneurologyint.com/surgicalint-articles/11977/
Abstract
Background: The appearance of sequential bilateral aneurysms in patients with persistent primitive trigeminal artery (PTA) is not described in the literature. No clear guidelines on screening and follow-up of patients with incidental PTAs for the detection of associated lesions have been established.
Case Description: A 55-year-old lady presented with occasional headaches. Detailed evaluation showed a left ophthalmic segment internal carotid artery (ICA) aneurysm measuring (11.2 × 5.5) mm. A bovine aortic arch configuration (type III) and a persistent left PTA were identified. A pipeline flex flow diverter was placed and aneurysm was coiled. Follow-up angiography after 6 months showed a completely occluded aneurysm with preserved PTA and a new aneurysm in the right ICA ophthalmic segment measuring 3.5 × 1.5 mm. It was followed up serially with angiography which revealed significant increase in 6 months. The base measured 5.4 mm and two blebs 3.1 mm and 2.5 mm had appeared on the dome. A SUPRASS flow diverter was placed across this aneurysm. Serial follow-up showed complete occlusion of the left aneurysm and significant reduction in filling of the right aneurysm. A review of the literature identified 34 cases of incidental PTAs associated with 50 aneurysms with increased prevalence of anterior circulation aneurysms in patients with incidental PTA.
Conclusion: Sequential angiography of a patient with incidental PTA and an ICA aneurysm shows presence of a new aneurysm in contralateral circulation and its progression in size and morphology. Detailed large-scale studies are needed to assess the impact of incidental PTA on aneurysm development and management.
Keywords: Aneurysm, Flow diverter, Persistent trigeminal artery
INTRODUCTION
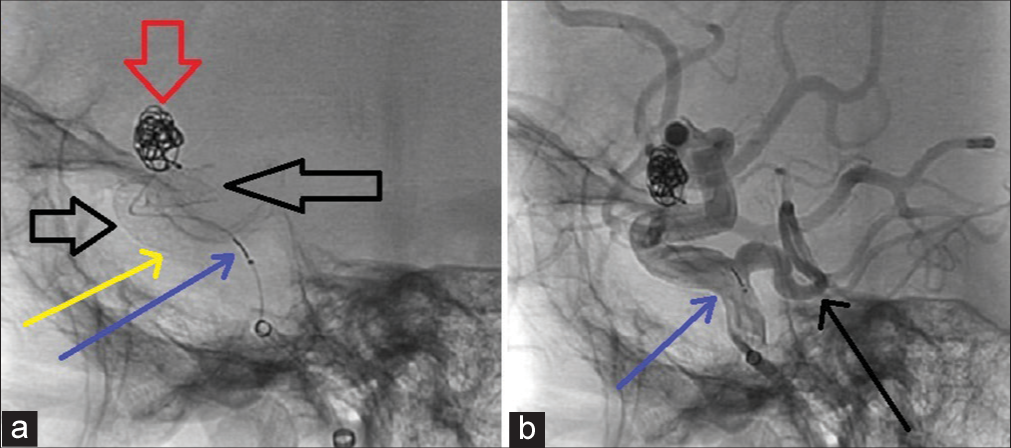
The appearance of sequential bilateral aneurysms in patients with persistent primitive trigeminal artery (PTA) is not described in the literature. There is disputing evidence in favor of long-term screening strategies for patients with incidental PTAs and cerebral aneurysms. We conducted a review with the aim to find out whether the associations of PTA with aneurysms are incidental or does it have a pathobiological mechanism? Does specific embryological or genetic mechanism predispose to aneurysms in patient with PTA? Does it have any clinical implications on long-term follow-up? A Google Scholar and PubMed search revealed 3270 articles where 34 studies had 50 aneurysms with incidental PTAs [
CASE DETAILS
A 55-year-old lady presented to the clinic with occasional headaches. She did not have family history of cerebral aneurysms. An outside computerized tomography scan showed hyperdensity in the right supraclinoid region. As further evaluation, she underwent diagnostic digital subtraction angiography (DSA). A persistent trigeminal artery communicating between cavernous portion of the left internal carotid artery (ICA) and basilar artery was noticed [
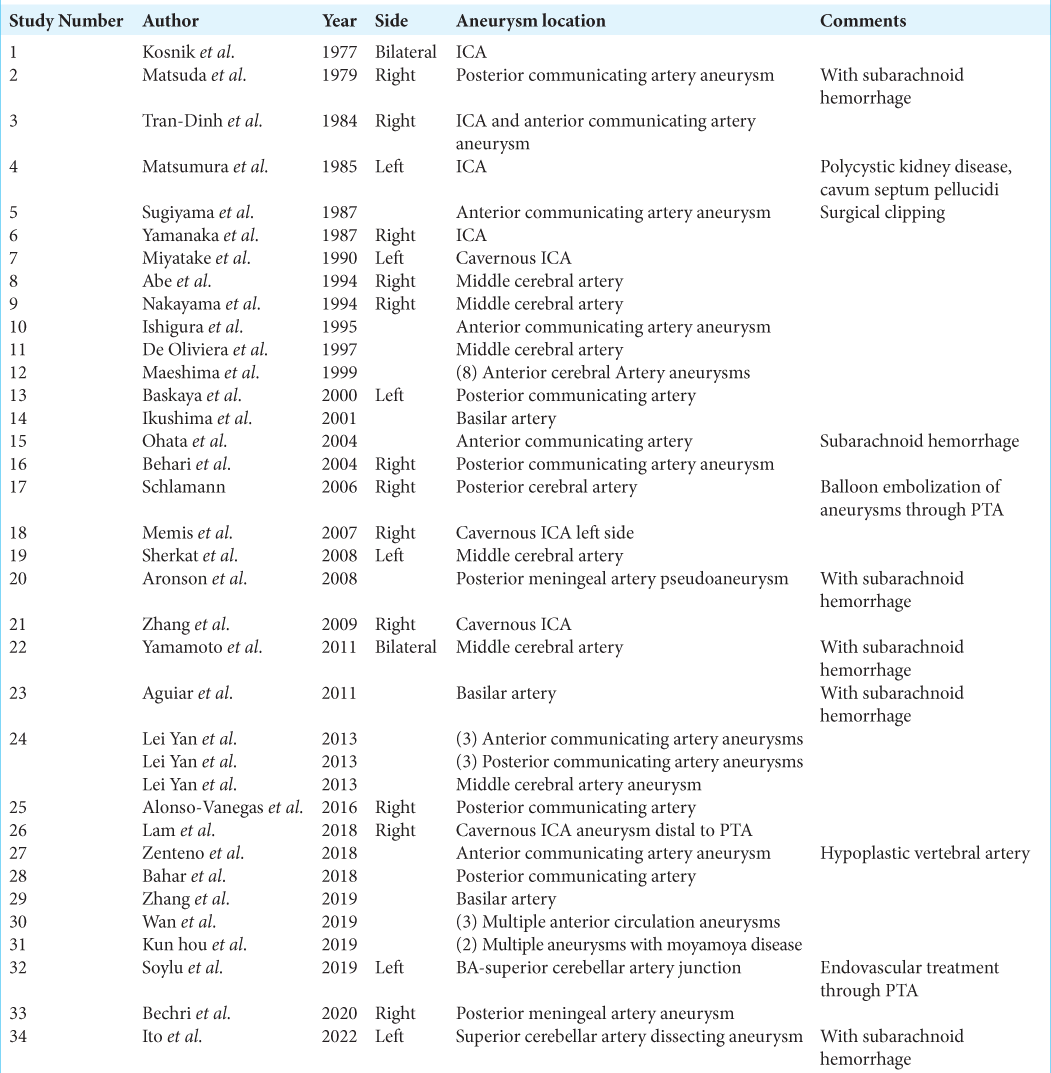
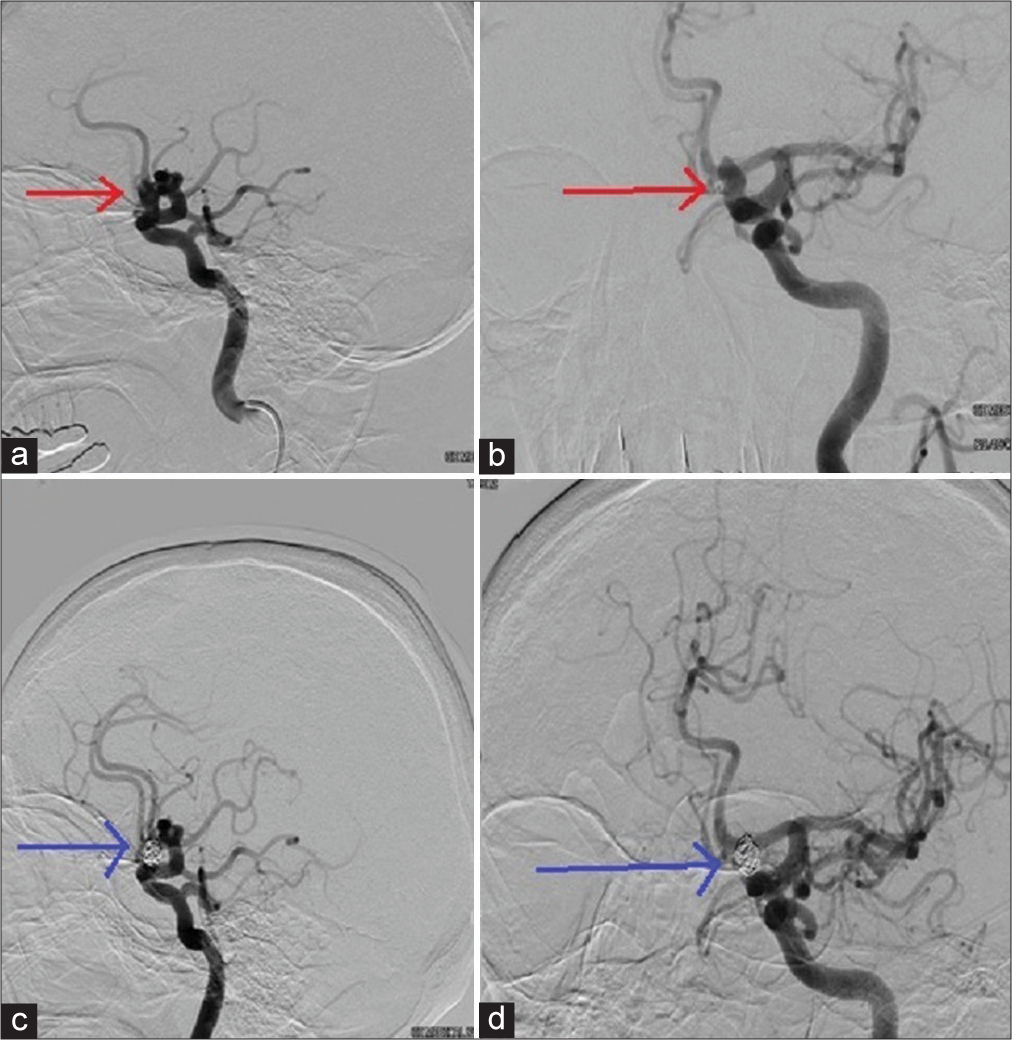
Figure 1:
(a) Early filling of PTA (red arrow) from ICA injection (b) filling of the ophthalmic segment ICA aneurysm (black arrow), PTA (red arrow), and upper extent of basilar artery (c) ICA injection image showing filling of posterior circulation (yellow arrow) through the PTA (d) ICA injection image showing filling of PTA with upper extent of basilar artery (blue arrow) and bifurcation into posterior cerebral arteries (postoperative image with coiled aneurysm seen).
Figure 2:
(a) Subtracted angiography image showing vertebral artery injection filling the PTA (black arrow) and cavernous segment of ICA, (b) sequential angiography image showing filling of ICA ophthalmic segment of ICA and faint filling of aneurysm (red arrow) via the PTA (black arrow), and (c) sequential angiography image showing filling of anterior circulation (black arrow) via PTA, after a vertebral injection.
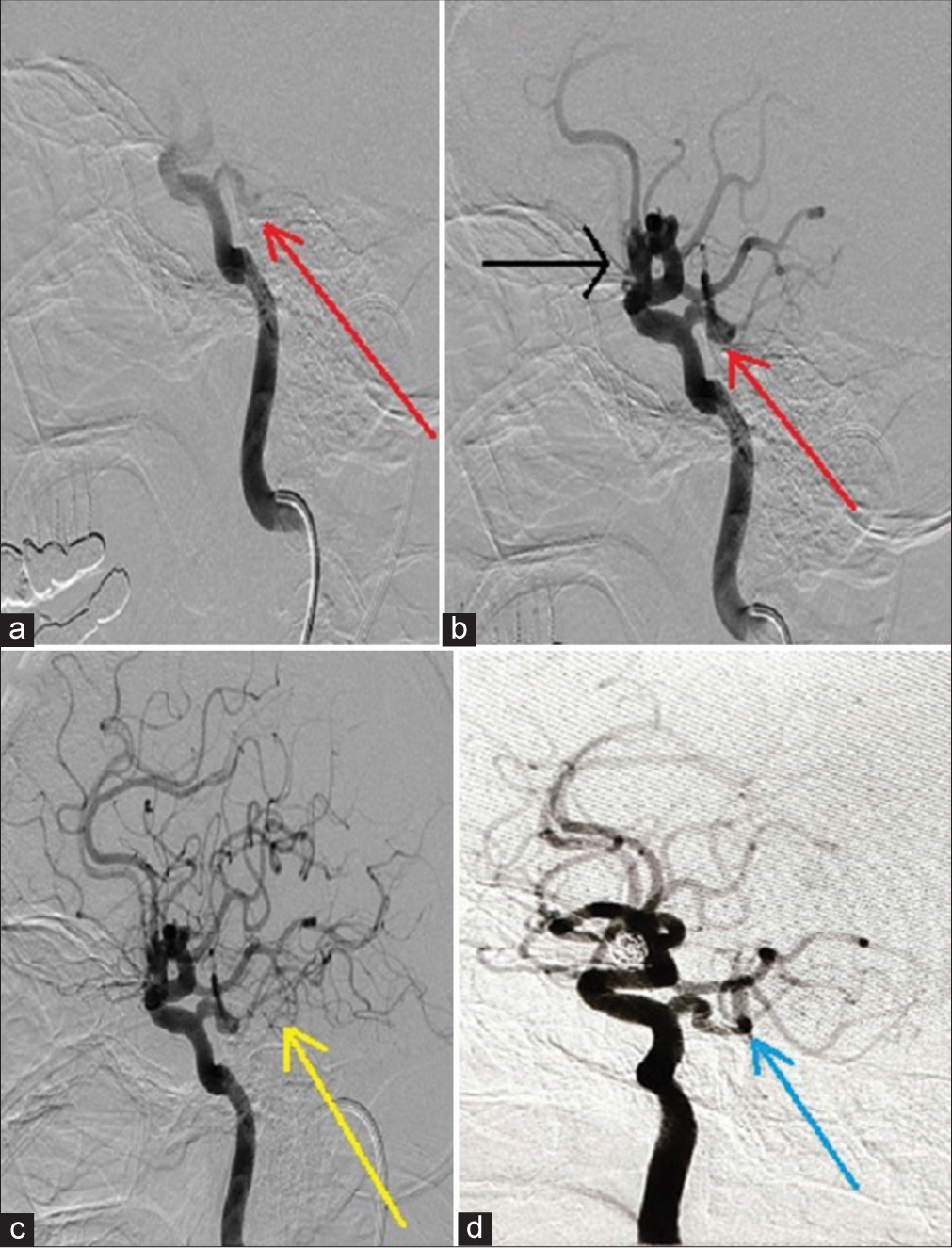
Figure 3:
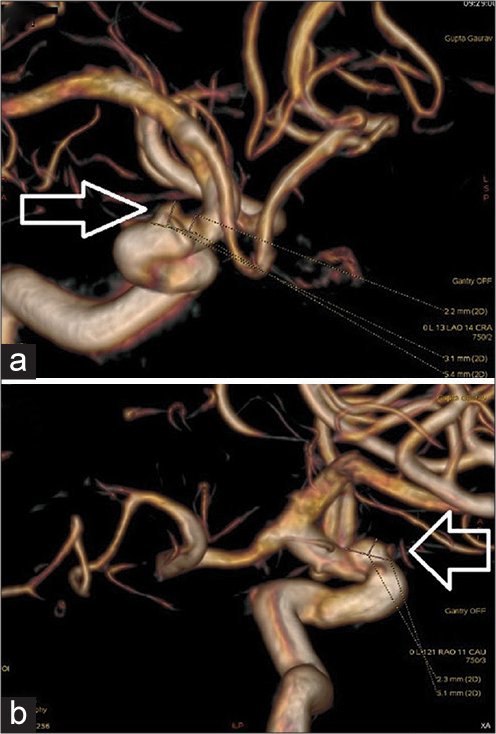
(a) A 3D reconstructed image showing size measurement of the ophthalmic segment ICA aneurysm (hollow white downward arrow) and presence of PTA filling the basilar trunk and bifurcation (solid white arrows) and (b) a 3D reconstructed image showing the saccular morphology of the aneurysm (hollow white arrow).
On performing aortic arch injection, the origin of innominate and left common carotid arteries appeared extremely close. This represented a bovine arch configuration. A direct origin of the vertebral artery from the left aortic arch was also noticed (type III aortic arch). A fetal posterior communicating artery (Pcom) was also present. After appropriate counseling and consent, she underwent therapeutic angiography. A 5 mm × 16 mm size pipeline flex flow diverter device was deployed across the aneurysmal ophthalmic ICA segment [
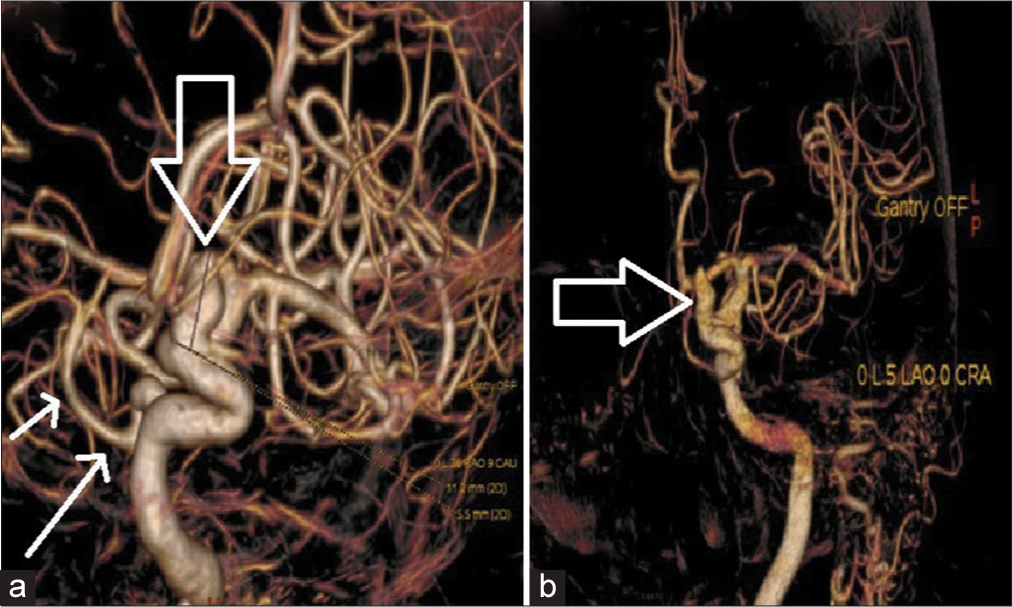
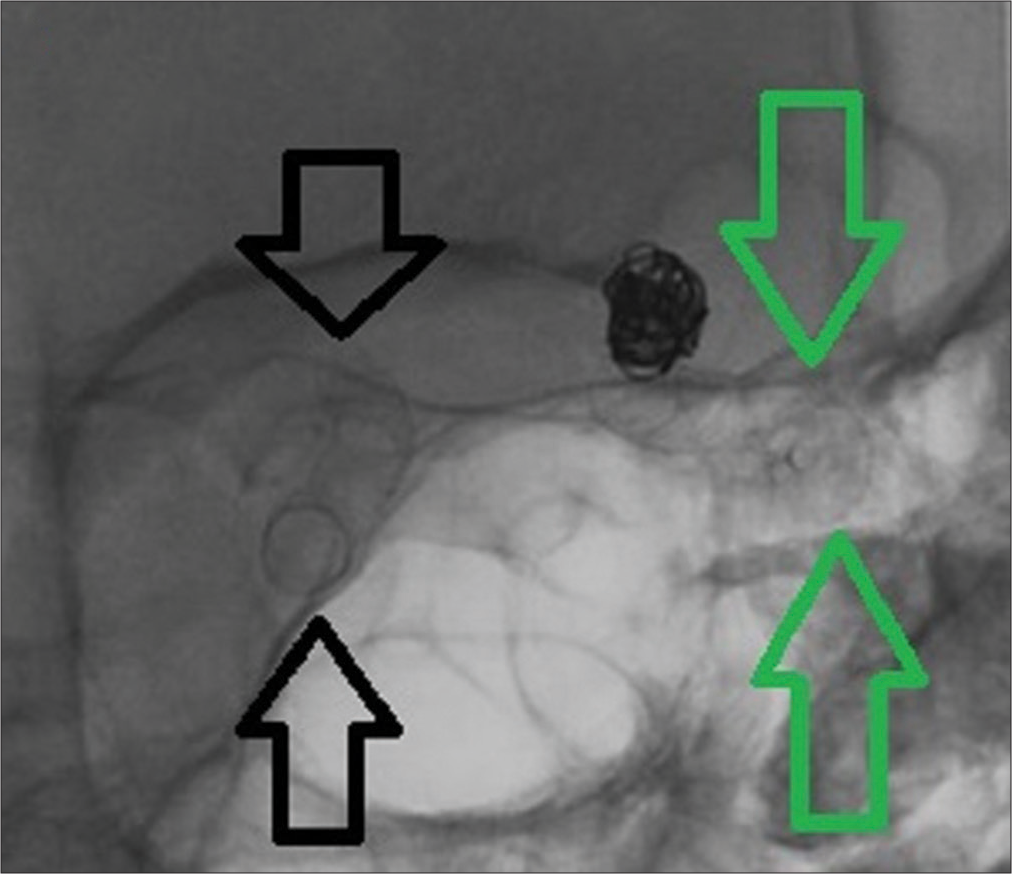
Figure 4:
(a) Unsubtracted angiography image showing presence of pipeline flex flow diverter (hollow black arrow) across ICA ophthalmic segment and presence of coils (red arrow) within the aneurysmal space. The pipeline device is carefully deployed so that it stops distal to the origin of PTA (shown with blue arrow toward the black marker of coil). The proximal end of pipeline device is shown with a solid yellow arrow and (b) solid black arrow has been cited in the text of legend as intact PTA draining into upper basilar trunk and posterior circulation. Blue arrow in figure corresponds to proximal coil marker at the level of origin of PTA from ICA.
A follow-up angiogram at 6 months demonstrated complete occlusion of the left ICA aneurysm [
Figure 5:
(a) Preoperative lateral angiography image showing the ICA aneurysm (red arrow), (b) preoperative anteroposterior view showing the ICA aneurysm (red arrow), and (c) postoperative lateral angiography image showing coiled aneurysm(blue arrow). A doubt of residual filling seen along the anterior border of aneurysm did arise after this image (d) subsequent anteroposterior image showing complete occlusion of the aneurysm (blue arrow) with no residual filling. The doubt of residual filling on lateral image was clarified as an overshadow of anterior cerebral artery circulation here.
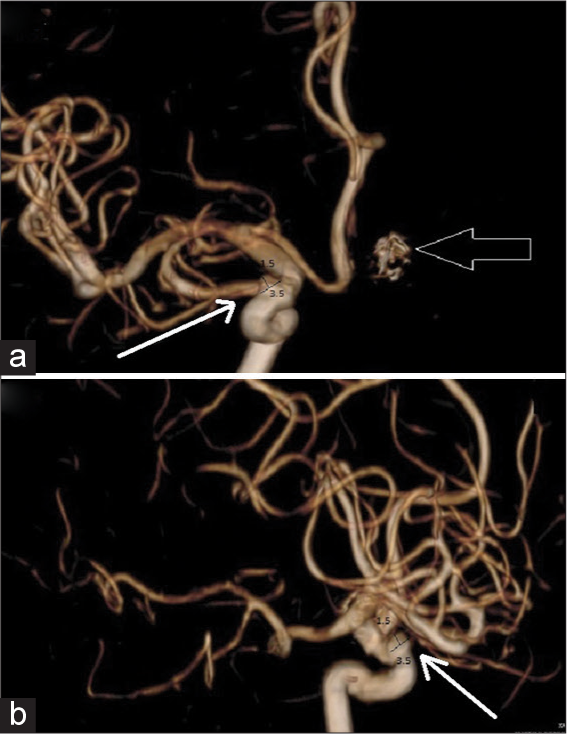
Figure 7:
(3D reconstructed images presented) (a) Morphology of the right ICA ophthalmic segment aneurysm (hollow white arrow) seen in follow-up angiography – two blebs seen measuring 2.2 mm and 3.1 mm and maximum base measurement 5.4 mm and (b) appearance of the right ICA aneurysm (white arrow) as seen with base measurement 5.1 mm.
A single SURPASS flow diverter device measuring 5 mm × 20 mm was placed across the right supraclinoid ICA aneurysm origin [
A 6-month follow-up angiography showed that majority of this new aneurysm was thrombosed, with an extremely small residual 0.9 mm aneurysm on the right side ICA [
DISCUSSION
The most common fetal intracranial anastomosis to survive unto adulthood is the persistent PTA.[
Association of PTA with aneurysms
The presence of aneurysms in patients with PTA is reported around 12–14%.[
Simultaneous occurrence of persistent intersegmental artery with PTA and aneurysm on PTA has been reported.[
We believe that the presence of PTA might alter the flow dynamics of circle of Willis, predisposing to aneurysm formation. Other pathogenic mechanisms of aneurysm formation include hypertension and hemodynamic stress. A PTA represents a developmental structural abnormality. The presence of PTA creates additional hemodynamic stress on ICA and BA. The PTA is a vessel situated in lateral parasellar region usually. Rarely, a medial sphenoidal variant (Salas) may be seen. The latter one may be associated with hypopituitarism. The abnormal origin of PTA from ICA and basilar artery predisposes to two regions of hemodynamic stress – one at the ICA posteromedial wall and one at the anterolateral wall of basilar artery. As per Rhoton’s theory, the presence of additional branch points in a vessel predisposes to aneurysm formation. The standard anatomy of basilar artery consists of two branch points of PCAs, two for superior cerebellar arteries within 5–8 mm of each other. The presence of another branch point within few millimeters of these will definitely cause added hemodynamic stress. The relative frequency of aneurysms near ICA-PTA junction and anterior circle of Willis were more common than near PTA-BA junction and the posterior circle. Of the 50 aneurysms seen in our literature review, majority were localized to ACA/Acom region, while ICA and PCom aneurysms were equal (eight each), and fewer MCA (6), BA (3), PCA (1), and SCA (2) aneurysms were noticed. This indicates an increased hemodynamic stress in the anterior circulation due to the presence of PTA.
The presence of PTA provides additional anatomic weak spots/pressure points: anatomical branch points act as weak pressure points. There are few cadaveric studies which highlight presence on PTA with associated aneurysms. We searched PubMed for 223 articles with key words – PTA, histology, and genetic basis; but none revealed a histological analysis from cadaveric studies. The anatomical composition of a PTA will suggest the fundamental basis of pathologies associated with it. It would be worthwhile to study the histology of PTA vessel wall – the tunica intima, media, and externa. A genetic analysis of the vessel wall would highlight the basic difference between a normal intracranial vessel and persistent carotid basilar anastomotic remnant.[
The location of aneurysm in relation to PTA is a decisive factor for therapy. An aneurysm which involves the ostium of PTA will need careful handling. Risk of occlusion of PTA with coils during endovascular treatment cannot be negated. Prolapse of coils into the parent artery with occlusion of PTA is another risk of treatment. Retrograde filling of aneurysm through a PTA needs to be considered. Simple ligation of aneurysm (while clipping) may not be sufficient when the PTA supplies blood to the aneurysm too.
The physiological significance of PTA depends on the type of circulation. In a fetal type, basilar system and PCAs are supplied by PTA. Occlusion of PTA can be hazardous here. In adult-type circulation, the PTA plays a rudimentary role. Risk of significant clinical consequences is low in this type. In our patient, the flow diverter stent encompassed the origin of PTA. While deploying the stent, it was essential to ensure complete apposition of the stent with endothelium. Precarious density between the endothelium and stent would predispose to thromboembolism of PTA and, hence, ischemia of brainstem perforators. Symptoms of posterior circulation stroke such as distal vertebrobasilar insufficiency will be seen in case of a fetal-type PTA thrombosis.
Association of PTA with stroke
In patients with carotid stenosis and incidental PTAs, posterior circulation ischemic stroke has been reported. PTA may also act as a conduit for superselective catheterization in angiography for stroke.
Association of PTA with trigeminal neuralgia
Symptoms of trigeminal neuralgia have been attributed to a PTA in some patients. Surgical manipulation does provide relief from neuralgic symptoms
Other associations
Several case reports documenting association of PTA with moyamoya disease, aneurysms, hemangiomas, and brain tumors such as medulloblastoma and hemangioblastomas, and other pathologies like arteriovenous malformations have been published.[
Need of surveillance
An important component of the management of patients with incidentally detected PTA is regular periodic follow-up angiography imaging. Appearance of new aneurysms on the PTA trunk, ICA-PTA junction, or BA-PTA junction or anywhere else in the circulation needs to be identified. In our patient with treatment history for two unruptured aneurysms, certain important features were traced on the follow-up angiography. This included detection of new aneurysms, patency of parent vessel with stent in situ, development of in-stent stenosis, thromboembolic occlusion of the PTA/ ophthalmic artery/Pcom artery, or other perforator vessels.
CONCLUSION
Persistence of carotid vertebral anastomosis has been associated with aneurysms in various locations. Histological basis of aneurysm formations remains to be seen. Although papers documenting equivocal presence of aneurysms in the patients with incidental PTA have been published, we report a case where patient develops progression of a newly diagnosed aneurysm. This highlights the heterogeneous nature of aneurysms with PTA as an associated factor. The role of active angiographic surveillance in patients with PTA cannot be undermined. Large-scale studies are needed to clarify the role of screening angiography in this subset of patients.
Consent to participate and publish material
Obtained in written from patient and relatives.
Availability of data and material
Available.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Aguiar GB, Conti ML, Veiga JC, Jory M, Souza RB. Basilar artery aneurysm at a persistent trigeminal artery junction. A case report and literature review. Interv Neuroradiol. 2011. 17: 343-6
2. Azab W, Delashaw J, Mohammed M. Persistent primitive trigeminal artery: A review. Turk Neurosurg. 2012. 22: 399-406
3. Baskaya MK, Roberts R, Rivera E, Nanda A. Persistent primitive trigeminal artery associated with posterior communicating artery aneurysm and hypoplastic vertebral artery. Surg Radiol Anat. 2001. 23: 169-71
4. Cloft HJ, Razack N, Kallmes DF. Prevalence of cerebral aneurysms in patients with persistent primitive trigeminal artery. J Neurosurg. 1999. 90: 865-7
5. Diana F, Mangiafico S, Valente V, Wlderk A, Grillea G, Colonnese C. Persistent trigeminal artery aneurysms: Case report and systematic review. J Neurointerv Surg. 2019. 11: 1261-5
6. Hou K, Ji T, Guo Y, Xu K, Yu J. The coexistence of persistent primitive trigeminal artery, moyamoya disease, and multiple intracranial aneurysms: A case report and literature review. World Neurosurg. 2019. 124: 313-8
7. Ikushima I, Arikawa S, Korogi Y, Uehara H, Komohara Y, Takahashi M. Basilar artery aneurysm treated with coil embolization via persistent primitive trigeminal artery. Cardiovasc Intervent Radiol. 2002. 25: 70-1
8. Ishikawa T, Yamaguchi K, Anami H, Sumi M, Ishikawa T, Kawamata T. Treatment of large or giant cavernous aneurysm associated with persistent trigeminal artery: Case report and review of literature. World Neurosurg. 2017. 108: 996.e11-5
9. Karasawa J, Terano M, Nishikawa M, Kyoi K, Kikuchi H. Case of persistent bilateral carotid-basilar anastomoses (primitive otic artery and primitive trigeminal artery) with multiple cerebrovascular anomalies. No To Shinkei. 1972. 24: 91-8
10. Li MH, Li WB, Pan YP, Fang C, Wang W. Persistent primitive trigeminal artery associated with aneurysm: Report of two cases and review of the literature. Acta Radiol. 2004. 45: 664-8
11. Maeshima S, Tereda T, Masuo O, Nakai K, Itakura T, Komai N. Multiple cerebral aneurysms with persistent primitive trigeminal artery. J Clin Neurosci. 1999. 6: 52-4
12. O’uchi E, O’uchi T. Persistent primitive trigeminal arteries (PTA) and its variant (PTAV): Analysis of 103 cases detected in 16,415 cases of MRA over 3 years. Neuroradiology. 2010. 52: 1111-9
13. Tanaka Y, Hara H, Momose G, Kobayashi S, Kobayashi S, Sugita K. Proatlantal intersegmental artery and trigeminal artery associated with an aneurysm: Case report. J Neurosurg. 1983. 59: 520-3
14. Tubbs RS, Shoja MM, Salter EG, Oakes WJ. Cadaveric findings of persistent fetal trigeminal arteries. Clin Anat. 2007. 20: 367-70
15. Tungaria A, Kumar V, Garg P, Jaiswal AK, Behari S. Giant, thrombosed, sellar-suprasellar internal carotid artery aneurysm with persistent, primitive trigeminal artery causing hypopituitarism. Acta Neurochir (Wien). 2011. 153: 1129-33
16. Ueda T, Goya T, Kinoshita K, Wakuta Y, Mihara K. Multiple anomalies of cerebral vessels. A case of multiple aneurysms associated with fenestration of the middle cerebral artery and persistent primitive trigeminal artery. No Shinkei Geka. 1984. 12: 531-6
17. Wan Z, Meng H, Xu N, Liu T, Chen Z, Zhang Z. Coil embolisation of multiple cerebral aneurysms with lateral Type I persistent primitive trigeminal artery: A case report and literature review. Interv Neuroradiol. 2019. 25: 628-34