- Department of Neurosurgery, School of Medicine, State University of New York at Stony Brook, and ℅ Dr. Marc Agulnick 1122 Frankllin Avenue Suite 106, Garden City, NY 11530, USA
- Department of Orthopedics, NYU Langone Hospital Long Island and St. Francis Hospital, 1122 Franklin Avenue Suite 106, Garden City, NY 11530, New York, United States.
Correspondence Address:
Nancy E. Epstein, M.D, F.A.C.S, Clinical Professor of Neurosurgery, School of Medicine, State University of NY at Stony Brook, NY and ℅ Dr. Marc Agulnick 1122 Frankllin Avenue Suite 106, Garden City, NY 11530, USA.
DOI:10.25259/SNI_541_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein1, Marc A. Agulnick2. Short Review/Perspective on Adjacent Segment Disease (ASD) Following Cervical Fusion Versus Arthroplasty. 22-Jul-2022;13:313
How to cite this URL: Nancy E. Epstein1, Marc A. Agulnick2. Short Review/Perspective on Adjacent Segment Disease (ASD) Following Cervical Fusion Versus Arthroplasty. 22-Jul-2022;13:313. Available from: https://surgicalneurologyint.com/surgicalint-articles/11737/
Abstract
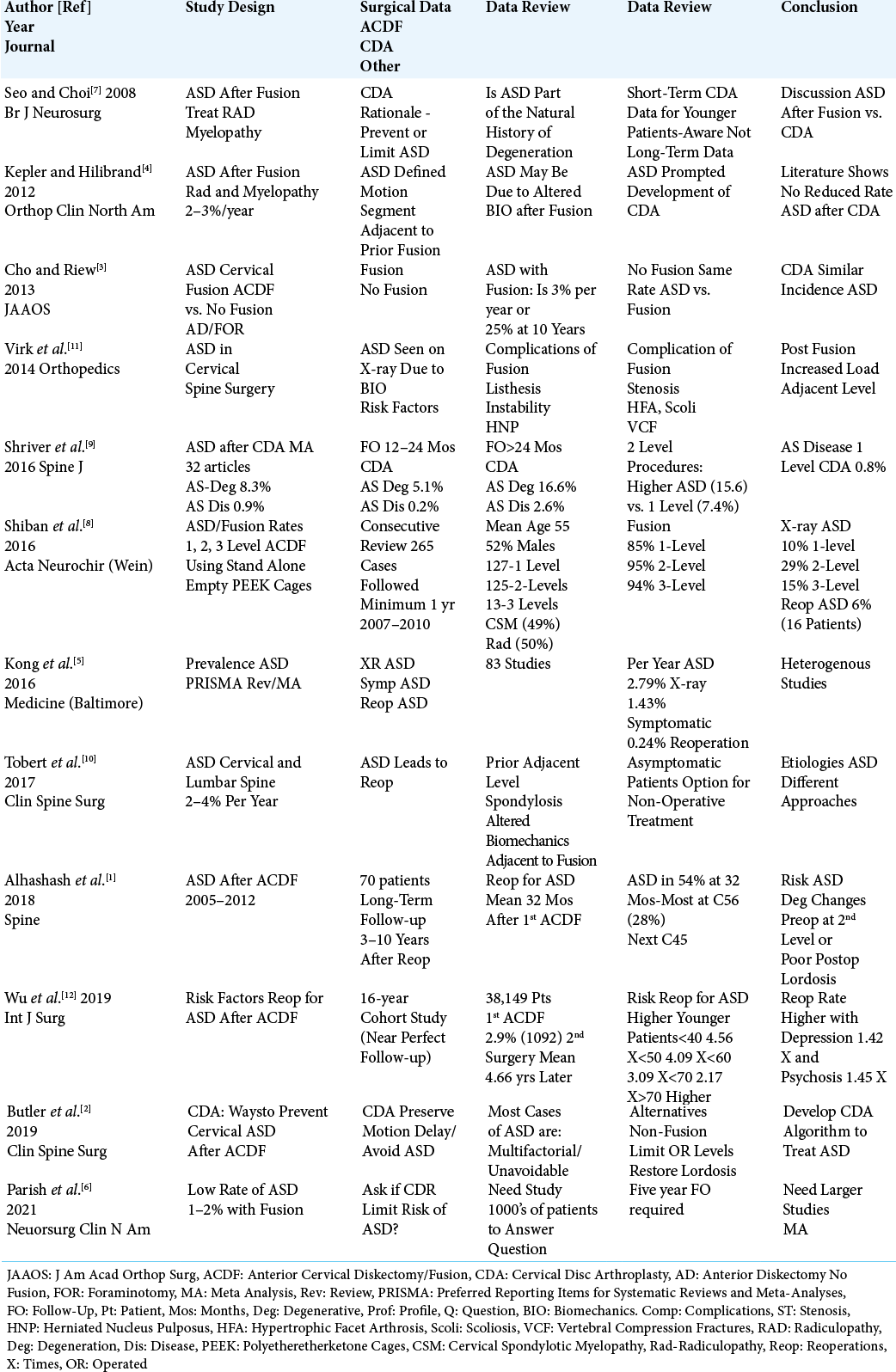
Background: Although the incidence of radiographic Adjacent Segment Disease (ASD) following anterior cervical diskectomy/fusion (ACDF) or cervical disc arthroplasty (CDA) typically ranges from 2-4%/year, reportedly fewer patients are symptomatic, and even fewer require secondary surgery.
Methods: Multiple studies have documented a 2-4% incidence of radiographic ASD following either ACDF or CDA per year. However, fewer are symptomatic from ASD, and even fewer require additional surgery/reoperations.
Results: In a meta-analysis (2016) involving 83 papers, the incidence of radiographic ASD per year was 2.79%, but symptomatic disease was present in just 1.43% of patients with only 0.24% requiring secondary surgery. In another study (2019) involving 38,149 patients undergoing ACDF, 2.9% (1092 patients; 0.62% per year) had radiographic ASD within an average of 4.66 postoperative years; the younger the patient at the index surgery, the higher the reoperation rate (i.e.
Conclusion: The incidence of radiographic ASD ranges from 2-4% per year for ACDF and CDA. Additionally, both demonstrate lesser frequencies of symptomatic ASD, and the need for secondary surgery. Further, doubling the frequency of ASD following 2 vs. 1-level CDA, should prompt surgeons to limit surgery to only essential levels.
Keywords: Adjacent Segment Disease (ASD), Cervical Spine, Surgery: Cervical Disc Arthroplasty (CDA), Anterior Cervical Diskectomy/Fusion (ACDF), Radiographic ASD, Symptomatic ASD: ASD Requiring Reoperations
INTRODUCTION
The incidence of radiographic Adjacent Segment Disease (ASD) following cervical spine surgery, whether following anterior diskectomy/fusion (ACDF) or cervical disc arthroplasty (CDA), typically ranges from 2-4%/year [
DEFINITION OF ASD
Virk et al. (2014) defined the various degenerative, radiographic, and/or biomechanical factors predisposing patients to the development of ASD [
INCIDENCE OF ASD AFTER CERVICAL SURGERY
Several studies cited 2–4% frequencies of ASD following ACDF, with some also citing comparable rates with non-fusion techniques [
REDUCING THE RISKS AND/OR PREVENTION OF ASD FOLLOWING CERVICAL SURGERY
Several cervical spine studies, mostly involving ACDF, identified risk factors predisposing patients to developing radiographic ASD, symptomatic ASD, and the need to reoperate on ASD [
ACDF Data Largely Excluded ASD Results with Polyetheretherketone (PEEK) Cages
Notably, we did not specifically focus on the results for ACDF performed with stand-alone polyetheretherketone (PEEK) cages. In Shiban et al. (2016), one year following 265 PEEK cage fusions, 16 (6%) warranted reoperation to address radiographic ASD [
CDA’S “BIOMECHANICAL MOTION SPARING” DESIGN FAILED TO REDUCE ASD
CDA’s, by maintaining “motion” at operated levels, were devised to “theoretically” reduce stress transmitted to adjacent segments [
CDA’S COMPARABLE ADJACENT SEGMENT DEGENERATION (AS-DEG) VS. ADJACENT SEGMENT DISEASE (AS-DIS) VS. ANTERIOR CERVICAL FUSIONS
Two studies emphasized that CDA’s failed to limit or eliminate ASD when compared with largely anterior cervical fusions [
CONCLUSION
This short review/perspective of select studies emphasizes how to limit the risk of adjacent segment degeneration (i.e. radiographic, symptomatic, and/or requiring reoperations). This requires; carefully selecting “symptomatic” patients for either ACDF or CDA (i.e., for CDA, younger patients with preserved range of motion without spondylosis), stringently limiting the number of operated levels, and optimizing the surgical “technique” to preserve lordosis.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Professor Department of Neurosurgery, Medical College of Wisconsin, Milwaukee, WI
The FEM stuff we have been doing goes well with this report showing adjacent level stresses throughout the spine with both ACDF and CDA. The Metal on Polymer CDA such as Prestige are stiffer and would be predicted to increase ASD more than a metal on Polymer (Secure- C, Prodisc-C, Mobi-C). These more mobile disc arthroplasties shift the stresses to the index level along the facets. The newer discs like Simplify with different core biomaterials will hopefully “soften” the construct and produce less ASD.
I agree with the “natural history of ASD” and often think of the A as standing for accelerated- both ACDF and CDA -accelerating a natural history. Seems like it boils down to whether you are treating radiculopathy or myelopathy and what is the least procedure a surgeon can do to achieve symptomatic relief without triggering the degenerative cascade. The posterior minimally invasive foraminotomy will be making a comeback in the near future.
References
1. Alhashash M, Shousha M, Boehm H. Adjacent segment disease after cervical spine fusion: evaluation of a 70 patient long-term follow-up. Spine. 2018. 43: 605-9
2. Butler JS, Morrissey PB, Wagner SC, Kaye ID, Sebastian AS, Schroeder GD. Surgical strategies to prevent adjacent segment disease in the cervical spine. Clin Spine Surg. 2019. 32: 91-7
3. Cho SK, Riew DK. Adjacent segment disease following cervical spine surgery. J Am Acad Orthop Surg. 2013. 21: 3-11
4. Kepler CK, Hilibrand AS. Management of adjacent segment disease after cervical spinal fusion. Orthop Clin North Am. 2012. 43: 53-62
5. Kong L, Cao J, Wang L, Shen Y. Prevalence of adjacent segment disease following cervical spine surgery: A PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore). 2016. 95: e4171
6. Parish JM, Asher AM, Coric D. Adjacent-segment disease following spinal arthroplasty. Neurosurg Clin N Am. 2021. 32: 505-10
7. Seo M, Choi D. Adjacent segment disease after fusion for cervical spondylosis; myth or reality J Neurosurg. 2008. 22: 195-9
8. Shiban E, Gapon K, Wostrack M, Meyer B, Lehmberg J. Clinical and radiological outcome after anterior cervical diskectomy and fusion with stand-alone empty polyetheretherketone (PEEK) cages. Acta Neurochir (Wien). 2016. 158: 349-55
9. Shriver MF, Lubelski D, Sharma AM, Steinmetz MP, Benzel EC, Mroz TE. Adjacent segment degeneration and disease following cervical arthroplasty: A systematic review and meta-analysis. Spine J. 2016. 16: 168-81
10. Tobert DG, Antoci V, Patel SP, Saadat E, Bono CM. Adjacent segment disease in the cervical and lumbar spine. Clin Spine Surg. 2017. 30: 94-101
11. Wu JC, Chang HK, Huang WC, Chen YC. Risk factors of second surgery for adjacent segment disease following anterior cervical discectomy and fusion: A 16-year cohort study. Int J Surg. 2019. 68: 48-55
12. Virk SS, Niedermeier S, Yu E, Khan SN. Adjacent segment disease. Orthopedics. 2014. 37: 547-55