- Pars Advanced and Minimally Invasive Medical Manners Research Center, Pars Hospital, Iran University of Medical Sciences, Tehran, Iran.
Correspondence Address:
Abolfazl Rahimizadeh, Pars Advanced and Minimally Invasive Medical Manners Research Center, Iran University of Medical Sciences, Tehran, Iran.
DOI:10.25259/SNI_1258_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Abolfazl Rahimizadeh, Housain Soufiani, Mahan Amirzadeh, Walter L. Williamson. Six cases of occult sacral meningocele. 11-Mar-2022;13:91
How to cite this URL: Abolfazl Rahimizadeh, Housain Soufiani, Mahan Amirzadeh, Walter L. Williamson. Six cases of occult sacral meningocele. 11-Mar-2022;13:91. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11431
Abstract
Background: Intrasacral occult sacral meningoceles (OSM) are uncommon congenital lesions that rarely become symptomatic, even over a patient’s life time.
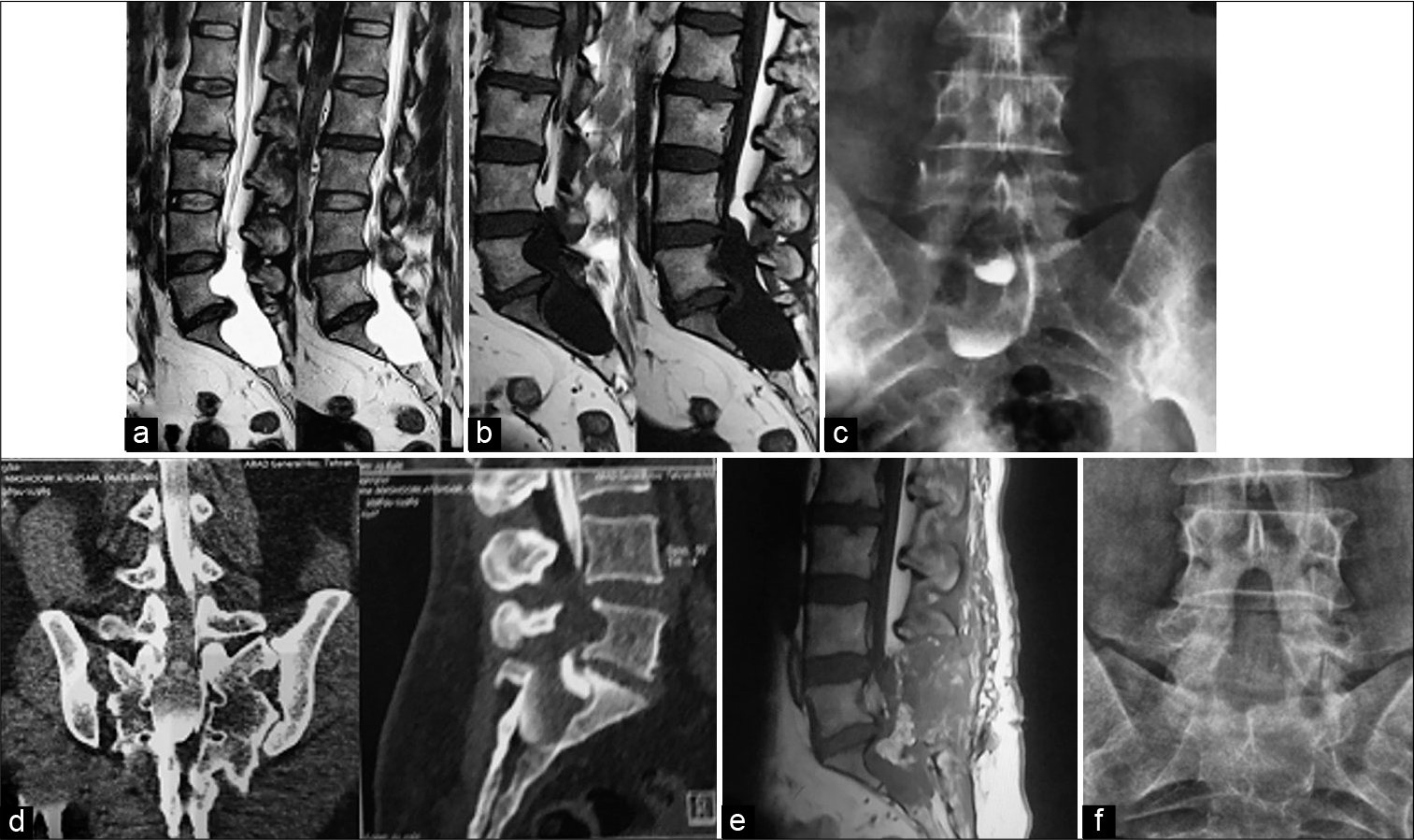
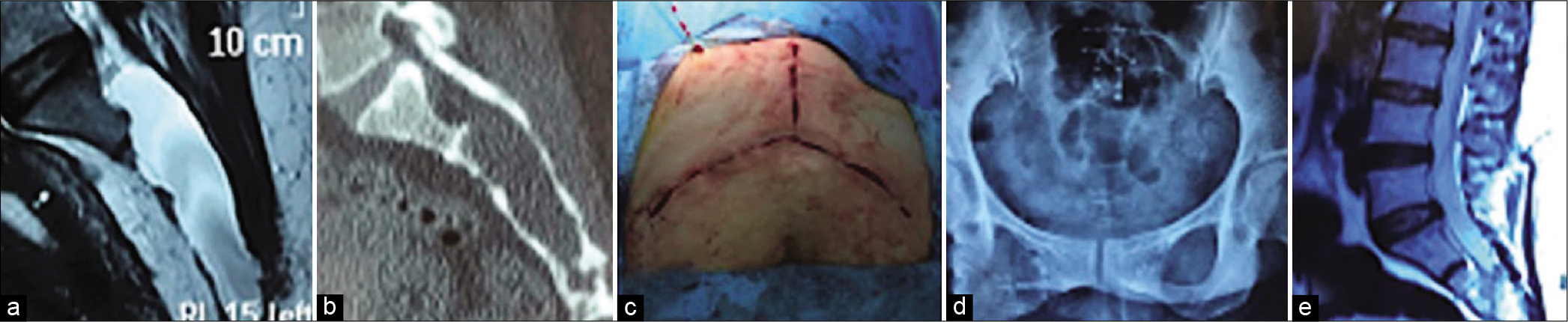
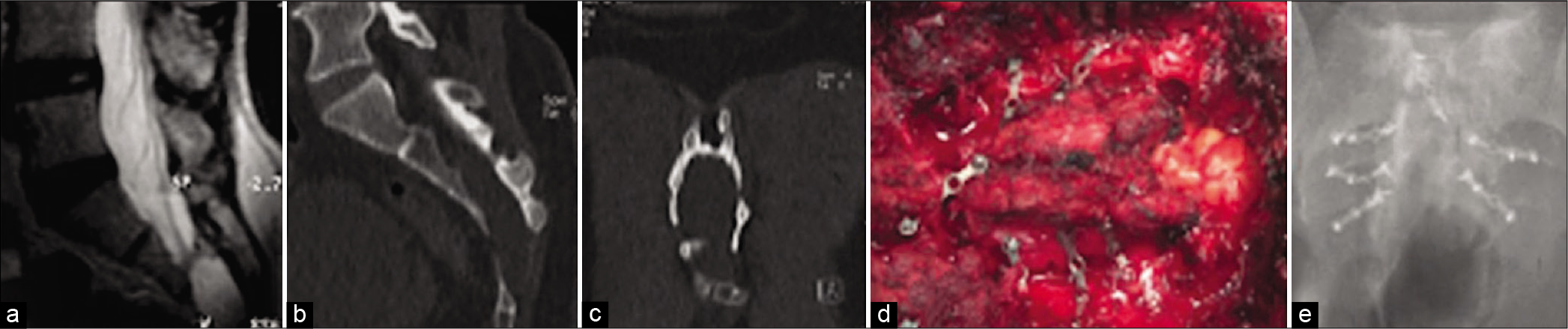
Methods: We operated on six patients with symptomatic OSM diagnosed on MR studies (all six) and/or CT examinations (four cases).
Results: All six patients had uneventful postoperative recoveries. Nevertheless, despite the resolution of low back pain and radiculopathy, preoperative bladder dysfunction improved postoperatively in only one patient.
Conclusion: Few cases of patients undergoing surgery for symptomatic OSM are reported in the literature. Here, we recount our experience with six patients with symptomatic OSM who demonstrated significant postoperative neurological recoveries except for rare improvement in bladder function.
Keywords: Extradural arachnoid cyst, Low back pain, Meningocele, Occult sacral, Sacrum
INTRODUCTION
Occult sacral meningoceles (OSM) are cerebrospinal fluid (CSF) containing cystic masses that are typically devoid of neural elements.[
MATERIALS AND METHODS
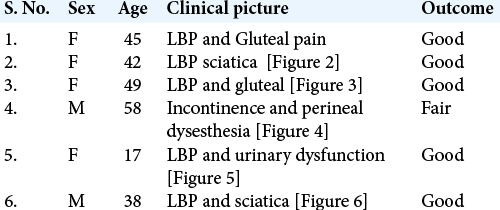
Six patients, including four females and two males ranging in age from 17 to 58 (mean of 41.5), presented with OSM [
Figure 1:
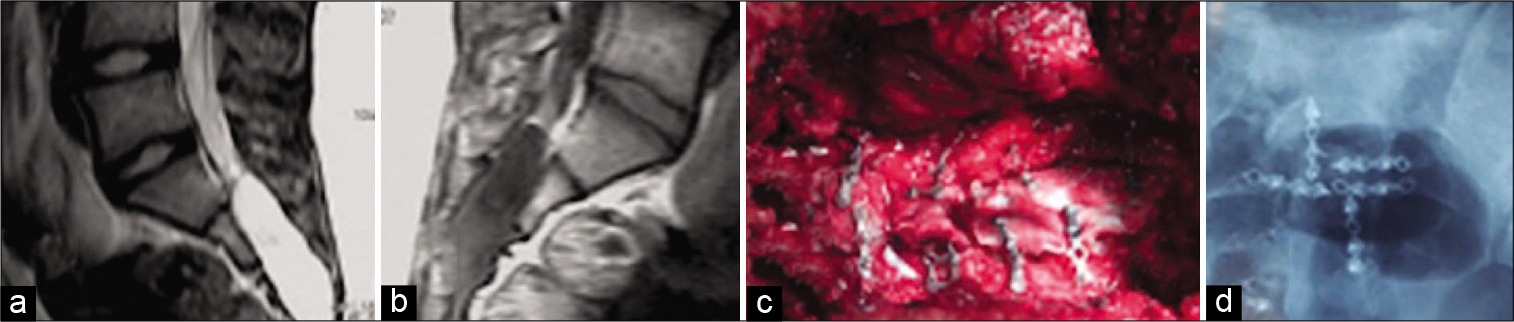
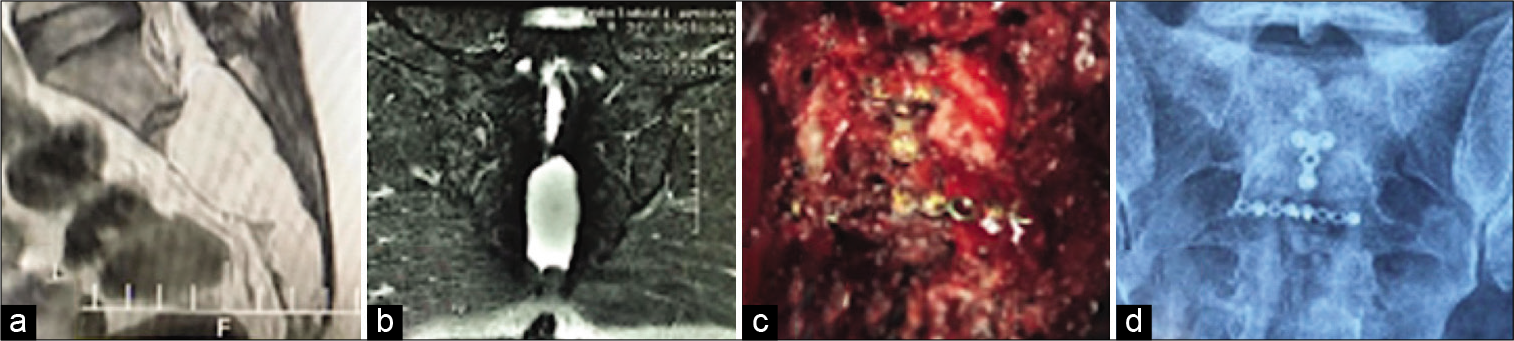
Lumbosacral sagittal MRI showing a cystic mass from L5 to S3; (a) hyperintense on T2-weighted; (b) hypointense in T2-weighted; (c) lumbosacral delayed myelogram shows dye at the bottom of the cyst; (d) CT myelogram demonstrate block of dye at L5 level and dye at the bottom of the cyst; (e) postoperative T2-weighted sagittal MRI, no fluid in the sacrum, hyperintensity is due to free fat graft; and (f) postoperative lumbosacral AP radiograph; note repair of the sacral roof.
RESULTS
All six patients had an uneventful postoperative course. Low back pain and radiculopathy resolved in all patients, but bladder dysfunction remained in five of the six.
Illustrative case
A 45-year-old female with the lower back and right radiculopathy of 4 month’s duration was diagnosed with an OSM based on X-ray, MR, and CT-myelographic studies. X-rays displayed scalloping of the sacrum. The MRI revealed a well-defined intrasacral cystic lesion (hypointense in T1 and hyperintense on T2-weighted images), extending from L5 to S3 with scalloping and thinning of the sacrum [
DISCUSSION
OSMs enlarge with time and often fill the sacral cavity.[
Imaging: X-rays, MR, and CT-myelo-CT studies
Plain X-rays of the sacrum typically demonstrate enlargement of the sacral canal with thin and scalloped walls.[
Management
We prefer the reverse Y skin incision to achieve maximum blood flow to the skin while facilitating the small en block laminoplasty/laminotomy. The OSM’s cyst wall should be incised and aspirated (i.e., demonstrating of CSF), and then followed by, water tight closure of the ostium.[
CONCLUSION
Intrasacral occult meningoceles should be considered among the differential diagnoses for patients presenting with the lower back pain, radiculopathy, perineal dysesthesia, and urinary/fecal dysfunction/incontinence in both adolescence and adulthood.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bozkurt M, Kahilogullari G, Eroglu U, Erdem A. Giant intrasacral meningocele: A case report. Childs Nerv Syst. 2013. 29: 2123-5
2. Doty JR, Thomson J, Simonds G, Rengachary SS, Gunby EN, Nabors MW. Occult intrasacral meningocele: Clinical and radiographic diagnosis. Neurosurgery. 1989. 24: 616-25
3. Enderle C. Occult sacral meningocele (Recealed with Myelography). Riv Neurol. 1932. 5: 418-23
4. Feigenbaum F. Giant sacral meningeal diverticulum containing a thickened filum with lipoma in an adult with spinal cord tethering. Case report and review of the literature. J Neurosurg Spine. 2008. 9: 281-2
5. Hamamcioglu MK, Hicdonmez T, Kilincer C, Cobanoglu S. Intrasacral extradural arachnoid cysts-three case reports. Neurol Med Chir (Tokyo). 2008. 48: 223-6
6. Huang SL, Jiang HX, Cheng B, Ning N, He XJ. Characteristics and management of occult intrasacral extradural cyst in children. Br J Neurosurg. 2013. 27: 509-12
7. Lohani S, Rodriguez DP, Lidov HG, Scott RM, Proctor MR. Intrasacral meningocele in the pediatric population. J Neurosurg Pediatr. 2013. 11: 615-22
8. Muthukumar N. Sacral extradural arachnoid cyst: A rare cause of low back and perineal pain. Eur Spine J. 2002. 11: 162-6
9. Nishio Y, Hamada H, Kurimoto M, Hayashi N, Hirashima Y, Endo S. A case of accoult intrasacral meningocele presented with atypical bowel symptoms. Childs Nerv Syst. 2004. 20: 65-7