- REHAB Basel, Clinic for Neurorehabilitation and Paraplegiology, Basel, Switzerland,
- Department of Radiology, Division of Diagnostic and Interventional Neuroradiology, University Hospital Basel, Basel, Switzerland,
- Department of Neurology, University Hospital Basel, Basel, Switzerland.
Correspondence Address:
Christian Saleh, M.D. (Neurologist) Department of Neurology, REHAB Basel, Clinic for Neurorehabilitation and Paraplegiology, Basel, Switzerland.
DOI:10.25259/SNI_893_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Petros Angelidis1, Christian Saleh1, Phillip Jaszczuk1, Muhannad Seyam2, Katarina Alexandra Ebner3, Margret Hund-Georgiadis1. SMART Syndrome (Stroke-like migraine attacks after radiation therapy): When to suspect it?. 16-Nov-2021;12:561
How to cite this URL: Petros Angelidis1, Christian Saleh1, Phillip Jaszczuk1, Muhannad Seyam2, Katarina Alexandra Ebner3, Margret Hund-Georgiadis1. SMART Syndrome (Stroke-like migraine attacks after radiation therapy): When to suspect it?. 16-Nov-2021;12:561. Available from: https://surgicalneurologyint.com/surgicalint-articles/11228/
Abstract
Background: Stroke-like migraine attacks after radiation therapy (SMART) syndrome is a benign complication of brain radiation therapy, which presents circa a decade after radiation treatment. Symptoms are stroke-like deficits, epileptic seizures, and migraine. Cranial magnetic resonance imaging is characteristic for alterations in the form of unilateral cortical hyperintensities and gyriform enhancement, most prominent in the parieto-occipital regions. Prompt diagnosis is essential to avoid unnecessary investigations (e.g., brain biopsy and angiography).
Case Description: We describe a 51-year-old female patient treated initially with cranial irradiation for a left-sided occipital metastatic lung adenocarcinoma. Five years later, she presented with migraine headache, aphasia, and a right sided hemiparesis.
Conclusion: The triad of migraine, seizure, and hemiparesis within the context of a prior brain radiotherapy should promptly raise the suspicion of SMART syndrome. Prompt diagnosis is essential to avoid unnecessary invasive investigations.
Keywords: Diagnostic work-up, Epileptic seizure, Migraine, Radiation therapy, Stroke
INTRODUCTION
Stroke-like migraine attacks after radiation therapy (SMART) syndrome is a late, but benign complication of brain radiation therapy.[
CASE DESCRIPTION
In 2009, a 51-year-old female patient was treated with cranial irradiation for a left-sided occipital metastatic lung adenocarcinoma. Four years later, in 2013, a further surgical intervention was necessary to remove a radiation-induced tumor necrosis. One year later, she presented with migraine headache, aphasia, and a right-sided hemiparesis. An electroencephalogram showed nonconvulsive status epilepticus. Treatment with lacosamide and levetiracetam was initiated. In 2020, hospitalization was necessary due to hip fracture. The patient again presented during this latter hospitalization with aphasia and a right-sided hemiparesis, which possibly caused a fall and consequently the hip fracture. Due to the patient’s aphasia, no conclusive anamnesis was available.
Based on her previous history, an epileptic event was suspected. Her antiepileptic medication was increased without improving her clinical status. Cranial MRI (cMRI) was performed to rule out an ischemic or hemorrhagic event. Instead, cMRI showed gyriform contrast enhancement within the left parieto-occipital regions. These changes were exclusively localized in the areas irradiated in 2009. Based on her clinical presentation (migraine, seizure, and hemiparesis), as well as on the morphology and location of the MRI alterations [thick gyriform enhancement,
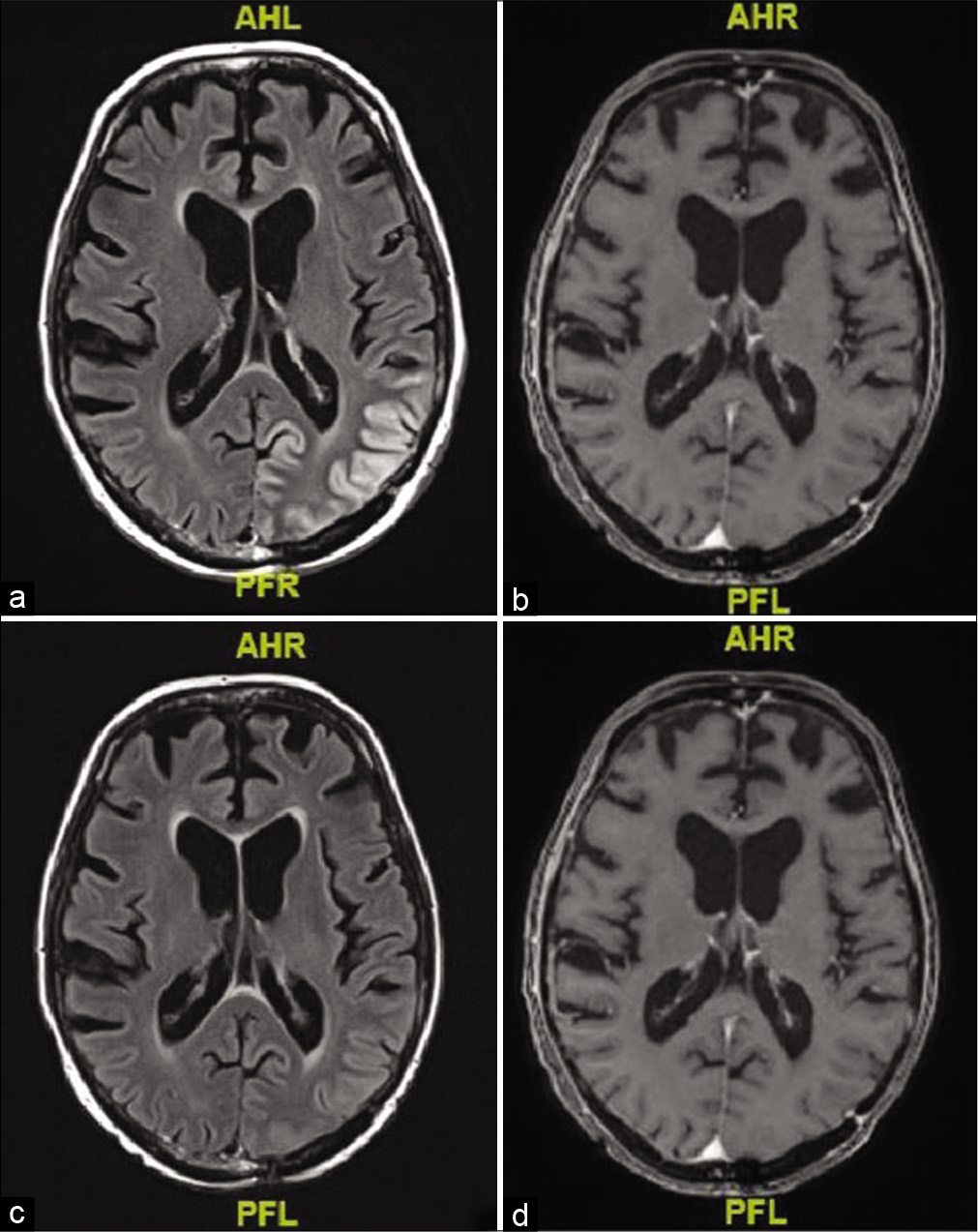
Figure 1:
Brain MRI at presentation and after 10 days of SMART syndrome. Gyral enhancement of the left parietooccipital region with mild swelling on axial postcontrast FLAIR MRI (a) and on postcontrast T1-weighted imaging (b). Complete resolution of findings 10 days later on postcontrast FLAIR (c) and postcontrast T1-weighted imaging (d).
DISCUSSION
SMART syndrome presents with a plethora of symptoms ranging from migraine and seizures to hemiparesis. Other conditions may present with similar symptoms, such as hemiplegic migraine,[
Take-home points
SMART syndrome is a clinicoradiologic diagnosis based on a history of brain irradiation, clinical symptoms, and characteristic MRI findings (see points 2 and 3). The triad of migraine, seizure, and hemiparesis within the context of a prior brain radiotherapy should promptly raise the suspicion of SMART syndrome. cMRI shows characteristic alterations in the form of unilateral cortical hyperintensities and gyriform enhancement, most prominent in the parieto-occipital regions. SMART syndrome can be self-limiting. Treatment is symptomatic (e.g., seizure control). Supplemental steroid therapy may prove beneficial. Prompt diagnosis is essential to avoid unnecessary investigations (e.g., brain biopsy and angiography).
Data availability statement
All data analyzed for this case report are included in this article and its supplementary material files. Further enquiries can be directed to the corresponding author.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
There is no specific funding source, but was performed as part of the employment of the authors. Authors Angelidis, Saleh, Jaszczuk, and Hund-Georgiadis are employed by the REHAB Basel, Clinic for Neurorehabilitation and Paraplegiology, Basel, Switzerland, and authors Seyam and Ebner by the University Hospital Basel, Basel, Switzerland.
Conflicts of interest
There are no conflicts of interest.
References
1. Black DF, Morris JM, Lindell EP, Krecke KN, Worrell GA, Bartleson JD. Stroke-like migraine attacks after radiation therapy (SMART) syndrome is not always completely reversible: A case series. AJNR Am J Neuroradiol. 2013. 34: 2298-303
2. Makary MS, Awan U, Puduvalli VK, Slone HW. Stroke-like migraine attacks after radiation therapy syndrome: Clinical and imaging characteristics. J Clin Imaging Sci. 2019. 9: 5
3. Saleh C, Pierquin G, Beyenburg S. Hemiplegic migraine presenting with prolonged somnolence: A case report. Case Rep Neurol. 2016. 8: 204-10
4. Singh AK, Tantiwongkosi B, Moise AM, Altmeyer WB. Stroke-like migraine attacks after radiation therapy syndrome: Case report and review of the literature. Neuroradiol J. 2017. 30: 568-73
5. Sudulagunta SR, Sodalagunta MB, Kumbhat M, Settikere Nataraju A. Posterior reversible encephalopathy syndrome(PRES). Oxf Med Case Reports. 2017. 2017: omx011