- Department of Neurosurgery, David Geffen School of Medicine, University of California, Los Angeles, California, USA
Correspondence Address:
Tianyi Niu
Department of Neurosurgery, David Geffen School of Medicine, University of California, Los Angeles, California, USA
DOI:10.4103/sni.sni_211_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tianyi Niu, Alexander M. Tucker, Daniel T. Nagasawa, Marvin Bergsneider. Solitary Aggregatibacter aphrophilus tectal abscess in an immunocompetent patient. 24-Oct-2017;8:257
How to cite this URL: Tianyi Niu, Alexander M. Tucker, Daniel T. Nagasawa, Marvin Bergsneider. Solitary Aggregatibacter aphrophilus tectal abscess in an immunocompetent patient. 24-Oct-2017;8:257. Available from: http://surgicalneurologyint.com/surgicalint-articles/solitary-aggregatibacter-aphrophilus-tectal-abscess-in-an-immunocompetent-patient/
Abstract
Background:A solitary abscess involving the tectum, specifically by Aggregatibacter aphrophilus, is an extremely rare condition with no known reported cases to date.
Case Description:Here, we present a case of isolated solitary midbrain tectum abscess in an immunocompetent 28-year-old male who was empirically diagnosed as a primary tectal tumor at an outside hospital where he also underwent placement of a ventriculoperitoneal shunt (VPS) for obstructive hydrocephalus. Eight weeks later he was readmitted with a VPS infection. He was transferred to our institution where the VPS was removed and he was started on broad-spectrum antibiotics. Cerebrospinal fluid (CSF) culture revealed A. aphrophilus. All other workup was negative for infectious etiologies. The tectal lesion completely resolved after 15 weeks of intravenous ceftriaxone without surgical aspiration.
Conclusion:We suggest that an empiric diagnosis of tectal glioma should be made with caution for a ring-enhancing mass. CSF should be routinely cultured at the time of operative diversion if abscess is a possibility.
Keywords: Aggregatibacter aphrophilus, brainstem abscess, differential diagnosis, solitary brain abscess, tectum
INTRODUCTION
Solitary brainstem abscess is a rare diagnosis, with an incidence of less than 0.5% at large tertiary referral centers. Risk factors include right–left heart shunting, immunosuppression, congenital heart disease, and endocarditis, with the causative organism most commonly identified as Streptococcus or Staphylococcus.[
CASE REPORT
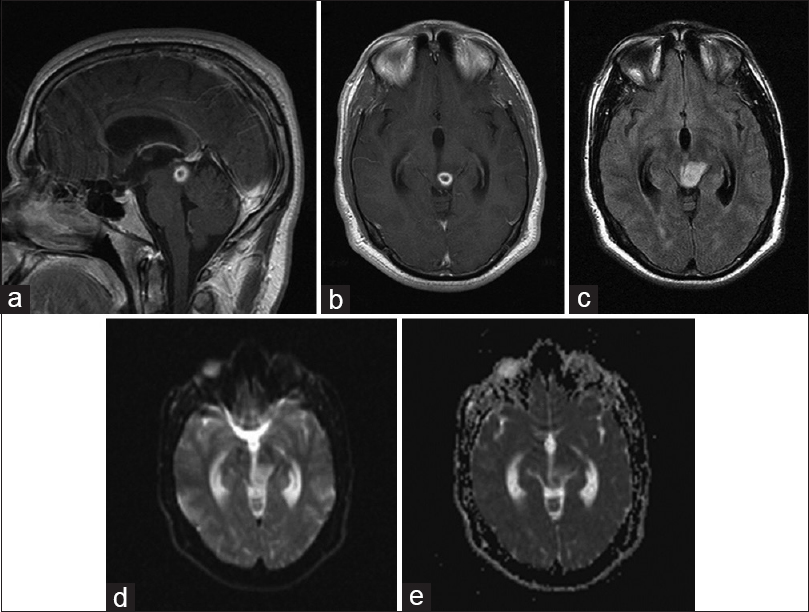
An immunocompetent 28-year-old male was empirically diagnosed with a primary tectal tumor at an outside hospital; his history was negative for intravenous drug use or significant systemic bacterial infection. He presented initially with progressive intermittent headache for more than 6 months. Initial magnetic resonance imaging (MRI) showed a 10 mm × 9 mm left midbrain tectum ring-enhancing lesion with associated surrounding edema and mild hydrocephalus [
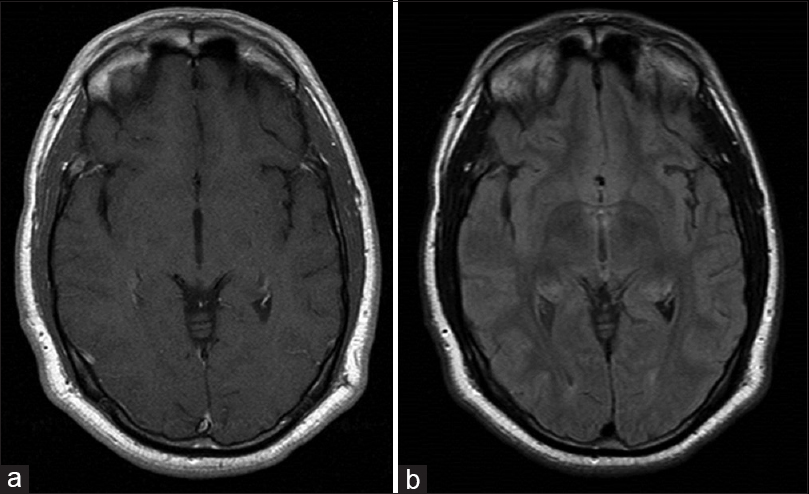
Eight weeks later, he started to have worsening headache, nausea, and intermittent vomiting. He was readmitted with a VPS infection and an abdominal pseudocyst. He was transferred to our institution where the VPS was removed, an external ventriculostomy was placed, and he was started on intravenous ceftriaxone and vancomycin. Cerebrospinal fluid (CSF) profile showed elevated white blood cell (WBC) count of 482 with lymphocyte predominance, suggesting a chronic infection; CSF culture revealed A. aphrophilus. His other workup including blood cultures and transthoracic echocardiogram were negative for infectious etiologies. He slowly improved with antibiotic treatment and was weaned off the ventriculostomy after 14 days, without any subsequent recurrence of hydrocephalus. Vancomycin was stopped after 10 days when the culture finalized A. aphrophilus sensitive to ceftriaxone. The tectal lesion completely resolved after 15 weeks of intravenous ceftriaxone [
DISCUSSION
Solitary brainstem abscess is a rare event,[
Differential diagnosis of enhancing tectal lesions includes abscess, primary brain tumors, lymphoma, or metastatic disease. MRI imaging, particularly diffusion-weighted imaging, can accurately diagnosis brain abscess in a majority of cases.[
Although definitive treatment remains controversial, ranging from antibiotics alone[
In our case, A. aphrophilus was isolated from CSF. It is a fastidious, gram-negative, oxidase-negative, catalase-negative coccobacillus.[
CONCLUSION
A high index of suspicion for brain abscess should be considered in a patient with an enhancing tectal lesion, particularly if the DWI shows homogenous restricted diffusion. Diagnosis involves microbiologic culture, which should be kept for at least 14 days to avoid missing slow-growing bacteria such as A. aphrophilus. For tectal lesions, hydrocephalus must be promptly treated with CSF diversion. While definitive treatment remains controversial, initial management typically involves antibiotics, often third generation cephalosporins with adequate central nervous system penetrance such as ceftriaxone, for 6–8 weeks. Patients with large lesions, poor clinical status, or an unknown diagnosis may be considered for surgical drainage and subsequent culture speciation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bogdan M, Zujic Atalic V, Hecimovic I, Vukovic D. Brain abscess due to Aggregatibacter aphrophilus and Bacteroides uniformis. Acta Med Acad. 2015. 44: 181-5
2. Fulgham JR, Wijdicks EF, Wright AJ. Cure of a solitary brainstem abscess with antibiotic therapy: Case report. Neurology. 1996. 46: 1451-4
3. Hamamoto Filho PT, Zanini MA. Brainstem abscess of undetermined origin: Microsurgical drainage and brief antibiotic therapy. Sao Paulo Med J. 2014. 132: 121-4
4. Jung GW, Parkins MD, Church D. Pyogenic ventriculitis complicating Aggregatibacter aphrophilus infective endocarditis: A case report and literature review. Can J Infect Dis Med Microbiol. 2009. 20: e107-9
5. Maraki S, Papadakis IS, Chronakis E, Panagopoulos D, Vakis A. Aggregatibacter aphrophilus brain abscess secondary to primary tooth extraction: Case report and literature review. J Microbiol Immunol Infect. 2016. 49: 119-22
6. Reddy JS, Mishra AM, Behari S, Husain M, Gupta V, Rastogi M. The role of diffusion-weighted imaging in the differential diagnosis of intracranial cystic mass lesions: A report of 147 lesions. Surg Neurol. 2006. 66: 246-