- Department of Neurosurgery, Kokilaben Dhirubhai Ambani Research and Medical Center, Mumbai, Maharashtra, India.
Correspondence Address:
Anirudha Bharat Doshi, Department of Neurosurgery, Kokilaben Dhirubhai Ambani Research and Medical Center, Mumbai, Maharashtra, India.
DOI:10.25259/SNI_586_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Anirudha Bharat Doshi, Hrishikesh Sarkar, Yashwant Shelke, Amit Pothare, Amey Kulkarni. Solving a complex, rare, and challenging scenario in a normal pressure hydrocephalus with recurrent shunt dysfunction and multiple revisions – The opposing role of evolving low-pressure hydrocephalus and idiopathic raised intra-abdominal pressure. Surg Neurol Int 25-Nov-2022;13:546
How to cite this URL: Anirudha Bharat Doshi, Hrishikesh Sarkar, Yashwant Shelke, Amit Pothare, Amey Kulkarni. Solving a complex, rare, and challenging scenario in a normal pressure hydrocephalus with recurrent shunt dysfunction and multiple revisions – The opposing role of evolving low-pressure hydrocephalus and idiopathic raised intra-abdominal pressure. Surg Neurol Int 25-Nov-2022;13:546. Available from: https://surgicalneurologyint.com/surgicalint-articles/12028/
Abstract
Background: Maintenance of pressure gradient within the intracranial chamber, shunt hardware, and the abdominal cavity plays a significant role in the optimal functioning of the ventriculo peritoneal shunt. We report a rare and a complex scenario in a patient with normal pressure hydrocephalus (NPH) who had recurrent and refractory ventricular peritoneal shunt dysfunction. Following a meticulous analysis, this was attributed to a very rare, and, first to be documented in the literature, a combination of an evolved very low pressure hydrocephalus (VLPH) system and asymptomatic raised intra-abdominal pressure (IAP).
Case Description: A 72-year-old male presented with NPH syndrome, associated with recurrent shunt dysfunction. A thorough systematic evaluation, which included intracranial pressure monitoring and IAP monitoring, revealed the presence of VLPH and a concomitant elevated IAP that was asymptomatic. This unique situation required changes in surgical strategy, which included correction of VLPH state, insertion of the anti-siphon device, and the placement of the distal end of the shunt into the pleural cavity. This led to solving the “mystery” of recurrent shunt dysfunction in this complex scenario.
Conclusion: It is imperative to perform the pressure analysis of the intracranial chamber, shunt hardware, and even the abdominal cavity, especially, in every case of refractory shunt revisions. Possibilities of a rare cause such as VLPH or an asymptomatic raised IAP acting alone or in combination must be considered. Only then, the final cerebrospinal fluid diversion strategy should be decided.
Keywords: Hydrocephalus, Intra abdominal pressure, Low pressure hydrocephalus, Shunt dysfunction, Ventriculo peritoneal shunt
INTRODUCTION
Hydrocephalus is an active distention of the ventricular system of the brain resulting from an inadequate passage of cerebrospinal fluid (CSF) from its point of production within the cerebral ventricles, to its point of absorption into the systemic circulation.[
Maintenance of pressure gradient within the intracranial chamber, shunt hardware, and abdominal cavity plays a significant role in optimal functioning of the ventricular peritoneal shunt. While the most frequent cause of shunt dysfunction is either related to altered pressure dynamics in the intracranial cavity or hardware dysfunction, minimal attention has been accorded to raise intra-abdominal pressure (IAP) as a causative factor. We report a rare and complex and unusual scenario in a patient presumed to have normal pressure hydrocephalus (NPH) with numerous failed shunt revisions, the cause of which was finally attributed to an extremely rare combination of an asymptomatic increased IAP and, a newly evolved very low pressure hydrocephalus (VLPH).
CASE HISTORY
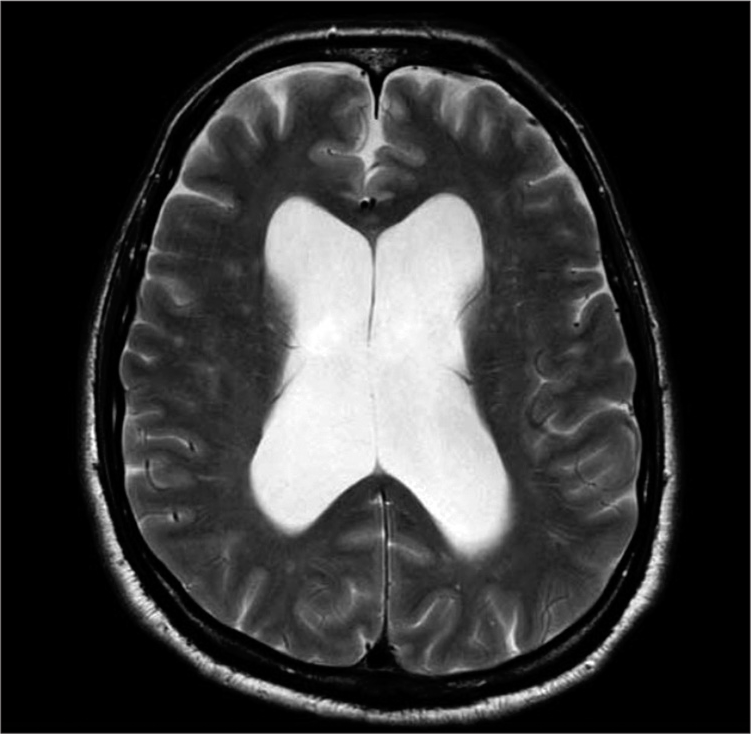
A 72-year-old male presented with memory disturbances, imbalance, and urinary urgency for the past 4 months, indicating classical features of NPH. This was further confirmed by radiographic imaging [
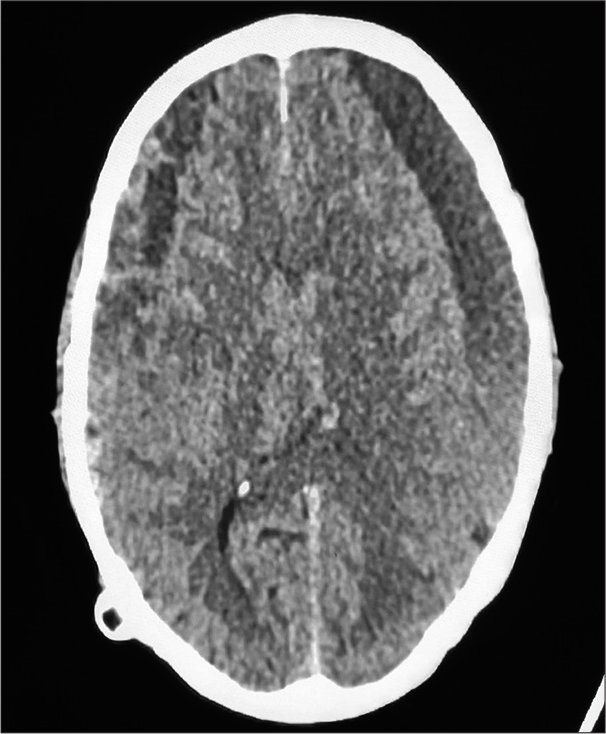
A month later, he presented again with altered sensorium and ventriculomegaly [
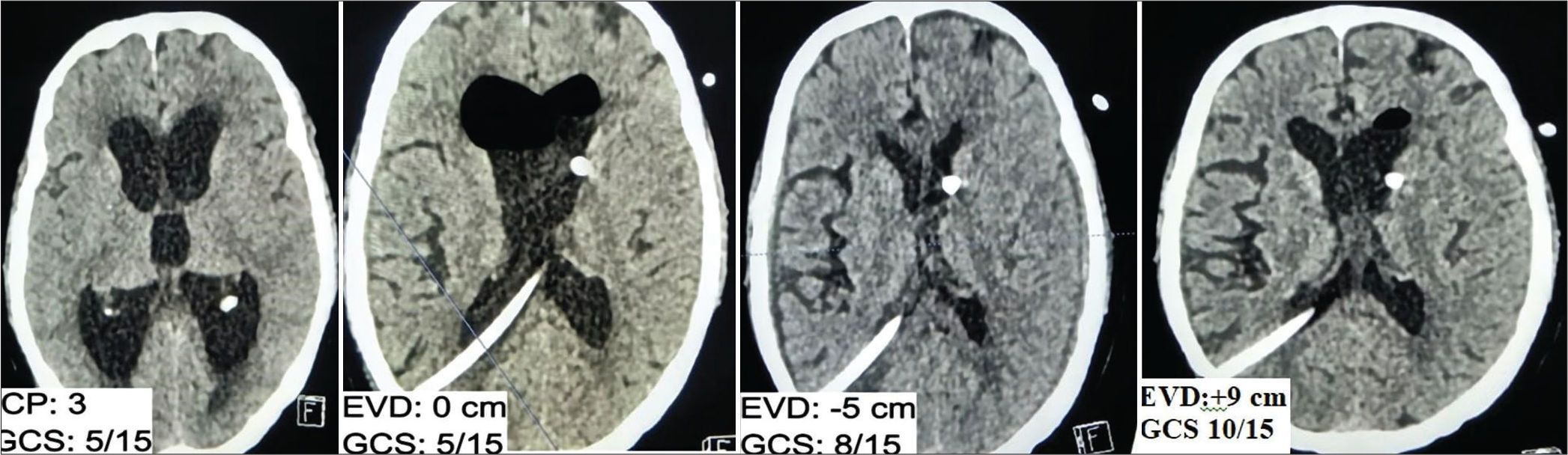
Considering a difficult case of hydrocephalus and recurrent shunt failure, it was imperative to assess every single compartmental pressure that directs the flow of CSF. To get a “true” value of the intracranial pressure (ICP) recordings and not allowing any effect of the existing valve settings, an external ventricular drainage (EVD) was placed in the contralateral left frontal horn, while the exteriorized tube was kept clamped. ICP measured through EVD was mere 3 mmHg, whereas the IAP was 25 cm of H2O (18 mm Hg). The evaluation was performed for the cause of high IAP and was inconclusive. This high IAP (18 mmHg) with a VLPH (<3 mmHg) contributed to loss of differential pressure resulting in recurrent shunt dysfunction.
This extraordinary situation was circumvented initially by correcting the VLPH by the sub-zero draining method of Pang et al.[
Significant improvement in the condition of the patient was noted within 1 week of surgery, patient was later discharged ambulating, with minimal assistance. Patient has been following up as outpatient for the past 2 years without any neurological deficits or shunt dysfunction.
DISCUSSION
We describe a rare and extraordinary case of a patient with LPHS and intra-abdominal hypertension. The combination of these two opposing pressure gradients resulted in recurrent shunt dysfunction.
Why does CSF flow within the shunt tube?
CSF flows from high pressure cavity to the low pressure cavity. The drainage of CSF in Ventriculoperitoneal (VP) shunt is regulated by ICP, hydrostatic pressure (HSP), and IAP. The tally of ICP with HSP needs to be more than IAP for effective drainage of CSF. This can be mathematically summed up as:
Draining pressure (+) = ICP (+) + HCP (+) (p fluid density × g gravity × h height) – IAP (+) (Eq. 1)[
When the draining pressure is positive, then there is forward flow of CSF within the shunt tube.
Situational analysis in our case
Role of ICP – State of low pressure/negative pressure hydrocephalus (NePH)
Pang et al.[
To promote adequate drainage of CSF, it is essential to have the drainage system pressure to be lower than the ICP. Hence, the treatment of NePH is to gradually increase the ICP by initiating the CSF drainage at pressure lower than ICP. This principle was followed in our case and the ICP was gradually increased to subnormal pressure.
Role of hydrostatic pressure
The hydrostatic pressure is directly dependent on the fluid density, gravity, and the height of the fluid column. Due to the position of the patient, the height of the fluid column can vary and therefore hydrostatic pressure can be variable in sitting and supine position.[
Role of IAP
Normal range of IAP is 0–7 mm Hg.[
IAP in standing and sitting pressure ranges from 16 to 20 mmHg.[
What had happened in this case?
In our case, IAP could have been normal/high normal at the time of the index shunt placement and also at the time of over drainage. Combination of “normal” ICP and the HCP was able to move the CSF into the abdominal cavity. However, progressively, the patient became non-ambulatory and obtunded probably due to evolution of VLPH. At this moment, two opposing pressure gradients were acting simultaneously – a very low ICP and a high IAP with resultant malfunction as illustrated in Equation 2.
Draining pressure (−) = ICP (−) + HCP (+) (p fluid density × g gravity × h height) – IAP (−) (Eq. 2)
Strategy for shunt placement in this scenario
To change the direction of flow, ICP needed to be more positive, and a distal reservoir more negative. Therefore, the VLPH state was corrected as described above and made more positive, while the pleural cavity was chosen as the reservoir as it has a negative pressure[
Were there options?
Endoscopic third ventriculostomy? (ETV)
ETV is a treatment for low pressure hydrocephalus (LPH) especially in patients who have undergone 3rd–4th ventricular tumor excision surgeries and intraventricular bleed. Due to the uncertainty over the results of ETV and concerns with the over drainage, we adopted a more “measurable” and a definitive procedure based on the strong hypotheses that were created.
Lumboperitoneal (LP) shunt?
LP shunt is a treatment for VLPH state. Considering a situation of LPH with high IAP approaching into peritoneum has high chances of failure. We had shunt in situ that was not infected, without blockage, and otherwise “working well.” Having worked on building up strong hypotheses, and limited data on the efficacy of LP shunt, we were less inclined to adopt LP shunt.
CONCLUSION
VP shunt for hydrocephalus is known for multiple complications. LPH itself is arduous to diagnose. In addition, the presence of “occult” elevated IAP can be a nightmare for the surgeon and the patient. Measuring IAP becomes essential in complex failed cases of shunt surgery to prevent complications. This case highlights the importance to understand the physiology behind the working of a VP shunt and the mechanisms behind its dysfunction especially if there is no mechanical obstruction. Pre-operative monitoring of ICP and IAP becomes essential to avoid repeated surgical procedures and reduce hospital stay and financial strain especially in patients with history of multiple shunt revision procedures, abdominal surgeries, and obesity.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Cobb WS, Burns JM, Kercher KW, Matthews BD, James Norton H, Todd Heniford B. Normal intraabdominal pressure in healthy adults. J Surg Res. 2005. 129: 231-5
2. Chatterjee S, Harischandra L. Cerebrospinal fluid shunts-how they work: The basics. Neurol India. 2018. 66: 24-35
3. De Keulenaer BL, De Waele JJ, Powell B, Malbrain ML. What is normal intra-abdominal pressure on how is it affected by positioning, body mass and positive end-expiratory pressure?. Intensive Care Med. 2009. 35: 969-76
4. Hakim S, Venegas JG, Burton JD. The physics of the cranial cavity, hydrocephalus and normal pressure hydrocephalus: Mechanical interpretation and mathematical model. Surg Neurol. 1976. 5: 187-210
5. Mirzayan MJ, Koenig K, Bastuerk M, Krauss JK. Coma due to meteorism and increased intra-abdominal pressure subsequent to ventriculoperitoneal shunt dysfunction. Lancet. 2006. 368: 2032
6. Pang D, Altschuler E. Low-pressure hydrocephalic state and viscoelastic alterations in the brain. Neurosurgery. 1994. 35: 643-55
7. Rekate HL. A contemporary definition and classification of hydrocephalus. Semin Pediatr Neurol. 2009. 16: 9-15
8. Sahuquillo J, Arikan F, Poca MA. Intra-abdominal pressure: The neglected variable in selecting the ventriculoperitoneal shunt for treating hydrocephalus. Neurosurgery. 2008. 62: 143-50
9. Sugerman H, Windsor A, Bessos M, Wolfe L. Intra-abdominal pressure, sagittal abdominal diameter and obesity comorbidity. J Intern Med. 1997. 241: 71-9