- Mexico City Spine Clinic, “Dr. Manuel Dufoo Olvera”, Mexico City, Mexico.
- Department of Neuroanestesiology, Specialties Hospital, La Raza National Medical Center, Mexican Social Security Institute, Mexico City, Mexico.
- Department of Neurosurgery, Specialties Hospital, La Raza National Medical Center, Mexican Social Security Institute, Mexico City, Mexico.
Correspondence Address:
Oscar Josue Montes-Aguilar, Mexico City Spine Clinic “Dr. Manuel Dufoo Olvera”, Mexico City, Mexico.
DOI:10.25259/SNI_564_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Oscar Josue Montes-Aguilar1, Karmen Karina Alaniz-Sida2, Manuel Dufoo-Olvera1, Guillermo Ivan Ladewig-Bernaldez1, Edith Oropeza-Oropeza1, Gerson Gómez-Flores1, Jeasson Javier Pérez-Rios1, Alejandro Miguel-Zambrano1, Maurilio Vicente Ochoa-González3, Héctor Alonso Tirado-Ornelas3. Spinal canal invasion as a predictor of neurological deficit in traumatic vertebral burst fractures. 23-Sep-2022;13:428
How to cite this URL: Oscar Josue Montes-Aguilar1, Karmen Karina Alaniz-Sida2, Manuel Dufoo-Olvera1, Guillermo Ivan Ladewig-Bernaldez1, Edith Oropeza-Oropeza1, Gerson Gómez-Flores1, Jeasson Javier Pérez-Rios1, Alejandro Miguel-Zambrano1, Maurilio Vicente Ochoa-González3, Héctor Alonso Tirado-Ornelas3. Spinal canal invasion as a predictor of neurological deficit in traumatic vertebral burst fractures. 23-Sep-2022;13:428. Available from: https://surgicalneurologyint.com/surgicalint-articles/11890/
Abstract
Background: This study correlated the extent of spinal canal compression from retropulsed traumatic burst cervical, thoracic, and lumbar spine fractures with the severity of neurological dysfunction.
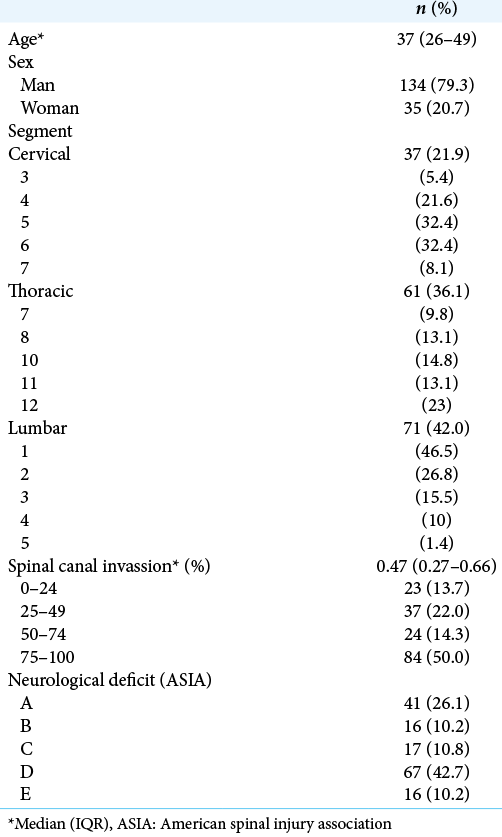
Methods: One hundred and sixty-nine patients with cervical, thoracic, or lumbar sub-axial traumatic burst fractures were seen in an emergency department from 2019 to 2021; 79.3% were men, averaging 37 years of age. The lumbar spine was most frequently involved (42%), followed by the thoracic (36.1%) and cervical (21.9%) levels. The extent of spinal canal compression was quantitated utilizing Hashimoto’s method, and correlated with patients’ extent of neurological injury based on their American Spinal Injury Association scores.
Results: There was a positive correlation between the extent of cervical and thoracic spinal cord compression due to retro pulsed burst fragments and the severity of the patients’ neurological deficits, but this was not true for the lumbar spine.
Conclusion: The extent of spinal cord compression from retropulsed cervical and thoracic traumatic burst fractures was readily correlated with the severity of patients’ neurological dysfunction. However, there was no such correlation between the extent of cauda equina compression from retropulsed lumbar burst fractures and the severity of their cauda equina syndromes.
Keywords: Burst fractures, Canal invasion, Spine trauma, Spine, Subaxial fractures
INTRODUCTION
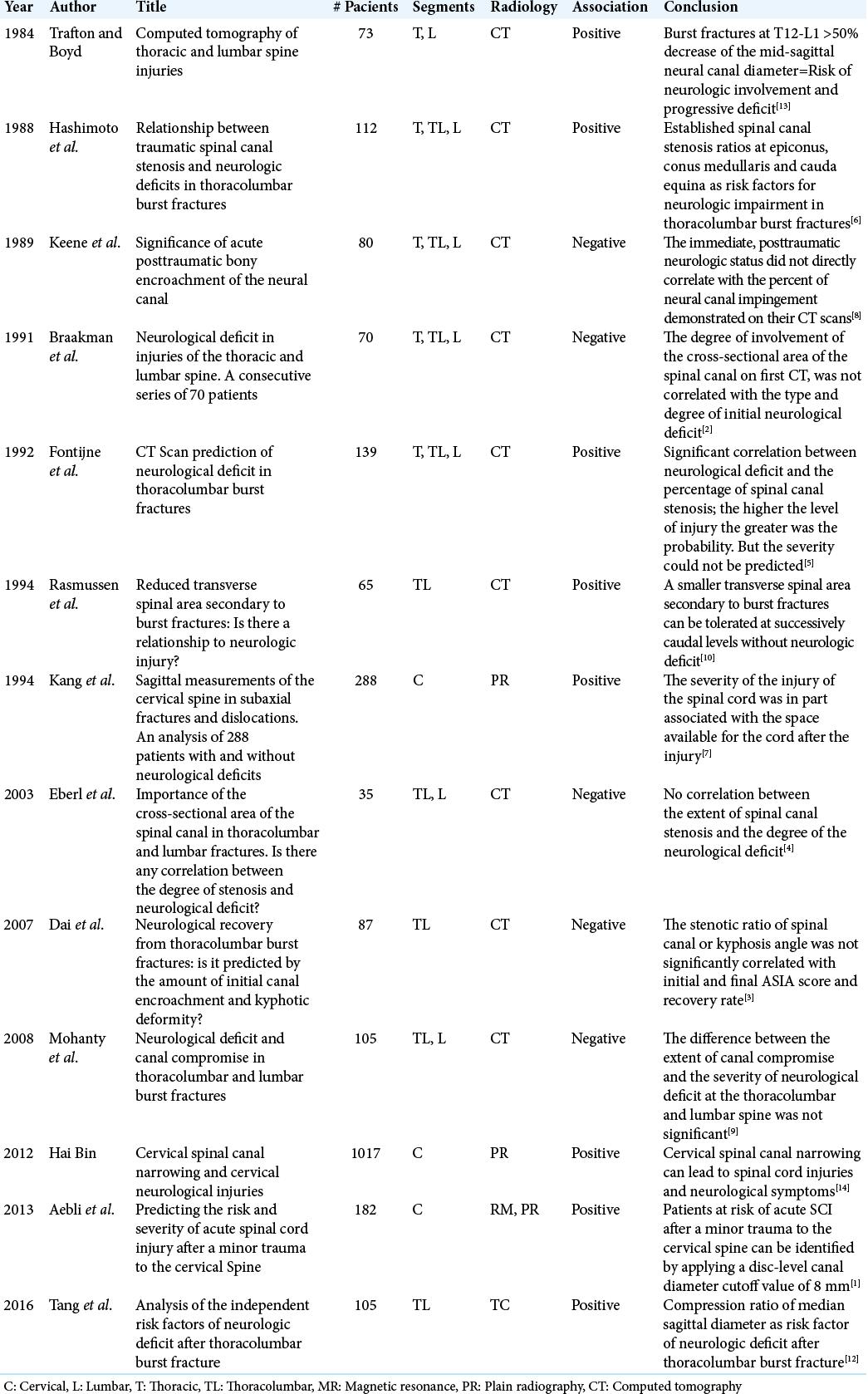
Different combination of plain X-rays, magnetic resonance, and computed tomography (CT) studies are used to assess the extent of spinal canal compromise and neurological deficits due to retropulsed cervical, thoracic, and lumbar burst fractures.[
MATERIALS AND METHODS
Clinical series
CT-Documented inclusion criteria
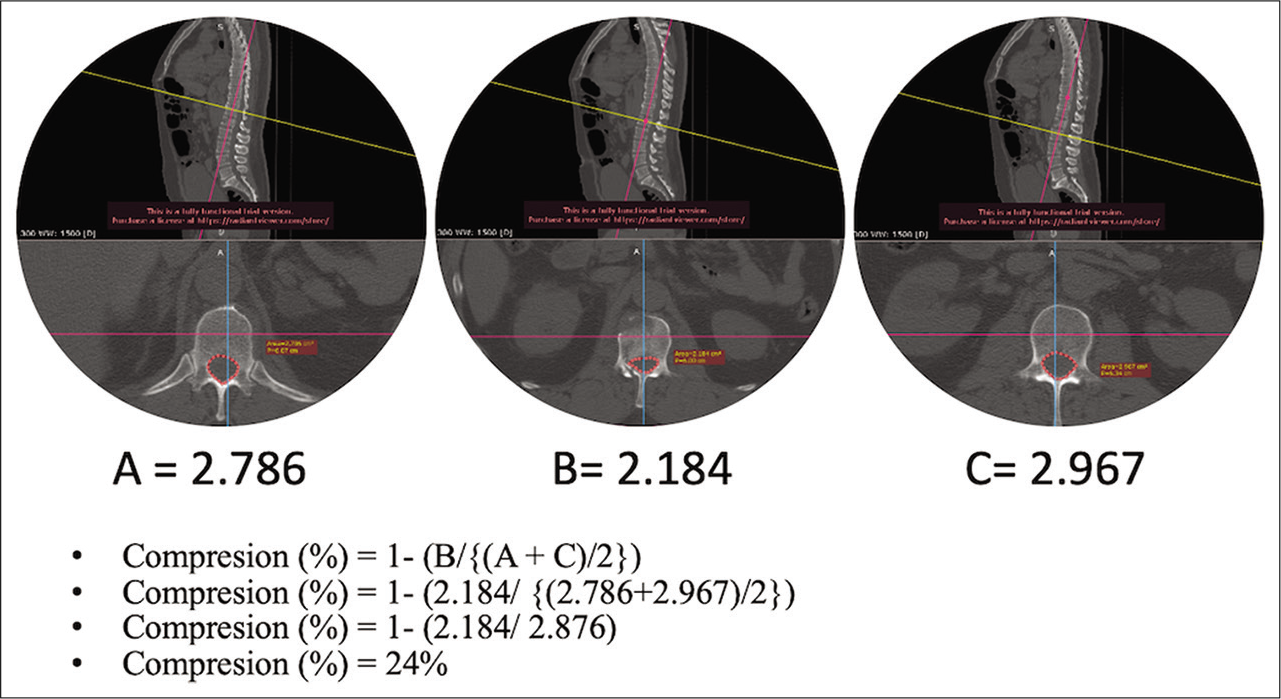
To be included in this study, patients’ CT studies had to demonstrate traumatic burst spine fractures (2019–2021) involving the sub-axial cervical (C3–7) spine, the thoracic spine, and/or the lumbar spine. The frequency of such burst fractures in descending order involved the lumbar (42%), followed by the thoracic (36.1%) and cervical (21.9%) regions. The extent of spinal canal compression (i.e., 50% had stenosis of greater than 47%) was measured on CT studies using Hashimoto’s method (i.e., transversa area of the spinal canal at the fracture level divided by mean transverse area of the spinal canal from the adjacent superior and inferior vertebrae[
Clinical review
We reviewed the complete electronic medical records and obtained written informed consent from 169 patients 79.3% of whom were male, averaging 37 years of age. All had vertebral burst fractures with most demonstrating incomplete spinal cord injuries [
Neurological deficits based on American spinal injury association (ASIA) scores
Neurological deficits were assessed using the ASIA score.[
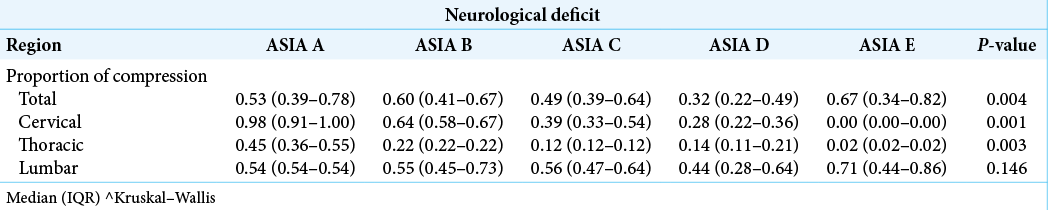
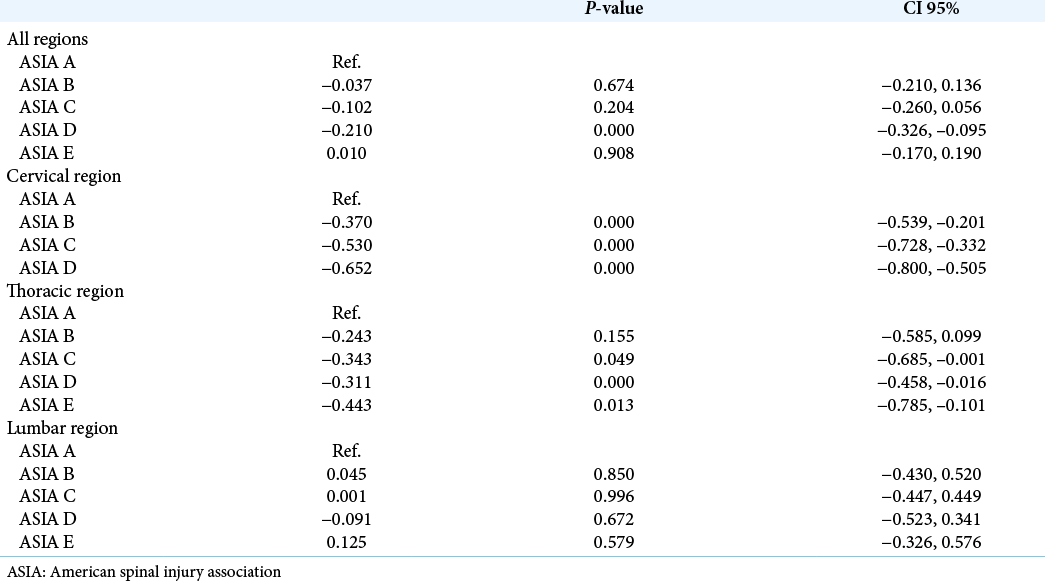
The authors performed a linear regression stratification of the different spinal level burst fractures to determine the correlate of the CT-documented extent of canal compromise with their resultant neurological deficits (i.e., using ASIA score and the Mann–Whitney test) [
RESULTS
Correlation of cervical and thoracic spinal canal compression from burst fractures with neurological deficits
The authors observed a positive correlation between the extent of cervical and thoracic spinal canal compression and the severity of patients’ neurological deficits. In the cervical spine, the median compression was 0.98 for ASIA A, which proportionally decreased for less severe spinal injuries [
DISCUSSION
We found the extent of cervical and thoracic canal compromise attributed to retropulsed vertebral burst fractures/fragments positively correlated with the severity of resultant neurological deficits, similar to the findings of Fontijne et al., who found a significant correlation between neurological deficit and the percentage of spinal canal stenosis, but the severity could not be predicted.[
CONCLUSION
Following sub-axial cervical and thoracic spine traumatic burst fractures, but not lumbar fractures, the extent of CT-documented spinal canal compression positively correlated with the severity of patients’ neurological deficits.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aebli N, Rüegg T, Wicki A, Petrou N, Krebs J. Predicting the risk and severity of acute spinal cord injury after a minor trauma to the cervical spine. Spine J. 2013. 13: 597-604
2. Braakman R, Fontijne W, Zeegers R, Steenbeek J, Tanghe H. Neurological deficit in injuries of the thoracic and lumbar spine. Acta Neurochir. 1991. 111: 11-7
3. Dai L, Wang X, Jiang L. Neurologic recovery from thoracolumbar burst fractures: Is it predicted by the amount of initial canal encroachment and kyphotic deformity?. Surg Neurol. 2007. 67: 232-7
4. Eberl R, Kaminski A, Müller EJ, Muhr G. Importance of the cross-sectional area of the spinal canal in thoracolumbar and lumbar fractures. Is there any correlation between the degree of stenosis and neurological deficit? Orthopade 2003. ;. 32: 859-64
5. Fontijne W, de Klerk L, Braakman R, Stijnen T, Tanghe H, Steenbeek R. CT scan prediction of neurological deficit in thoracolumbar burst fractures. J Bone Joint Surg Br. 1992. 74: 683-5
6. Hashimoto T, Kaneda K, Abumi K. Relationship between traumatic spinal canal stenosis and neurologic deficits in thoracolumbar burst fractures. Spine. 1988. 13: 1268-72
7. Kang J, Figgie M, Bohlman H. Sagittal measurements of the cervical spine in subaxial fractures and dislocations. An analysis of two hundred and eighty-eight patients with and without neurological deficits. J Bone Joint Surg. 1994. 76: 1617-28
8. Keene J, Fischer S, Vanderby R, Drummond D, Turski P. Significance of acute posttraumatic bony encroachment of the neural canal. Spine. 1989. 14: 799-802
9. Mohanty S, Bhat N, Abraham R, Keerthi C. Neurological deficit and canal compromise in thoracolumbar and lumbar burst fractures. J Orthop Surg (Hong Kong). 2008. 16: 20-3
10. Rasmussen P, Rabin M, Mann D, Perl J, Lorenz M, Vrbos L. Reduced transverse spinal area secondary to burst fractures: Is there a relationship to neurologic injury?. J Neurotrauma. 1994. 11: 711-20
11. Roberts TT, Leonard GR, Cepela DJ. Classifications in brief: American spinal injury association (ASIA) impairment scale. Clin Orthop Relat Res. 2017. 475: 1499-504
12. Tang P, Long A, Shi T, Zhang L, Zhang L. Analysis of the independent risk factors of neurologic deficit after thoracolumbar burst fracture. J Orthop Surg Res. 2016. 11: 128
13. Trafton P, Boyd C. Computed tomography of thoracic and lumbar spine injuries. J Trauma. 1984. 24: 506-15
14. Zhang L, Chen HB, Wang Y, Zhang LY, Liu JC, Wang ZG. Cervical spinal canal narrowing and cervical neurological injuries. Chin J Traumatol. 2012. 15: 36-41