- Department of Neurosurgery, Highly Specialized Hospital and of National Importance “Garibaldi,” Catania,
- Experimental Biomedicine and Clinical Neurosciences, School of Medicine, Postgraduate Residency Program in Neurological Surgery, Neurosurgical Clinic, AOUP “Paolo Giaccone,” Palermo, Italy,
- Department of Neurosurgery, UC Health, Cincinnati, Ohio, United States,
- Department of Neurosurgery, Cannizzaro Hospital, Trauma Center, Gamma Knife Center, Catania, Italy.
Correspondence Address:
Gianluca Scalia, Department of Neurosurgery, Highly Specialized Hospital and of National Importance “Garibaldi,” Catania, Sicily, Italy.
DOI:10.25259/SNI_260_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Gianluca Scalia1, Salvatore Marrone2, Federica Paolini2, Paolo Palmisciano3, Giancarlo Ponzo1, Massimiliano Giuffrida1, Massimo Furnari1, Domenico Gerardo Iacopino2, Giovanni Federico Nicoletti1, Giuseppe Emmanuele Umana4. Spinal epidural abscess due to acute pyelonephritis. 22-Apr-2022;13:159
How to cite this URL: Gianluca Scalia1, Salvatore Marrone2, Federica Paolini2, Paolo Palmisciano3, Giancarlo Ponzo1, Massimiliano Giuffrida1, Massimo Furnari1, Domenico Gerardo Iacopino2, Giovanni Federico Nicoletti1, Giuseppe Emmanuele Umana4. Spinal epidural abscess due to acute pyelonephritis. 22-Apr-2022;13:159. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11556
Abstract
Background: Spinal epidural abscesses are rare and are misdiagnosed in up to 75% of cases. Fever, back pain, and neurological deficits are part of the classical triad. Here, the authors report a patient with a L2–L5 spinal epidural abscess with the left paravertebral extension attributed to acute pyelonephritis.
Case Description: A 54-year-old female presented with persistent low back pain and lower extremity weakness accompanied by paresthesias. Previously, she had been hospitalized with the left acute pyelonephritis. The lumbosacral MRI documented a T12/L5 anterior epidural abscess with ring enhancement on the contrast study; the maximum diameter of the abscess at the L2–L3 level contributed to severe cauda equina compression. She underwent a L2/L4 decompressive laminectomy with drainage of the intraspinal/extradural and paravertebral components. Intraoperative microbiological sampling grew Staphylococcus aureus for which she then received targeted antibiotic therapy. Fifteen days later, she was walking adequately when discharged.
Conclusion: Thoracolumbar epidural abscesses are rare. They must be considered among the differential diagnoses when patients present with acute back pain, fever, and new neurological deficits following prior treatment for acute pyelonephritis.
Keywords: Abscess, Batson’s plexus, Epidural, Pyelonephritis, Pyogenic bacteria
INTRODUCTION
Spinal epidural abscesses (SEAs) are rare and are misdiagnosed in up to 75% of cases.[
CASE REPORT
Clinical history
A 54-year-old female was previously hospitalized with acute pyelonephritis for 3 weeks. She was now admitted after about 1 week with persistent lumbar pain (visual analog scale score of 8 / 10) and the onset of a spastic paraparesis (4 / 5 BMRC) without sphincter dysfunction. The lumbar CT scan showed left paravertebral and epidural collections extending from T12 to L5. The lumbosacral MRI documented a T12/L5 anterior epidural hypointense lesion with ring enhancement; the maximum AP diameter was 1.2 cm at the L2–L3 where it caused severe cauda equina compression [
Figure 1:
Preoperative sagittal T1-WI with contrast enhancement (a), sagittal T2-WI (b), and axial T2-WI (c) MRI showed a T12/L5 anterior epidural hypointensity with ring enhancement on T1-WI sequences after gadolinium administration, with a maximum diameter of 1.2 cm at L2–L3 causing severe cauda equina compression.
Surgery and postoperative course
The patient underwent a L2/L4 decompressive laminectomy with drainage of the intraspinal/extradural and paravertebral SEA; at surgery, a ventral extradural frankly purulent collection identified. After drainage, local vancomycin powder was applied. Postoperatively, within 15 days, she was pain free, had no residual neurological deficits, and was discharged home. One week postoperative, lumbar MRI documented adequate canal decompression with complete abscess drainage [
Pathogen
Staphylococcus aureus was the organism isolated from surgery. The patient, therefore, underwent targeted antibiotic therapy with daptomycin, meropenem, and teicoplanin until serum inflammatory values returned to normal.
DISCUSSION
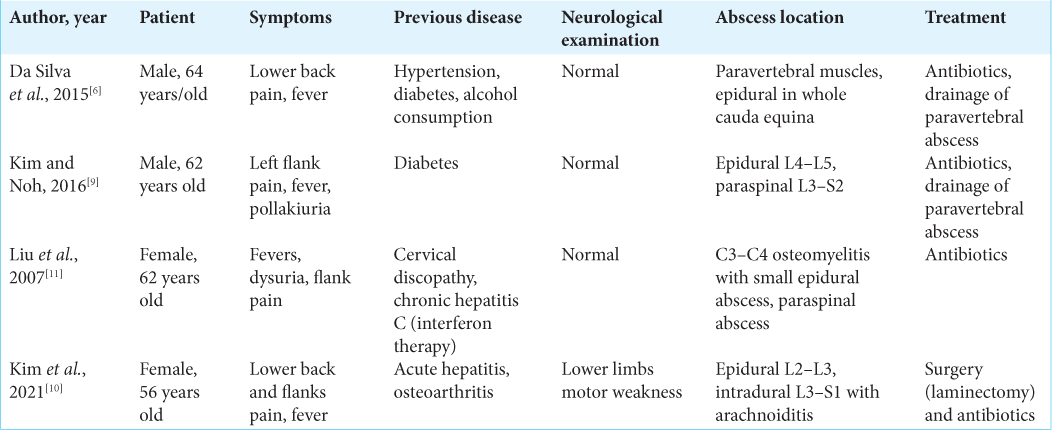
There are a few select reports attributing SEA to pyelonephritis.[
CONCLUSION
SEA may occur due to hematogenous extension of bacteria attributed to prior pyelonephritis. Here, a 54-year-old female, following pyelonephritis 4 weeks ago, presented with low back pain and a paraparesis attribute to a CT/MR documented T12/L5 anterior SEA successfully treated with an L2–L4 laminectomy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ameer MA, Knorr TL, Mesfin FB.editors. Spinal epidural abscess. StatPearls. Treasure Island, FL: StatPearls Publishing; 2021. p.
2. Bond A, Manian FA. Spinal epidural abscess: A review with special emphasis on earlier diagnosis. Biomed Res Int. 2016. 2016: 1614328
3. Carpenter K, Decater T, Iwanaga J, Maulucci CM, Bui CJ, Dumont AS. Revisiting the vertebral venous plexus-a comprehensive review of the literature. World Neurosurg. 2021. 145: 381-95
4. Chao D, Nanda A. Spinal epidural abscess: A diagnostic challenge. Am Fam Physician. 2002. 65: 1341-6
5. Curry WT, Hoh BL, Amin-Hanjani S, Eskandar EN. Spinal epidural abscess: Clinical presentation, management, and outcome. Surg Neurol. 2005. 63: 364-71
6. da Silva CN, Safadi AP, de Azevedo Silva AB, Lanzieri PG. Epidural abscess in a diabetic patient with complicated pyelonephritis: Case report and literature review. Med Case Stud. 2016. 7: 1-4
7. Davis DP, Salazar A, Chan TC, Vilke GM. Prospective evaluation of a clinical decision guideline to diagnose spinal epidural abscess in patients who present to the emergency department with spine pain. J Neurosurg Spine. 2011. 14: 765-70
8. Heller MT, Haarer KA, Thomas E, Thaete F. Acute conditions affecting the perinephric space: Imaging anatomy, pathways of disease spread, and differential diagnosis. Emerg Radiol. 2012. 19: 245-54
9. Kim DH, Noh SH. Spinal epidural and subarachnoid abscess due to acute pyelonephritis in a 56-year-old woman: A case report and literature review. Nerve. 2021. 7: 114-6
10. Kim MJ, Koo HM, Lee WJ, Choi JH, Choi MN, Park SY. Development of epidural and paraspinal abscesses after insufficient evaluation and treatment of acute pyelonephritis caused by Staphylococcus aureus. Korean J Fam Med. 2016. 37: 299-302
11. Liu JH, Lin PW, Liu YL, Liao PY. Cervical spinal osteomyelitis with epidural abscess: A rare complication after interferon therapy following acute pyelonephritis. Nephrology (Carlton). 2007. 12: 418-9
12. Ogoshi T, Yoshimiya M, Ichibakase H, Kimura T, Kameoka M, Yoshioka H. Spinal epidural abscess in patients with sepsis who experienced significant improvements after complete paralysis: Two case reports. Open J Emerg Med. 2020. 8: 84014
13. Sendi P, Bregenzer T, Zimmerli W. Spinal epidural abscess in clinical practice. QJM. 2008. 101: 1-12