- Neurosurgical Department, Asclepeion General Hospital of Athens, Athens, Greece
Correspondence Address:
Rovlias Aristedis
Neurosurgical Department, Asclepeion General Hospital of Athens, Athens, Greece
DOI:10.4103/sni.sni_197_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Rovlias Aristedis, Bougioulis Dimitrios. Spinal epidural hematoma mimicking subarachnoid hemorrhage: A case study. 10-Aug-2017;8:182
How to cite this URL: Rovlias Aristedis, Bougioulis Dimitrios. Spinal epidural hematoma mimicking subarachnoid hemorrhage: A case study. 10-Aug-2017;8:182. Available from: http://surgicalneurologyint.com/surgicalint-articles/spinal-epidural-hematoma-mimicking-subarachnoid-hemorrhage-a-case-study/
Abstract
Background:Spontaneous spinal epidural hematoma (SSEH) is a rare spinal cord disorder requiring urgent diagnosis and prompt treatment to prevent irreversible neurological damage. Subarachnoid hemorrhage (SAH), usually presenting with headache and neck stiffness, is also a worldwide neurosurgical emergency. In this case study, a patient on clopidogrel presented with an SSEH mimicking a spontaneous SAH.
Case Description:A 74-year-old female presented with severe headache and neck pain which ultimately attributed to a cervicothoracic SSEH resulting in cord compression. Notably, there was a long delay in establishing the diagnosis of SSEH as her symptoms mimicked a SAH. Although the patient ultimately underwent spinal surgery followed by intense rehabilitation, the diagnostic delay resulted in a poor neurological outcome.
Conclusions:Patients with spontaneous cervicothoracic epidural hematomas may occasionally present with symptoms of severe headache and neck pain/stiffness mimicking an SAH. Long diagnostic delays in establishing SSEH may result in irreversible cord damage.
Keywords: Clopidogrel, magnetic resonance imaging, spinal epidural hematoma, subarachnoid hemorrhage
INTRODUCTION
Subarachnoid hemorrhage (SAH), usually presenting with headache and neck pain/stiffness, is a worldwide neurosurgical emergency and must be differentiated from spontaneous spinal epidural hematoma (SSEH). SSEH, however, is a rare entity that must be differentiated from SAH early on in the clinical course to avoid irreversible spinal cord injury (0.1 patients per 100,000 individuals per year).[
Here, we present a 74-year-old female on clopidogrel whose headache/neck stiffness was originally misdiagnosed as a SAH. This led to delayed treatment of a cervicothoracic SSEH that resulted in an irreversible quadriparesis.
CASE REPORT
An obese 74-year-old female patient presented with a 3-day history of spontaneous sudden-onset headache and neck pain, accompanied by nausea, and a worsening occipital headache unresponsive to analgesics. Notably, she was taking clopidogrel 75 mg/d for coronary artery disease.
Neurological examination revealed marked nuchal rigidity, positive Kernig's sign, normal funduscopic examination (e.g., no papilledema), and no other focal neurological deficits. The initial clinical diagnosis was a spontaneous SAH.
Diagnostic studies
Routine laboratory and coagulation tests were within normal limits. Chest X-ray showed no abnormalities. Noncontrast cranial computed tomography (CT) was negative for intracranial hemorrhage. Lumbar puncture (LP) yielded clear cerebrospinal fluid (CSF); laboratory analysis of the CSF was normal. Doppler ultrasonography of the carotid revealed no significant stenosis or arterial dissection.
Progressive neurological deterioration
Thirty hours postadmission, the patient developed a rapidly progressive right hemiparesis accompanied by severe pain in the right shoulder. On examination, she exhibited marked hypesthesia with a severe flaccid paresis in both the right upper and right lower extremities (2/5 motor function). On the right side, deep tendon reflexes were decreased and there was no Babinski response. The second emergent brain CT scan was negative.
The patient was transferred to another institution 8 hours after the onset of hemiparesis at which point she was nearly quadriplegic (e.g., severe bilateral motor and sensory deficits below C5 level, labored respiration, and decreased chest expansion). Following cardiopulmonary resuscitation, magnetic resonance imaging (MRI) scan of the cervical spine demonstrated a large extradural mass, dorsally to the spinal cord extending from C3 through mid-T3. The mass had well-defined contours and contributed to multilevel posterior to anterior spinal cord compression. It was hyperintense on T1 [
Figure 1
An extradural more right -sided mass located dorsal to the spinal cord, extending from C3 through the mid-T3 vertebral level, resulting in marked spinal cord compression and edema/myelomalacia (high intrinsic cord signal). It was hyperintense on T1-weighted images (a), and heterogeneously hyperintense on T2-weighted images (b)
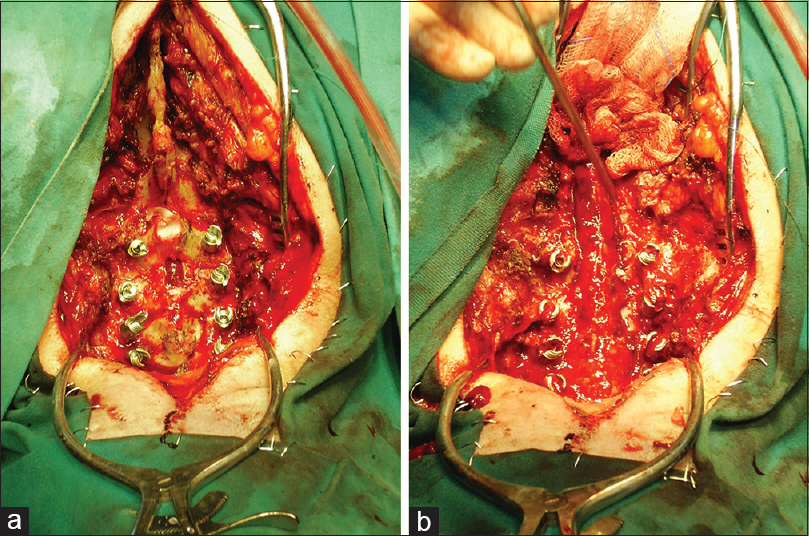
Operational procedure
The patient underwent a C3 to T1 laminectomy with lateral masses screws – posterior fixation to prevent instability; the C3–T3 epidural hematoma was completely evacuated. Below the ligamentum flavum, large hard, dark clots were found, but no discrete bleeding points or abnormal vessels could be identified [Figure
DISCUSSION
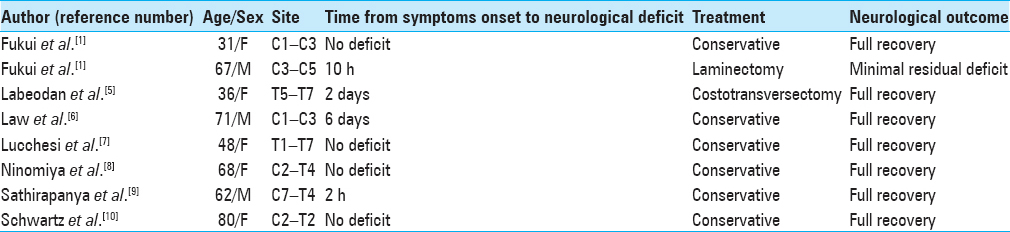
SSEH rarely causes spinal cord compression. It requires early diagnosis and prompt surgical treatment to prevent irreversible neurological damage or even death if the hematoma extends into the cephalad cervical region.[
Risk factors for SSEH include anticoagulant therapy, aspirin, vascular malformation, venous epidural plexus defects, hypertension, pregnancy, thrombolysis, physical exertion, chiropractic spinal manipulation, and hematological disorders.[
Delays in diagnosing SSEH increase the risks of permanent neurological deficits.[
SSEH requires emergent surgery to avoid rapid neurological deterioration. In our patient, the MR findings documented a subacute C3–T3 epidural hematoma, but the surgical delay of 36 hours resulted in an irreversible neurological injury/quadriparesis.
CONCLUSIONS
Patients with SSEH rarely present with severe headache and neck pain/stiffness. SSEH must rapidly be differentiated from a SAH, and MR studies of the neuraxis must be performed to localize and then surgically treat the SSEH to avoid permanent neurological injury.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Fukui MB, Swarnkar AS, Williams RL. Acute spontaneous spinal epidural hematomas. AJNR Am J Neuroradiol. 1999. 20: 1365-72
2. Groen RJ, van Alphen HA. Operative treatment of spontaneous spinal epidural hematomas: A study of the factors determining postoperative outcome. Neurosurgery. 1996. 39: 494-508
3. Holtas S, Heiling M, Lonntoft M. Spontaneous spinal epidural hematoma: Findings at MR imaging and clinical correlation. Radiology. 1996. 199: 409-13
4. Kreppel D, Antoniadis G, Seeling W. Spinal hematoma: A literature survey with meta-analysis of 613 patients. Neurosurg Rev. 2003. 26: 1-49
5. Labeodan OA. Spinal epidural haematoma mimicking spontaneous subarachnoid haemorrhage. Emerg Med J. 2005. 22: 606-7
6. Law EM, Smith PJ, Fitt G, Hennessy OF. Non-traumatic spinal extradural haematoma: Magnetic resonance findings. Australas Radiol. 1999. 43: 192-6
7. Lucchesi C, Ulivi M, Kiferle L, Baldacci F, Cafalli M, Puglioli M. Dorsal extramedullary hematoma: A rare case presenting as isolated thunderclap headache. Headache. 2015. 55: 1263-5
8. Ninomiya K, Iwatsuki K, Mrasawa A, Goto T, Naao K, Yoshimine T. Spontaneous spinal epidural hematoma: Magnetic resonance imaging for diagnosis and patient management in two cases. J Neurosci Behav Health. 2015. 7: 26-30
9. Sathirapanya P, Setthawatcharawanich S, Limapichat K, Phabphal K. Thunderclap headache as a presentation of spontaneous spinal epidural hematoma with spontaneous recovery. J Spinal Cord Med. 2013. 36: 707-10
10. Schwartz D, Arcot K, Grosberg BM, Robbins MS. Spontaneous cervical epidural hematoma associate with thunderclap headache. J Headache Pain. 2012. 13: 331-3