- Department of Neurosurgery, UNIFESP, Campinas, São Paulo, Brazil.
- Department of Medicine, Pontifical Catholic University of Campinas, Campinas, São Paulo, Brazil.
- Department of Neurosurgery, Pontifical Catholic University of Campinas, Campinas, São Paulo, Brazil.
- Department of Neurosurgery, UNICAMP, Cidade Universitária Zeferino Vaz - Barão Geraldo, Campinas, São Paulo, Brazil.
Correspondence Address:
Enrico Barletta
Department of Neurosurgery, UNICAMP, Cidade Universitária Zeferino Vaz - Barão Geraldo, Campinas, São Paulo, Brazil.
DOI:10.25259/SNI_728_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Eduardo Augusto Iunes1, Enrico Barletta2, Telmo Augusto Barba Belsuzarri3, Daniel Paz Araujo1, Fabio Sparapani1, Franz Onishi1, Sergio Cavalheiro1, Thiago Salati1, Vinicius De Meldau Benites1, Andrei Joaquim4. Spinal fractures in patients with ankylosing spondylitis: A case report and literature review. 04-Dec-2020;11:417
How to cite this URL: Eduardo Augusto Iunes1, Enrico Barletta2, Telmo Augusto Barba Belsuzarri3, Daniel Paz Araujo1, Fabio Sparapani1, Franz Onishi1, Sergio Cavalheiro1, Thiago Salati1, Vinicius De Meldau Benites1, Andrei Joaquim4. Spinal fractures in patients with ankylosing spondylitis: A case report and literature review. 04-Dec-2020;11:417. Available from: https://surgicalneurologyint.com/surgicalint-articles/10428/
Abstract
Background: Severe ankylosing spondylitis (AS) affects the entire spine, increasing the risk of vertebral fractures. There are several fusion procedures used (e.g., anterior, posterior, or combined 360° procedures) to stabilize these fractures.
Case Description: A 45-year-old male with a 33-year diagnosis of AS presented with a progressive quadriparesis of 6 months’ duration. Previously, he had surgery on both hips. The medical report documented degenerative spondylolisthesis at the C5-C6 level along with syndesmophytes a herniated disc and stenosis. Following a circumferential decompression/fusion without complications, the patient’s symptoms resolved.
Conclusion: For patients presenting with cervical fractures and AS, circumferential surgical decompression/ fusion may result in good outcomes.
Keywords: Ankylosing, Cervical and fracture, Spondylitis, Treatment
INTRODUCTION
Ankylosing spondylitis (AS) may present in patients under the age of 40 and is more prevalent in males (e.g., 80% under age 30).[
METHODS
We performed a literature review in PUBMED for AS. We included 13 AS articles involving a total of 221 patients.
Here, we also present a 45-year-old male who in 2019 presented with a C5-6 cervical fracture attributed to AS.
CASE REPORT
Case description
A 45-year-old male with a 33-year history of AS presented with a progressive quadriparesis (e.g., hypertonia, hyperreflexia positive bilateral Babinski and Hoffman signs, and neck disability index [NDI] of 10) of 6 months duration. The neurological findings included Grade IV quadriparesis, with hypertonia/hyperreflexia, and bilateral Hoffman’s and Babinski signs. Previously, he had surgery on both hips for AS deformities.
Radiologic findings
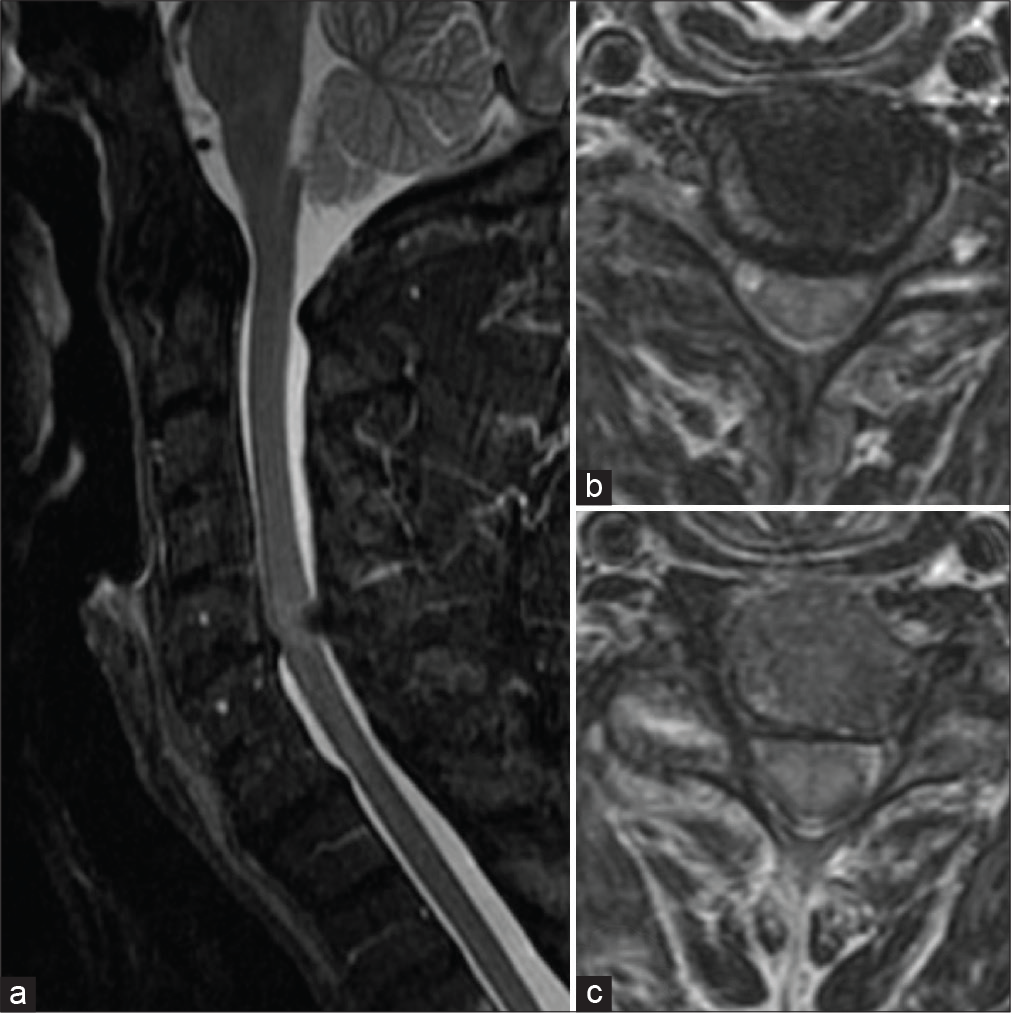
The preoperative medical report showed degenerative changes of the atlantoaxial joint, and at the C5-C6 level, degenerative spondylolisthesis, posterior syndesmophytes, thickening of ligamentum flavum, bilateral uncoarthroses, degenerative changes of the interapophyseal articulation, C5-C6 joint effusion, and disc dehydration/herniation and stenosis [
Surgical procedure
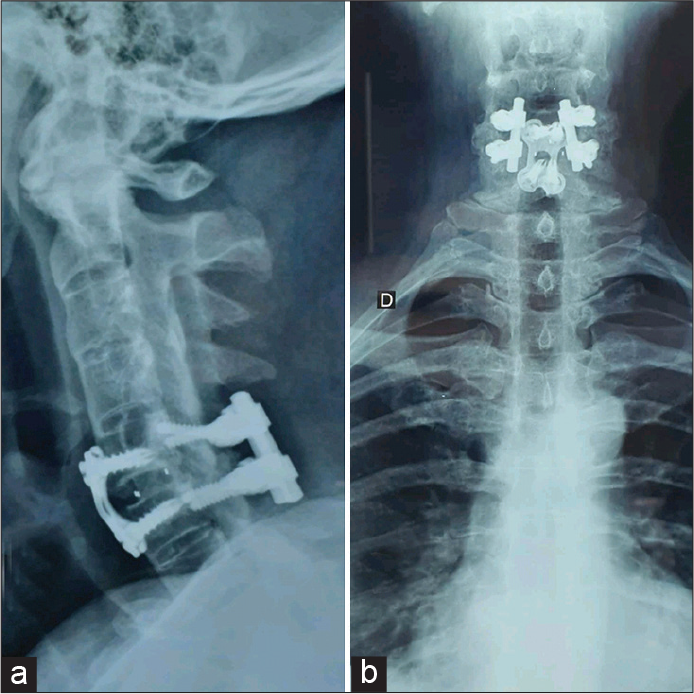
The patient underwent a circumferential surgical procedure. The first operation included an anterior C5-C6 discectomy and fusion that utilized a cage containing iliac autograft; a plate was also applied. The secondary surgery involved a posterior approach (e.g., C5-C6 laminectomy with bilateral lateral mass screw placement).
Postoperative course
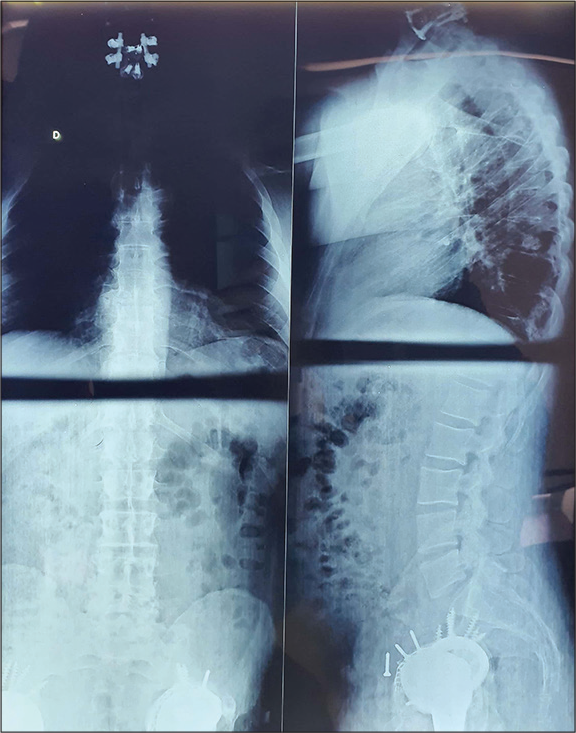
Up to 2 years postoperatively, the patient remained asymptomatic (e.g., NDI of 0) with final fluoroscopic images confirming adequate C5-C6 circumferential fusion [
DISCUSSION
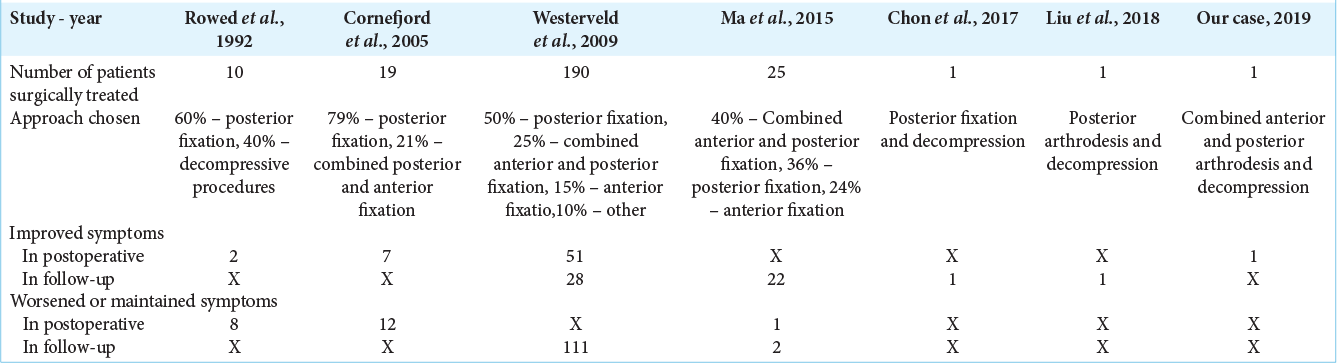
We presented our case of AS and a review of 13 studies of cervical AS. Those cases are presented in [
Ma et al.[
CONCLUSION
The operative technique utilized to treat patient with cervical AS fractures should depend on the type/location of these fractures with the clinical findings.[
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Allouch H, Shousha M, Böhm H. Surgical management of ankylosing spondylitis (Bechterew’s disease). Z Rheumatol. 2017. 76: 848-59
2. Chon H, Park JH. Cervical vertebral body fracture with ankylosing spondylitis treated with cervical pedicle screw: A fracture body overlapping reduction technique. J Clin Neurosci. 2017. 41: 150-3
3. Cornefjord M, Alemany M, Olerud C. Posterior fixation of subaxial cervical spine fractures in patients with ankylosing spondylitis. Eur Spine J. 2005. 14: 401-8
4. Jacobs WB, Fehlings MG. Ankylosing spondylitis and spinal cord injury: Origin, incidence, management, and avoidance. Neurosurg Focus. 2008. 24: E12
5. Ma J, Wang C, Zhou X, Zhou S, Jia L. Surgical therapy of cervical spine fracture in patients with ankylosing spondylitis. Medicine (Baltimore). 2015. 94: e1663
6. Rustagi T, Drazin D, Oner C, York J, Schroeder GD, Vaccaro AR. Fractures in spinal ankylosing disorders: A narrative review of disease and injury types, treatment techniques, and outcomes. J Orthop Trauma. 2017. 31: S57-74
7. Smith JA. Update on ankylosing spondylitis: Current concepts in pathogenesis. Curr Allergy Asthma Rep. 2015. 15: 489
8. Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: A systematic review of the literature on treatment, neurological status and complications. Eur Spine J. 2009. 18: 145-56