- Department of Neurosurgery, Vydehi Institute of Medical Sciences and Research Centre, Bengaluru, Karnataka, India.
Correspondence Address:
Manpreet Singh Banga, Department of Neurosurgery, Vydehi Institute of Medical Sciences and Research Centre, Bengaluru, Karnataka, India.
DOI:10.25259/SNI_1043_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Raj Swaroop Lavadi, B. V. Sandeep, Manpreet Singh Banga, Sangamesh Halhalli, Anantha Kishan. Spinal intramedullary tuberculoma in a 3-year-old girl. 14-Dec-2021;12:609
How to cite this URL: Raj Swaroop Lavadi, B. V. Sandeep, Manpreet Singh Banga, Sangamesh Halhalli, Anantha Kishan. Spinal intramedullary tuberculoma in a 3-year-old girl. 14-Dec-2021;12:609. Available from: https://surgicalneurologyint.com/surgicalint-articles/11289/
Abstract
Background: Spinal intramedullary tuberculoma (IMT) is a rare manifestation of extrapulmonary tuberculosis (TB). Presentation of TB in the pediatric age group is a significant contributor to mortality.
Case Description: A young vaccinated girl presented to the neurosurgery department with difficulty walking and urinary incontinence. A magnetic resonance imaging performed outside the hospital showed a hyperintense intramedullary lesion extending from T6 to T9. The patient underwent T6–T9 laminoplasty with intramedullary lesion decompression under neuromonitoring. The dense adherence of the lesion to the cord and nerve roots permitted only debulking. Histopathological examination confirmed the diagnosis of tuberculoma. The patient was started on antitubercular treatment and was then subsequently discharged. After 8 months, the patient was reviewed and showed improvement in her symptoms and complete resolution of the lesion on imaging. The patient has now developed hydrocephalus on the latest computed tomography imaging, which may be due to tubercular meningitis or arachnoiditis.
Conclusion: Complete resolution of spinal IMT is possible with a combined treatment approach.
Keywords: Antitubercular treatment, Pediatric spine, Spinal intramedullary lesion, Tuberculoma
BACKGROUND
Tuberculosis (TB) is one of the top 10 causes of under-5 mortality worldwide.[
CASE DESCRIPTION
A 3-year-old girl was brought by her parents to the neurosurgery department with complaints of difficulty walking for 4 months. The patient had a backward bending posture while walking. She swayed to one side and dragged her right lower limb. She also had difficulty wearing her slippers. She was not able to bend forward or sit for a long duration of time. Ten months ago, she had a history of headaches that lasted for a week. The patient also had urinary incontinence for 4 months. The patient had one episode of seizures post which she developed lower limb weakness. There was no history of trauma to the spine and no history of coming in contact with a patient who had TB. The patient was vaccinated according to the World Health Organization schedule. The patient had a history of pneumonia at the age of 1 month, following which she was admitted to the intensive care unit for 1 week.
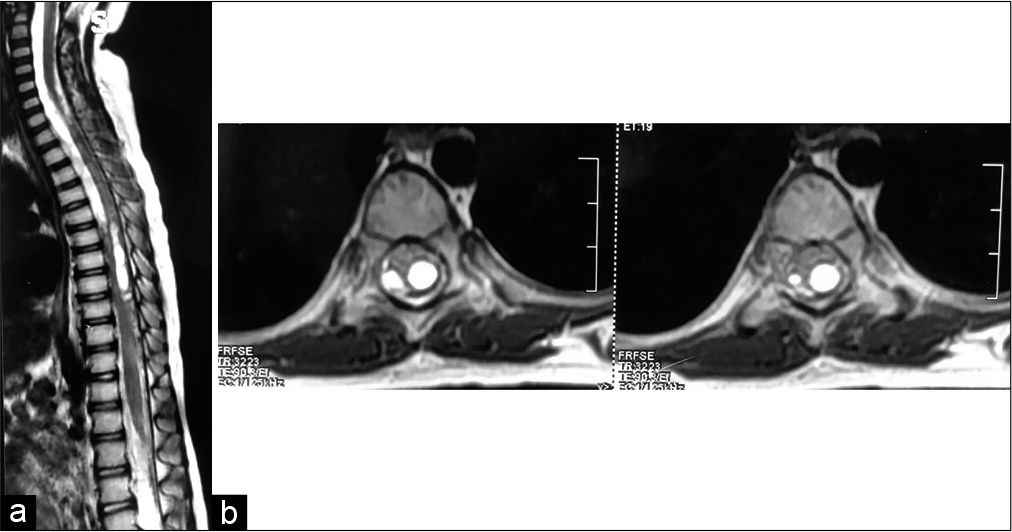
On examination, vitals were stable. Neurological examination showed that the tone of both lower limbs was increased. Plantar reflexes were extensor bilaterally. A magnetic resonance imaging (MRI) from an outside clinic showed a hyperintense intramedullary lesion, on T2W imaging, from T6 to T9 [
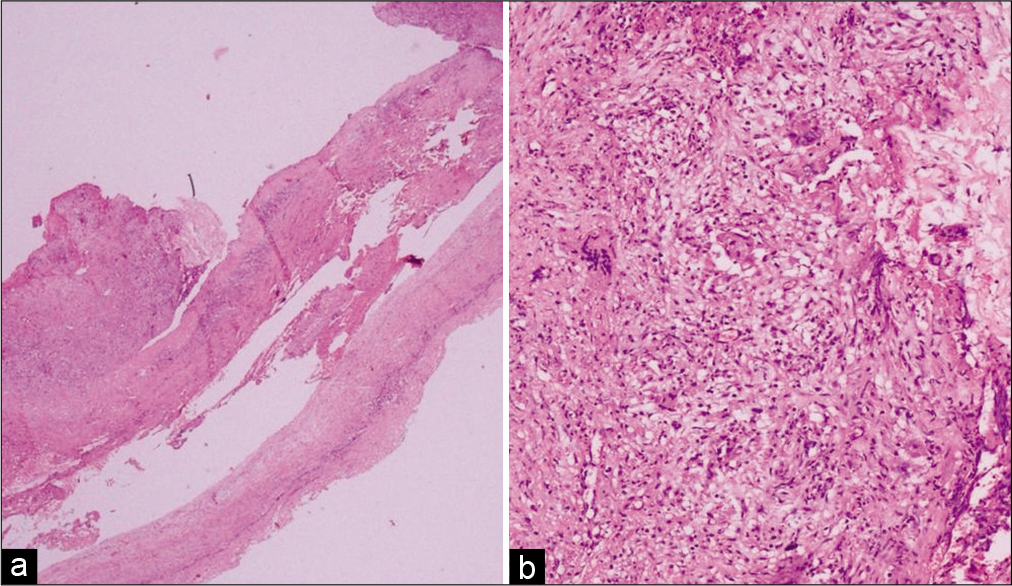
Figure 3:
(a) Low-power view (×20) of thickened and hyalinized connective tissue (meninges) strips with infiltration by large nodular foci of dense inflammation. The slide was stained with hematoxylin and eosin. (b) A closer view (×200) revealed coalescing loose epithelioid cell granulomas and scattered Langhan’s multinucleated giant cells on a background of lymphocytes and plasma cells. The slide was stained with hematoxylin and eosin.
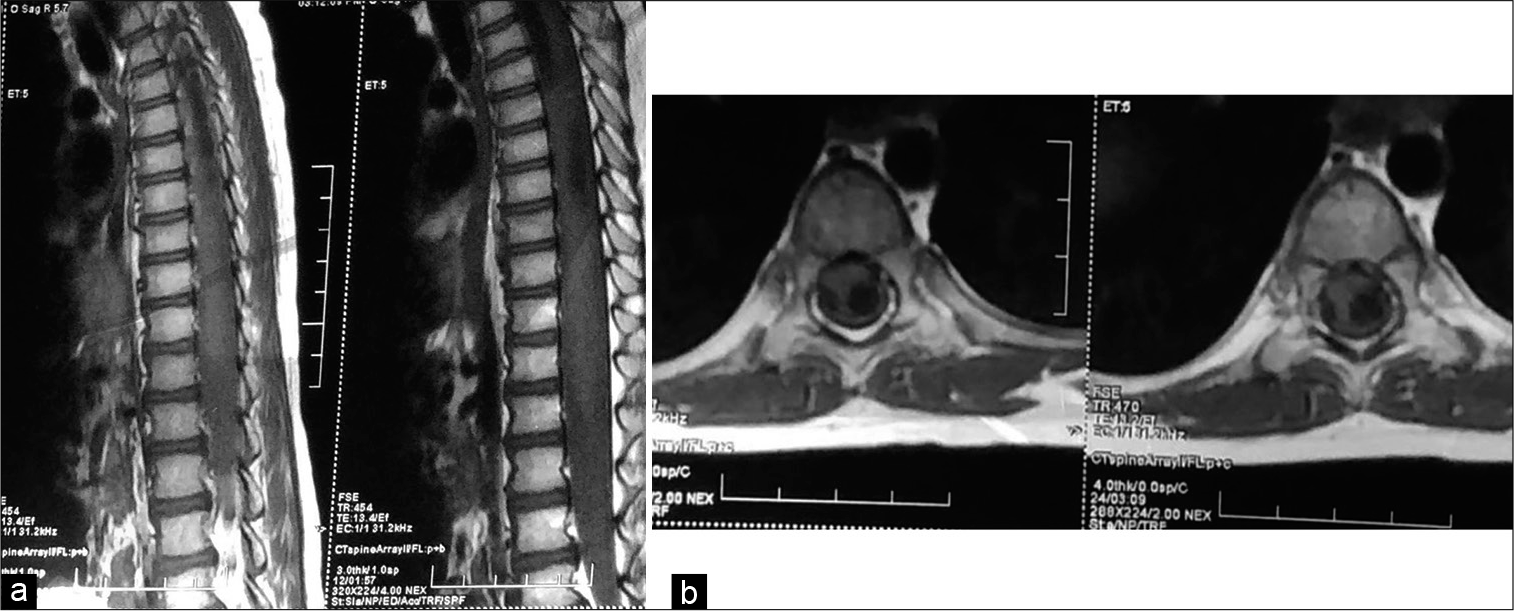
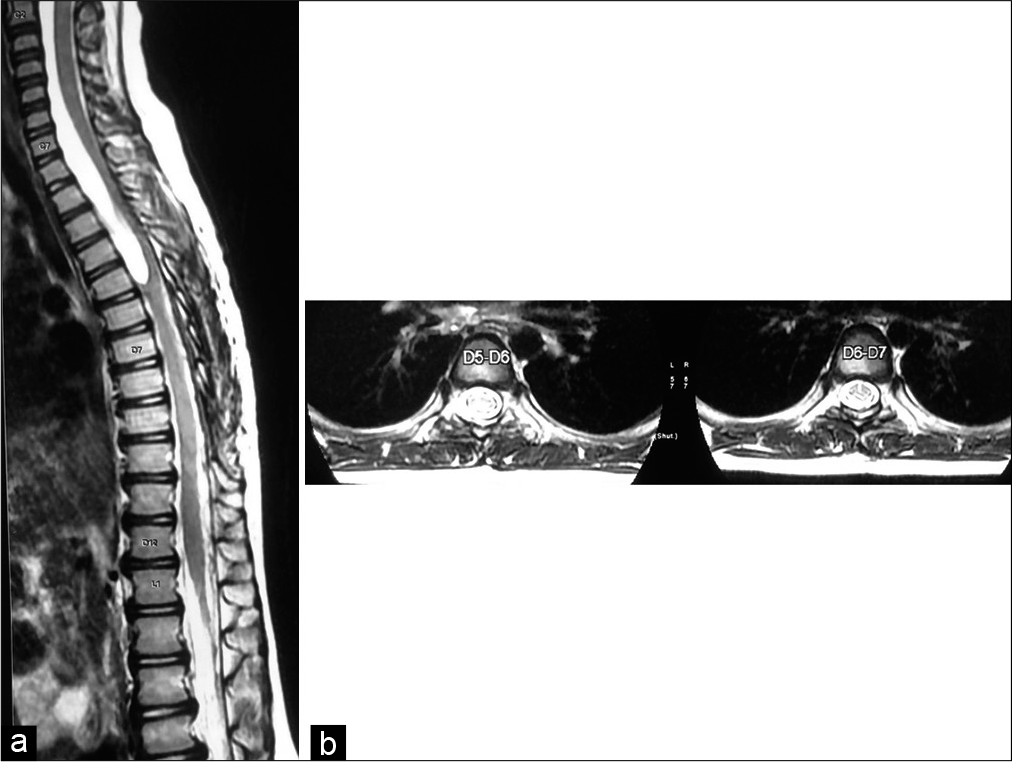
The diagnosis was then established. A pulmonology consultation for initiation of antitubercular treatment (ATT) was taken. The child was started on ATT and was subsequently discharged after being symptomatically better. The patient was reviewed 8 months after her initial visit while still on ATT, and she showed improvement in her gait abnormalities and is walking with support. The review scans [
Figure 5:
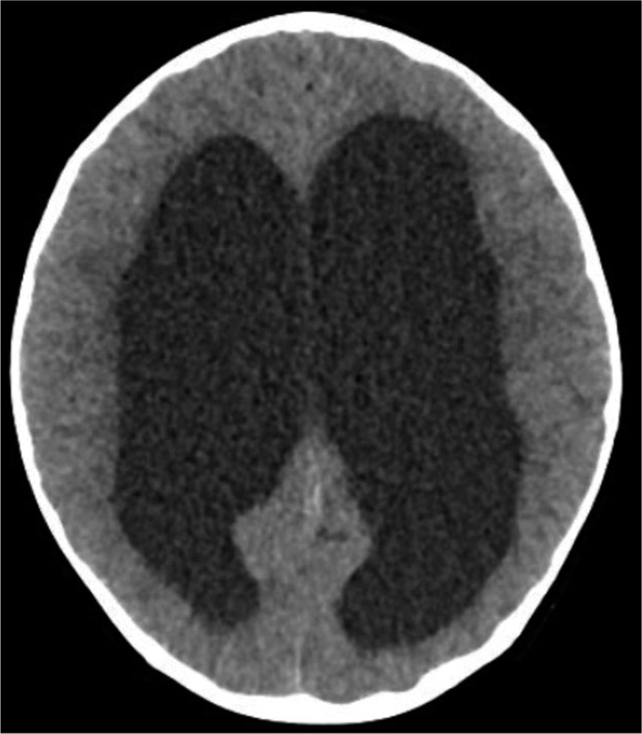
Computed tomography brain taken at the 8-month review showing features suggestive of noncommunicating hydrocephalus. There is dilation of the fourth ventricle, aqueduct, third ventricle, and bilateral lateral ventricles with transependymal cerebrospinal fluid seepage. There is no dilation of the foramina of Luschka or Magendie. We believe that this was caused as a result of tubercular meningitis or arachnoiditis.
DISCUSSION
Spinal TB is a common site of extrapulmonary TB, accounting for approximately 50% of skeletal TB.[
MRI is the imaging modality of choice for spinal IMT.[
Kulkarni et al.[
In addition, our diagnosis was confirmed by biopsy and subsequent histopathological examination.
We are aware that other granulomatous conditions share some similar microscopic findings as TB, such as sarcoidosis.[
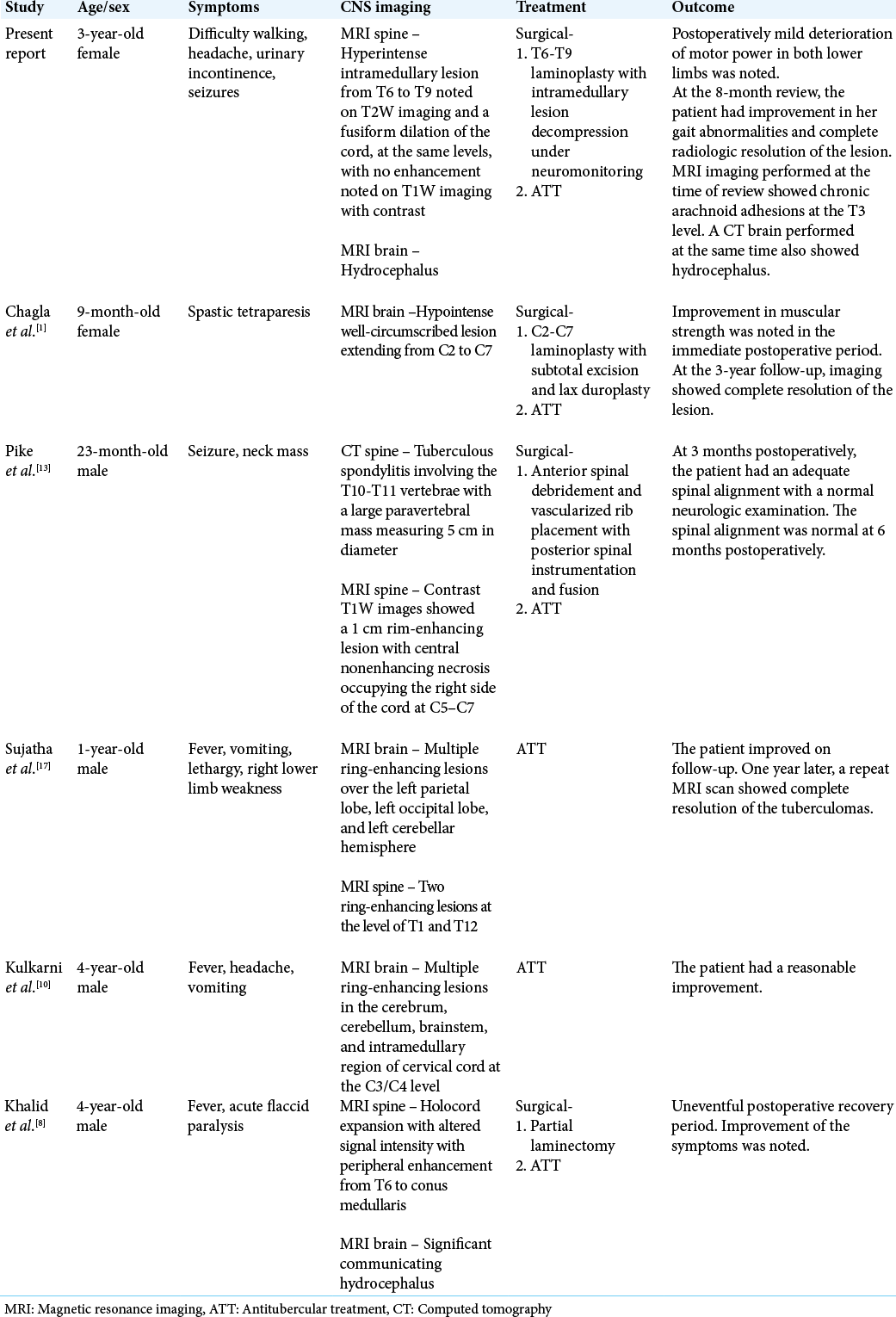
Four of the previously mentioned cases of IMT have been recorded in India.[
Continuation of the ATT will be required to address the arachnoid adhesions. Further follow-up will be required to ensure the resolution of this new finding and prevent possible post-tubercular kyphosis.[
CONCLUSION
IMTs are a rare spinal manifestation of TB, especially in the under-5 category. Tuberculomas are more likely to occur in the brain rather than the spine. The treatment depends on the presentation of the patient, radiologic findings, and the surgeon’s decision. We present this case to further the accounts made of this infrequent diagnosis and show that complete resolution of IMT is possible with a combined treatment approach.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Chagla AS, Udayakumaran S, Balasubramaniam S. Cervical intramedullary tuberculoma in an infant. J Neurosurg Pediatr. 2007. 106: 243
2. Dodd PJ, Yuen CM, Sismanidis C, Seddon JA, Jenkins HE. The global burden of tuberculosis mortality in children: A mathematical modelling study. Lancet Glob Health. 2017. 5: e898-906
3. Dunn RN, Husien MB. Spinal tuberculosis: Review of current management. Bone Joint J. 2018. 100B: 425-31
4. Garg RK, Somvanshi DS. Spinal tuberculosis: A review. J Spinal Cord Med. 2011. 34: 440-54
5. Ghane V, Shanbag P, Meshram A. Coexisting spinal intramedullary and intracranial tuberculomas in an immunocompetent child. J Pediatr Neurosci. 2019. 14: 143-7
6. Gupta D, Agarwal R, Aggarwal AN, Jindal SK. Sarcoidosis and tuberculosis: The same disease with different manifestations or similar manifestations of different disorders. Curr Opin Pulm Med. 2012. 18: 506-16
7. Gupta SK. Pediatric sarcoidosis in India. Indian J Pediatr. 2001. 68: 931-5
8. Khalid M, Khalid S, Mittal S, Ahmad U. Intramedullary tubercular abscess with syrinx formation. J Pediatr Neurosci. 2012. 7: 61-3
9. Knobbe K, Gaines M. Intramedullary tuberculoma of the spinal cord: A case report. Kansas J Med. 2020. 13: 300-3
10. Kulkarni K, Kaur S, Gupta V, Rastogi H. Concurrent intramedullary and intracranial tuberculomas in a child with tubercular meningitis. BMJ Case Rep. 2010. 2010: bcr12-2009.2569
11. Lu M. Imaging diagnosis of spinal intramedullary tuberculoma: Case reports and literature review. J Spinal Cord Med. 2020. 33: 159-62
12. Meegada S, Gyamfi R, Muppidi V, Dandu V, Challa T. Multiple intracranial tuberculomas with an intra-medullary spinal cord tuberculoma in a pediatric patient. Cureus. 2020. 12: 1-7
13. Pike J, Steinbok P, Reilly CW. Cervical intramedullary tuberculoma and tuberculous kyphosis in a 23-month-old child: Case report. Can J Surg. 2005. 48: 247-50
14. Rajasekaran S. The natural history of post-tubercular kyphosis in children. Radiological signs which predict late increase in deformity. J Bone Joint Surg Br. 2001. 83: 954-62
15. Ramos JM, Pérez-Butragueño M, Tesfamariam A, Reyes F, Tiziano G, Endirays J. Comparing tuberculosis in children aged under 5 versus 5 to 14 years old in a rural hospital in Southern Ethiopia: An 18-year retrospective cross-sectional study. BMC Public Health. 2019. 19: 1-9
16. Shah KK, Pritt BS, Alexander MP. Histopathologic review of granulomatous inflammation. J Clin Tuberc Other Mycobact Dis. 2017. 7: 1-12
17. Sujatha S, Ravsekar CV, Lakshmi S, Kumarasamy K. A rare case of intracranial and intramedullary tuberculomas. Indian J Pract Pediatr. 2011. 13: 105-8
18. Swaminathan S, Sachdeva KS. Treatment of childhood tuberculosis in India. Int J Tuberc Lung Dis. 2015. 19: 43-6