- Harvard Medical School, Boston, Massachusetts, Boston, United States.
- Department of Neurosurgery, Brigham and Women’s Hospital, Boston, United States.
Correspondence Address:
John H. Chi, Department of Neurosurgery, Brigham and Women’s Hospital, Boston, United States.
DOI:10.25259/SNI_479_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sarah Elizabeth Blitz1, Melissa Ming Jie Chua2, Neil Vernon Klinger2, John H. Chi2. Spinal osteomyelitis and epidural abscess caused by ureterovertebral fistula: A case report. 01-Jul-2022;13:279
How to cite this URL: Sarah Elizabeth Blitz1, Melissa Ming Jie Chua2, Neil Vernon Klinger2, John H. Chi2. Spinal osteomyelitis and epidural abscess caused by ureterovertebral fistula: A case report. 01-Jul-2022;13:279. Available from: https://surgicalneurologyint.com/surgicalint-articles/11691/
Abstract
Background: Ureteral fistulas are abnormal connections between the ureters and other organs. Maintaining a high index of suspicion is important because they can precipitate dangerous complications such as sepsis and renal failure. Connections to a vertebral body have only been documented in the setting of trauma. Here, we present a 67-year-old female with a ureterovertebral fistula extending into the L3 vertebral body.
Case Description: A 67-year-old female with a history of endometrial adenocarcinoma underwent surgery and radiation therapy complicated by a right ureteral obstruction requiring stent placement. Five months later, she developed back pain and MR-documented L2-L4 level osteomyelitis/discitis with a psoas phlegmon/abscess, which required drainage. A fistula was later identified between the right ureter and the psoas phlegmon. Despite percutaneous nephrostomy placement and aggressive IV antibiotic treatment, she was readmitted for persistent signs of infection over the next few months during which time she was repeatedly and unsuccessfully treated with multiple antibiotics. Sixteen months following her original stent placement, she developed right leg weakness and urinary incontinence attributed to the MR-documented ureteropsoas fistula extending into the L3 vertebral body. Following a nephrectomy with ureteral ligation, an L3 anterior corpectomy with interbody fusion for discitis at both L2-L3 and L3-L4, and an L1-L5 posterolateral fusion, she was discharged to a rehabilitation center.
Conclusion: In patients with recurrent sepsis, osteomyelitis/discitis, or psoas abscess of unknown origin or who have a significant history (e.g., pelvic malignancy, radiation, and instrumentation), it is important to consider urodynamic testing to look for a ureteral leak or fistula.
Keywords: Epidural abscess, Osteomyelitis, Ureterovertebral fistula
INTRODUCTION
Urinary tract fistulas, abnormal connections between the urinary and other organ systems, can have a wide variety of causes, anatomic locations, organ involvement, and clinical features. Typical precipitating events include iatrogenic injury, trauma, inflammatory diseases, infection, malignancies, or radiation. Fistulas including the ureters, specifically, usually connect to the intestines, vascular system, skin, or female reproductive tract.[
CASE DESCRIPTION
A 67-year-old female with endometrial adenocarcinoma with known metastases to the liver and spine underwent a total abdominal hysterectomy, bilateral salpingooophorectomy, omentectomy, and radiation therapy. Postoperatively, the patient developed malignant right ureteral obstruction with hydronephrosis requiring ureteral stent placement. Five months later, she returned to the hospital with worsening back pain. The spine MR revealed abnormal signal enhancement ventrally between the L2-L4 levels consistent with osteomyelitis, L2-L3/L3-L4 discitis, and left psoas muscle phlegmon. Interventional radiology (IR) percutaneously drained the abscess, and cultures grew Bacteroides fragilis and Streptococcus mitis.
Over the next 5 months, she was readmitted 3 times with recurrent infections despite multiple oral and IV courses of antibiotics. The CT urogram of her abdomen/pelvis revealed a right ureteral fistula extending to the psoas muscle. Blood cultures revealed Bacteroides vulgaris, Enterococcus faecalis, and Aerococcus urinae. Despite the placement of a diverting percutaneous nephrostomy and exchanging ureteral stent, the infections persisted. Urine cultures showed Citrobacter, Candida tropicalis, and mold speciation consistent with Fusarium species.
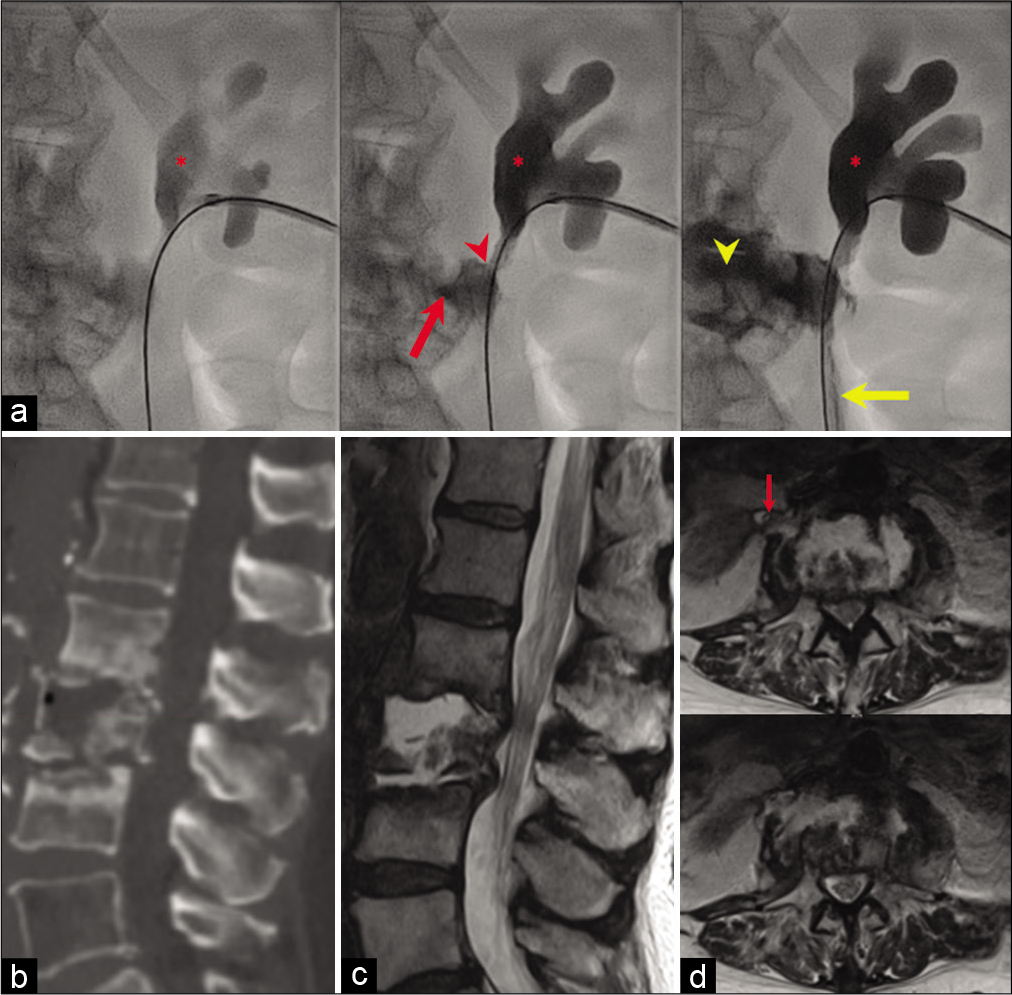
Sixteen months after original stent placement, she was readmitted with the right lower extremity weakness and increased urinary incontinence. The MRI demonstrated progression of her osteomyelitis and discitis from L2-L4 with significant osseous destruction of L3 and spinal cord stenosis due to osseous retropulsion. A nephroureterogram with stent exchange demonstrated a worsening ureteropsoas fistula with contrast extravasation into the osteomyelitic cavity within the L3 body (i.e., progression to ureterovertebral fistula) [
Figure 1:
Postinfectious ureterovertebral fistula. (a) IR nephrogram (left to right, during injection; red asterisk demarcates the right renal pelvis; yellow arrow demarcates the right ureter) obtained during nephrostomy exchange demonstrating extravasation of contrast and opacification of the abnormal connections to the psoas phlegmon (red arrowhead) and adjacent osteomyelitic L3 vertebral body (red arrow) consistent with ureterovertebral fistula. Sagittal CT (b) and T2-weighted MRI (c) demonstrating extensive osseous destruction at L3. (d) Axial T2-weighted MRI images demonstrating continuity of the right ureter/renal pelvis containing her ureteral stent (red arrow) and the cystic space in the L3 vertebral body.
DISCUSSION
Connections between ureters and vertebral bodies are extraordinarily rare, and they are almost uniformly due to trauma. Dagain et al. discussed a ureterovertebral fistula to L3 after a vertebromedullary gunshot wound. The fistula was identified by CT.[
Diagnostic testing for urinary fistulas
Diagnosis of urinary fistulas can be made through uroradiological examinations. Fistulography is the most direct means of fistula visualization and should be used when feasible (e.g., cutaneous fistulas).[
Difficulty with diagnosing ureteral fistulas
Ureteral leaks or fistulas can go undiagnosed for protracted periods of time at which point they often become severely symptomatic. Suspicion should be high, especially in patients with a history of cancer surgery. Note, the patient presented had an original pelvic malignancy, radiation, and prior instrumentation that all put her at high risk for the delayed complications that occurred several months later.
CONCLUSION
In patients with recurrent sepsis, osteomyelitis/discitis, or psoas abscess of unclear origin, it is important to consider urodynamic testing to evaluate whether these findings may be attributed to a ureteral leak or fistula.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abboudi H, Ahmed K, Royle J, Khan MS, Dasgupta P, N’Dow J. Ureteric injury: A challenging condition to diagnose and manage. Nat Rev Urol. 2013. 10: 108-15
2. Dagain A, Dulou R, Blondet E, de Soultrait F, Debien B, Pernot BG. Vertebromedullary wound with ureteral fistula. Mil Med. 2007. 172: 335-7
3. Kahokehr AA, Boysen WR, Schild MH, Nosé BD, Huang J, Eward W. Urinary pubic symphysis fistula leads to histopathologic osteomyelitis in prostate cancer survivors. Urology. 2021. 148: 297-301
4. Madden-Fuentes RJ, Peterson AC. Pubic bone osteomyelitis and pubosymphyseal urinary fistula: A poorly recognized complication in prostate cancer survivors. Oncology (Williston Park). 2017. 31: 169-73
5. Matsushita K, Ginsburg L, Mian BM, De E, Chughtai BI, Bernstein M. Pubovesical fistula: A rare complication after treatment of prostate cancer. Urology. 2012. 80: 446-51
6. Miguel BR, de Avila SR, Ribo MA, Cárdenas JD, Chacón JI, Esteban CE. Myositis and osteomyelitis due to radiotherapy-related fistulae in locally advanced cervical cancer. J Case Rep Images Obstet Gynecol. 2019. 5: 100051
7. Palma LD. What is left of iv urography?. Eur Radiol. 2001. 11: 931-9
8. Salunke AA, Nambi GI, Manoharan A. Osteomyelits of the pubic bone with vesicocutaneous vesicovaginal fistula: A delayed complication of post-cervical cancer radiotherapy. Niger Med J. 2014. 55: 83-5
9. Sexton SJ, Lavien G, Said N, Eward W, Peterson AC, Gupta RT. Magnetic resonance imaging features of pubic symphysis urinary fistula with pubic bone osteomyelitis in the treated prostate cancer patient. Abdom Radiol. 2019. 44: 1453-60
10. Soundararajan DC, Maheswaran A, Kumarasamy D, Shetty AP, Kanna RM, Rajasekaran S. Delayed presentation of urinoma mimicking spondylodiscitis secondary to ureteric injury following carrot stick fracture in ankylosing spondylitis. Eur Spine J. 2020. 29: 171-5
11. Sunday-Adeoye I, Ekwedigwe KC, Isikhuemen ME, Eliboh MO, Yakubu EN, Daniyan BC. Intravenous urography findings in women with ureteric fistula. Pan Afr Med J. 2018. 30: 203
12. Yu NC, Raman SS, Patel M, Barbaric Z. Fistulas of the genitourinary tract: A radiologic review. Radiographics. 2004. 24: 1331-52