- Department of Neurosurgery, Padjadjaran University, Bandung, West Java, Indonesia.
Correspondence Address:
Rully Hanafi Dahlan, Department of Neurosurgery, Padjadjaran University, Bandung, West Java, Indonesia.
DOI:10.25259/SNI_1201_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Rully Hanafi Dahlan, Sevline Estethia Ompusunggu, Yustinus Robby Budiman Gondowardojo, Radityo Priambodo, Samuel Willyarto Anugerah. Spinal tuberculosis: A case series and a literature review. 13-May-2022;13:196
How to cite this URL: Rully Hanafi Dahlan, Sevline Estethia Ompusunggu, Yustinus Robby Budiman Gondowardojo, Radityo Priambodo, Samuel Willyarto Anugerah. Spinal tuberculosis: A case series and a literature review. 13-May-2022;13:196. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11594
Abstract
Background: Spinal tuberculosis (TB) is a common form of extrapulmonary TB. Although the first line of the treatment is anti-TB medications, patients with severe neurological deficits, spinal instability, and/or kyphotic deformity often warrant surgery. Here, we report five cases of spinal TB requiring operative intervention at Hasan Sadikin General Hospital, Bandung, Indonesia.
Case Description: We operated on five patients with spinal TB cases from 2019 to October 2021. In addition to appropriate medical management, all five patients successfully underwent laminectomy with or without posterior stabilization.
Conclusion: It is essential to establish the diagnosis and surgically manage patients with spinal TB early in the clinical course to minimize residual post-operative neurological deficits.
Keywords: Diagnosis, Management, Pott’s disease, Spinal tuberculosis, Spondylitis tuberculosis
INTRODUCTION
Tuberculosis (TB) is responsible for 1.3 million deaths annually.[
CASE DESCRIPTION
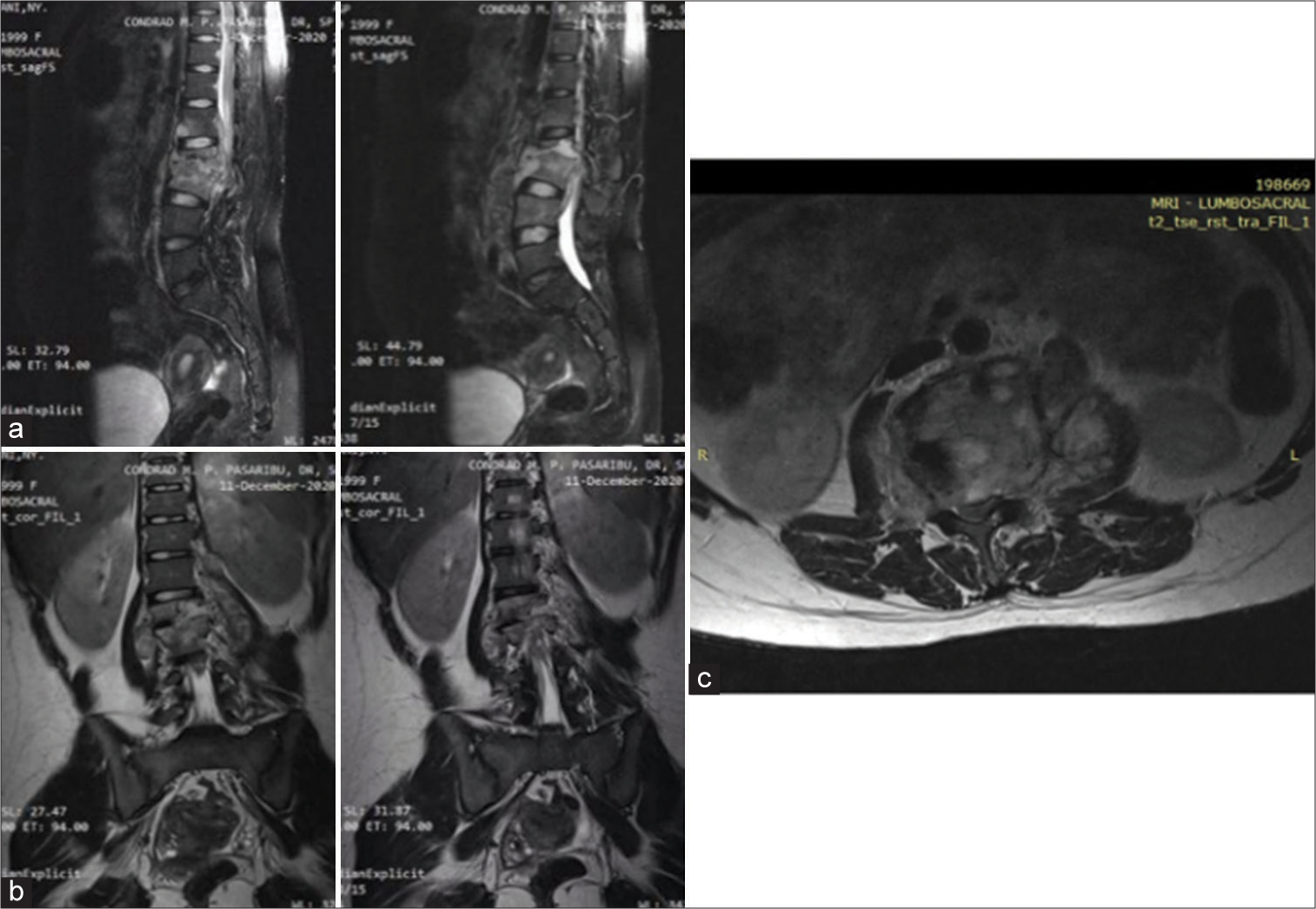
Five patients diagnosed with spinal TB with the average age are 25.8 years old, and included two males and three females [
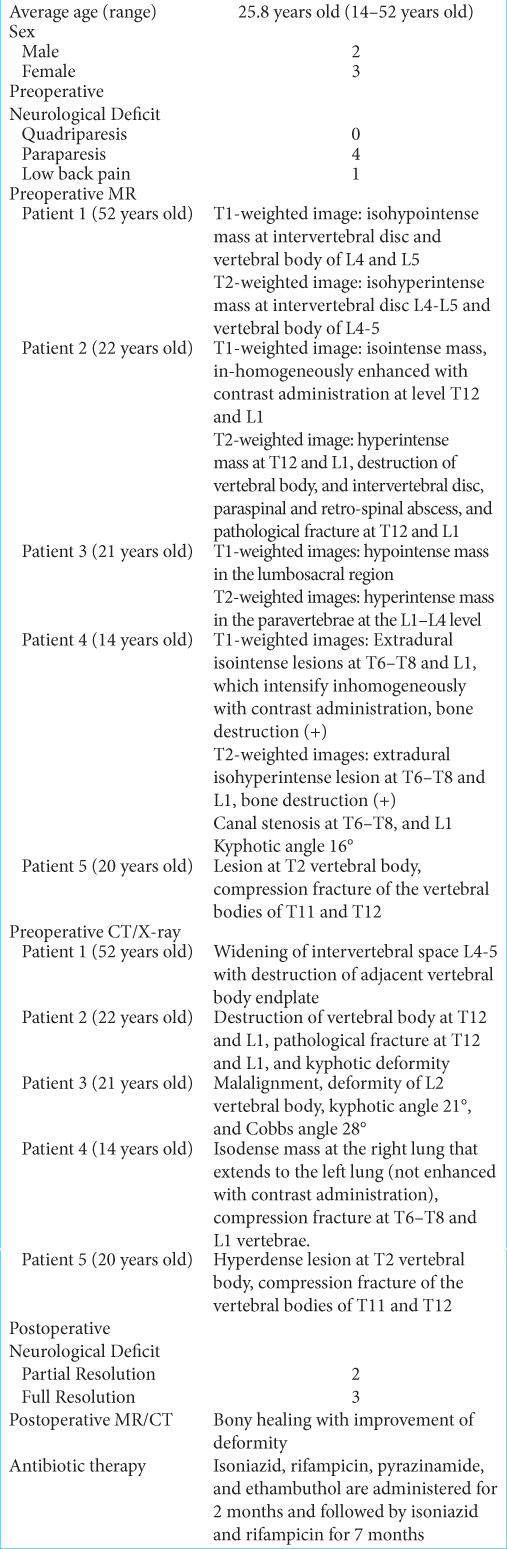
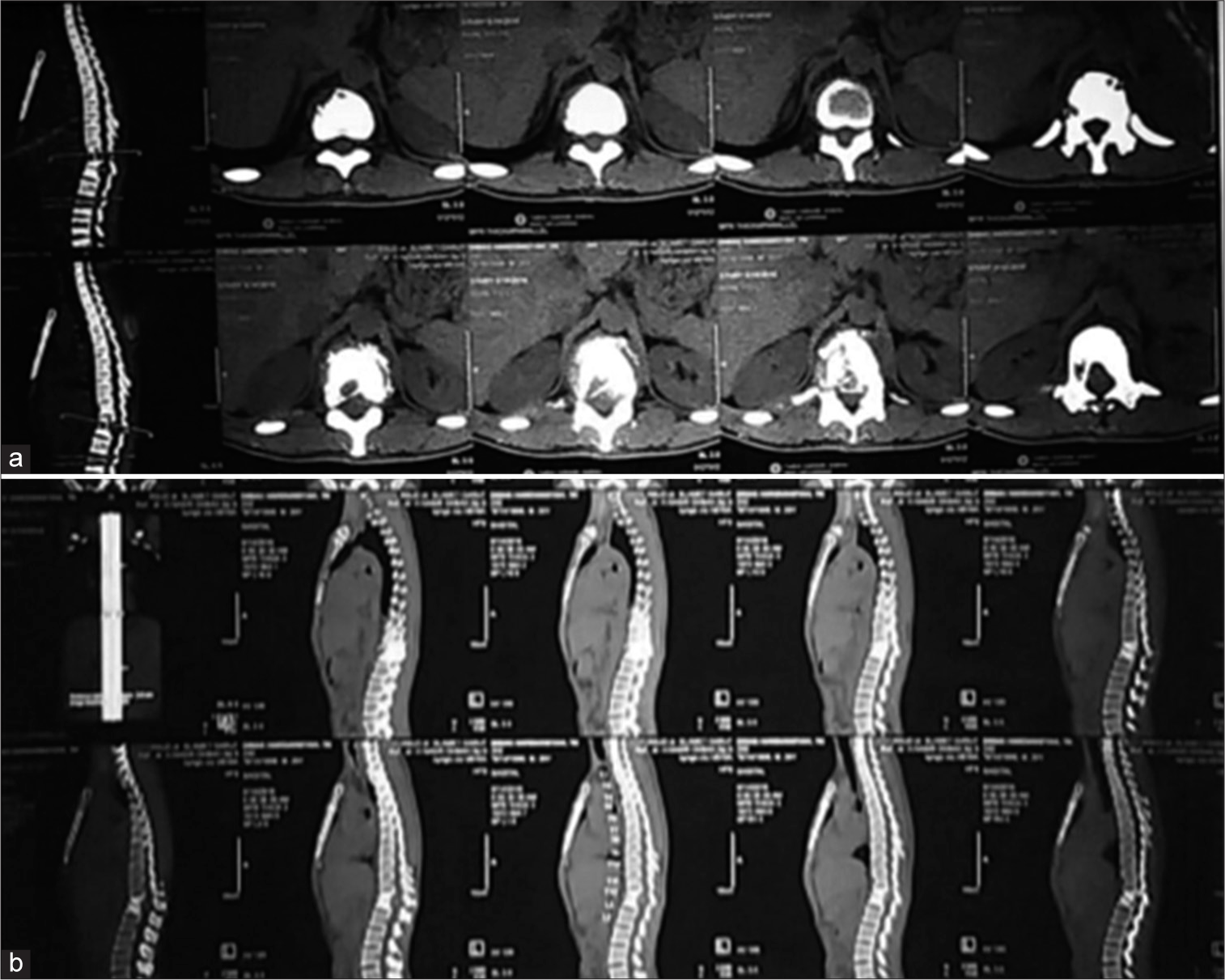
Figure 1:
Thoracolumbar MRI of spinal TB in 52-year-old male; (a)T1-weighted image showed isohypointense mass at intervertebral disc L4-L5 and vertebral body of L4-5; (b)T1-weighted image showed isohypointense mass which inhomogeneously enhanced with contrast administration at intervertebral disc L4-L5; (c)T2-weighted image showed isohyperintense mass at intervertebral disc L4-L5 and vertebral body of L4-5; (d) Coronal view; (e)Axial view.
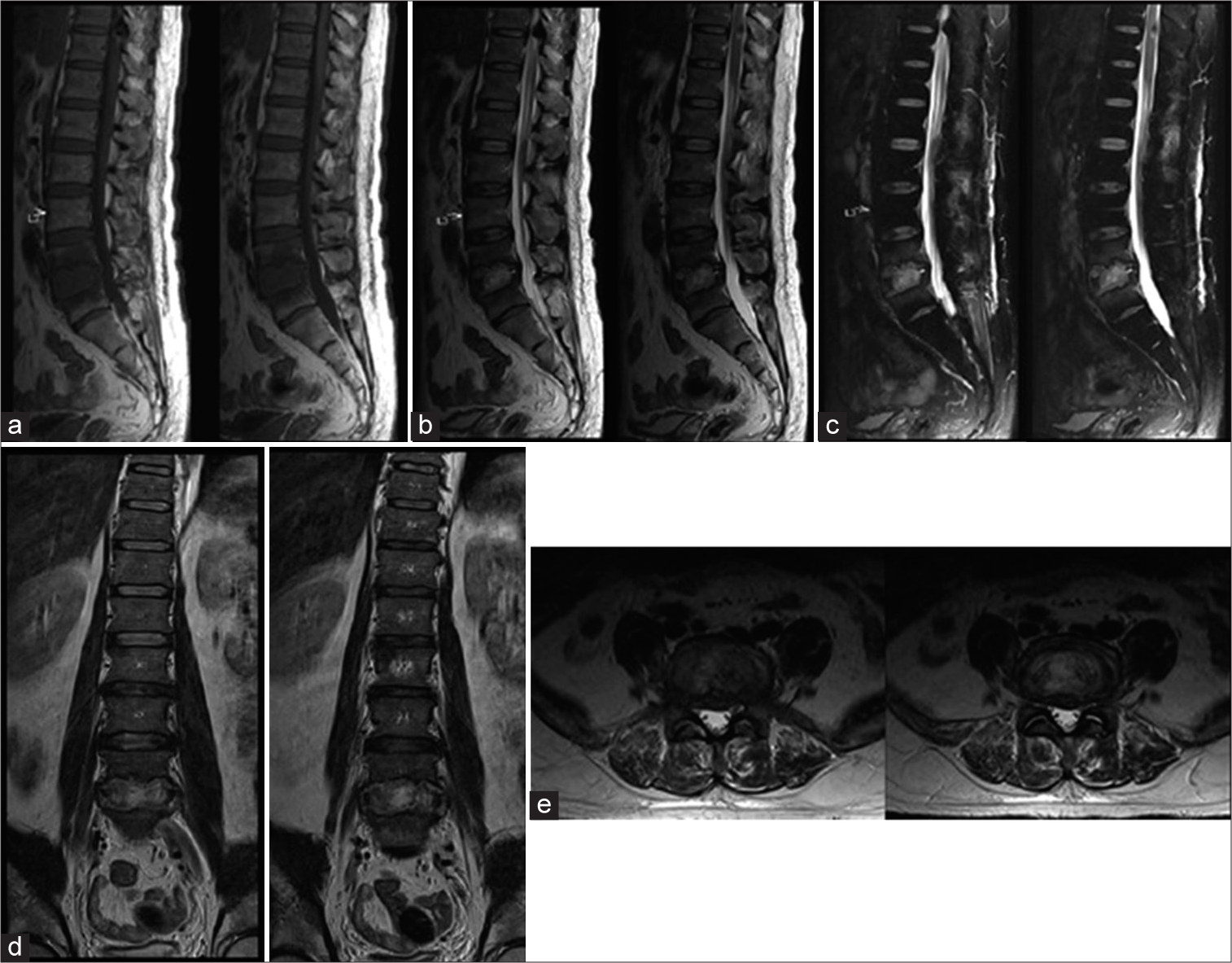
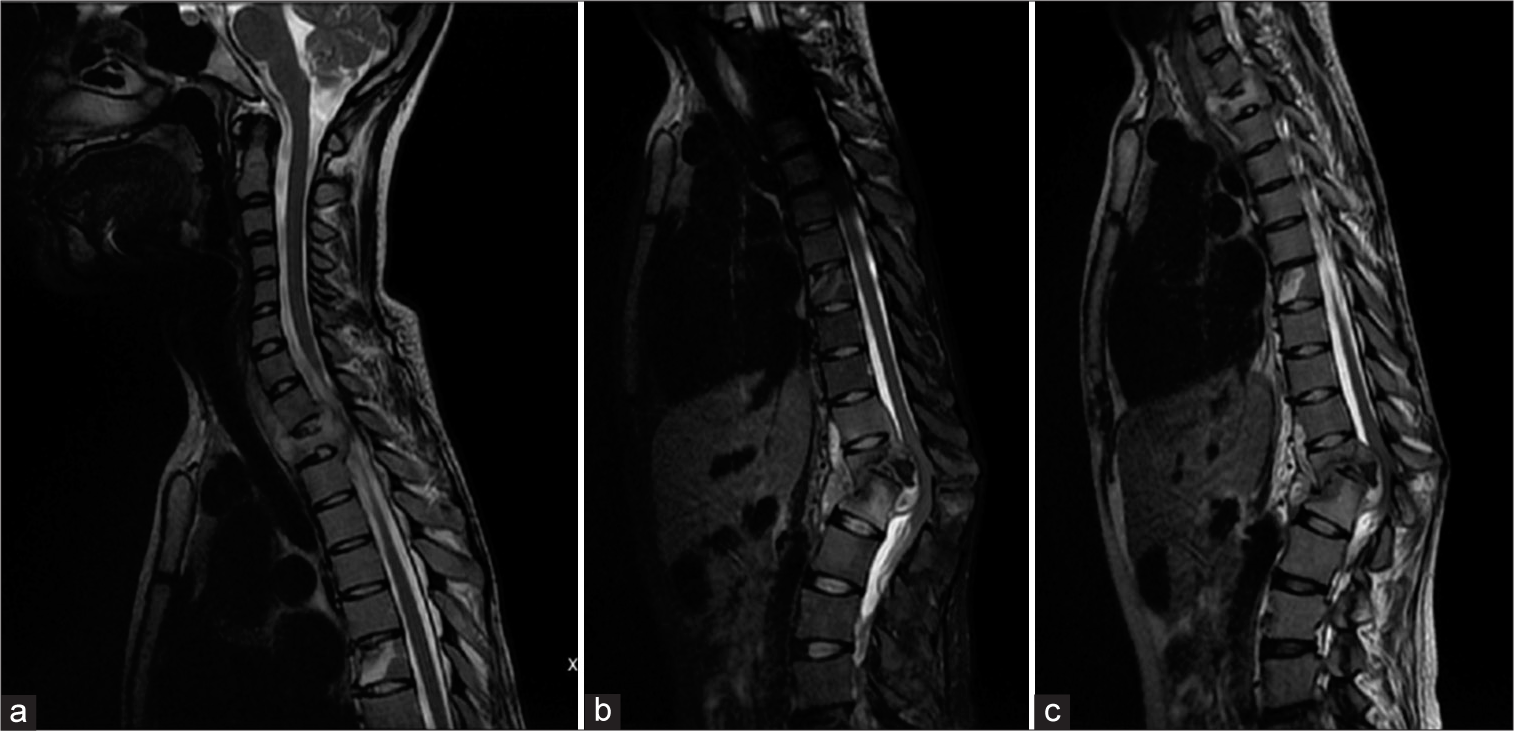
Figure 2:
(a-b) Thoracolumbar MRI in a 22-year-old male with spinal TB. T1-weighted image showed isointense mass which inhomogeneously enhanced with contrast administration at level T12-L1. T2-weighted image showed hyperintense mass at T12-L1, destruction of vertebral body, and intervertebral disc, paraspinal and retro-spinal abscess, and pathological fracture at T12 and L1.
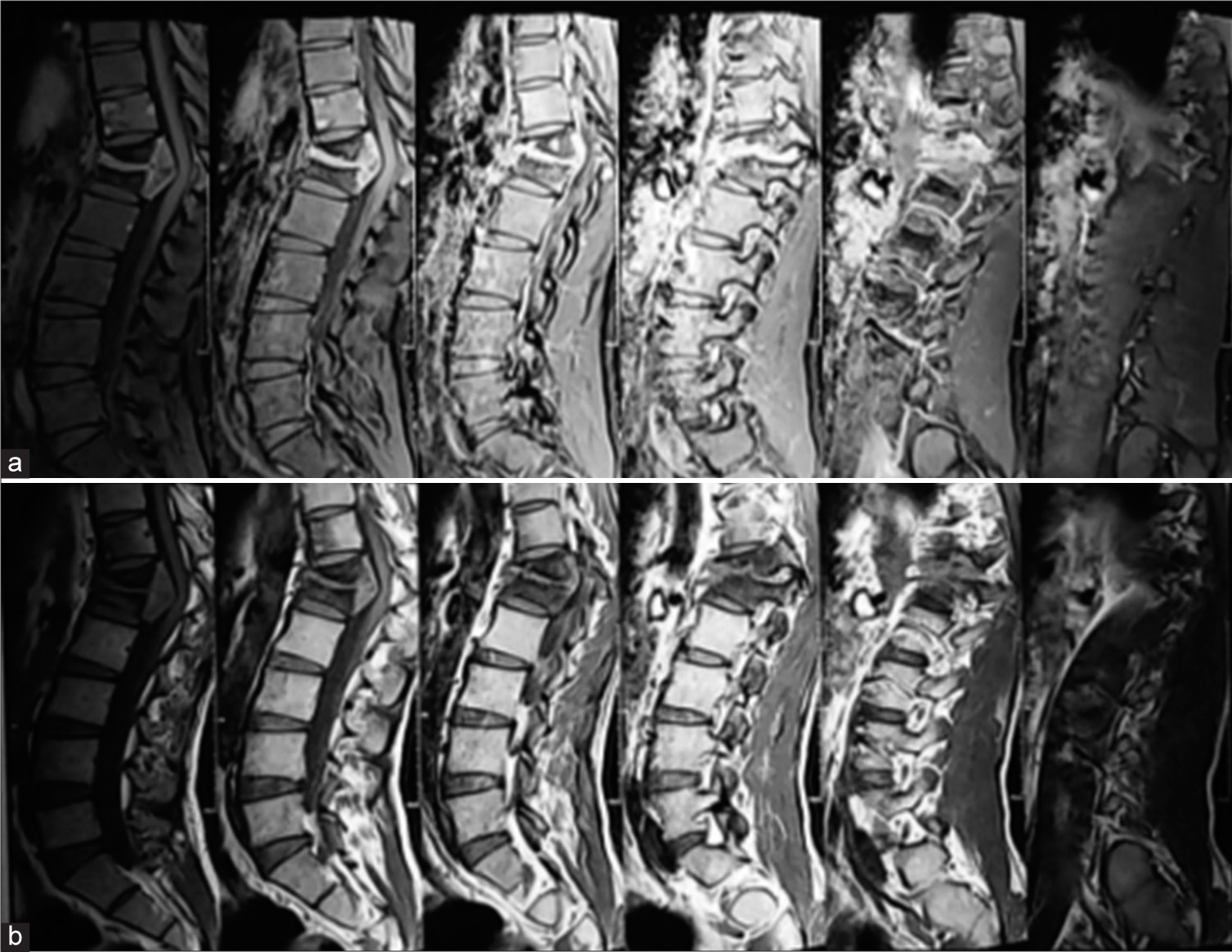
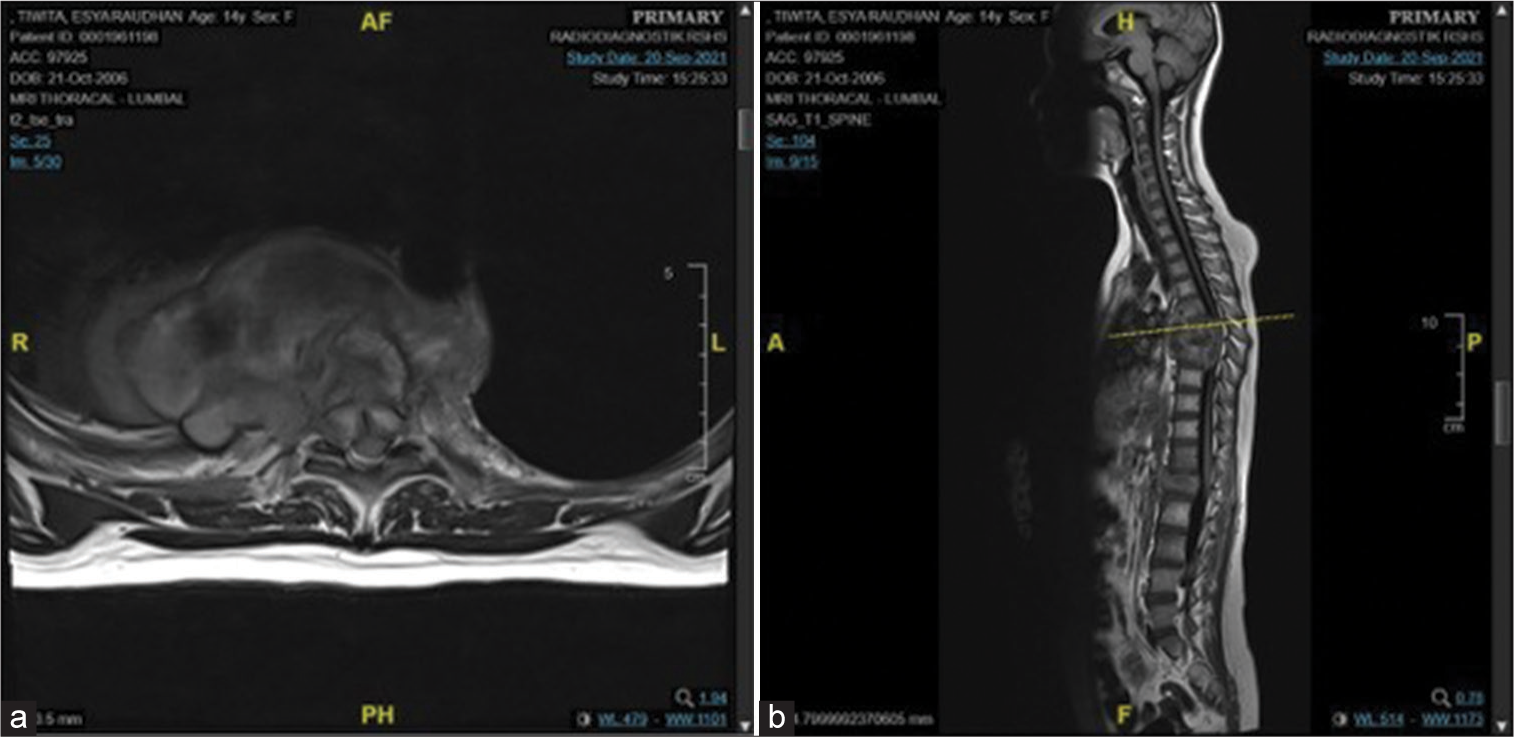
Figure 4:
MRI of spinal TB in a 14-year-old female. T1-weighted images showed extradural isointense lesions at T6–T8 and L1, which intensify inhomogeneously with contrast administration. Note also that there is bone destruction. T2-weighted images showed extradural isohyperintense lesion at T6–T8 and L1 with bone destruction, canal stenosis at T6-T8, and L1, and kyphotic angle 16°. (a) Axial view ; (b) Sagital view.
DISCUSSION
Medical treatment is the mainstay of the treatment for spinal TB, with surgical interventions indicated in certain circumstances.[
The literature describes three surgical approaches for treating spinal tuberculosis (TB): the anterior approach, the posterior approach, and the combined approach (combined anterior and posterior approach).[
Yang et al. provide evidence for anterior, posterior, and combined surgical approaches for spinal TB. However, the combined approaches require significantly longer operation times and more blood loss versus anterior alone procedures. Ultimately, Yang et al. concluded that posterior approaches offered better clinical outcomes.[
Spinal TB involving the thoracolumbar region is biomechanically challenging and the surgical options with thoracolumbar involvement are anterior debridement and reconstruction with posterior pedicle screws or a posterior- only approach.[
CONCLUSION
Spinal TB should optimally be quickly diagnosed and appropriately surgically managed (where needed) to achieve the best postoperative outcomes.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Benli IT, Kaya A, Acaroǧlu E. Anterior instrumentation in tuberculous spondylitis: Is it effective and safe?. Clin Orthop Relat Res. 2007. 60: 108-16
2. Bian Z, Gui Y, Feng F, Shen H, Lao L. Comparison of anterior, posterior, and anterior combined with posterior surgical treatment of thoracic and lumbar spinal tuberculosis: A systematic review. J Int Med Res. 2019. 48: 300060519830827
3. Dunn RN, Ben Husien M. Spinal tuberculosis review of current management. Bone Joint J. 2018. 100B: 425-31
4. Miller AG, Spicer PJ. Extrapulmonary tuberculosis: A case report involving the spine and soft tissues. Radiol Case Rep. 2021. 16: 2236-9
5. Rajasekaran S, Soundararajan DC, Shetty AP, Kanna RM. Spinal tuberculosis: Current concepts. Glob Spine J. 2018. 8: 96S-108
6. Shetty A, Kanna RM, Rajasekaran S. TB spine-current aspects on clinical presentation, diagnosis, and management options. Semin Spine Surg. 2016. 28: 150-62
7. Tuberculosis. Available from: https://www.who.int/news-room/fact-sheets/detail/tuberculosis [Last accessed on 2021 Oct 31].
8. Yang P, Zang Q, Kang J, Li H, He X. Comparison of clinical efficacy and safety among three surgical approaches for the treatment of spinal tuberculosis: A meta-analysis. Eur Spine J. 2016. 25: 3862-74