- Department of Neurosurgery, Atsugi City Hospital, Atsugi, Kanagawa, Japan.
- Department of Neurosurgery, Jikei University School of Medicine, Nishi-Shimbashi, Tokyo, Japan.
Correspondence Address:
Keiichiro Ohara
Department of Neurosurgery, Jikei University School of Medicine, Nishi-Shimbashi, Tokyo, Japan.
DOI:10.25259/SNI_268_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Keiichiro Ohara1, Tohru Terao1, Shotaro Michishita1, Kunitomo Sato1, Yuichi Sasaki1, Yuichi Murayama2. Spontaneous cerebrospinal fluid otorrhea and pneumocephalus on the contralateral side of the previous cranial surgery. 15-Aug-2020;11:245
How to cite this URL: Keiichiro Ohara1, Tohru Terao1, Shotaro Michishita1, Kunitomo Sato1, Yuichi Sasaki1, Yuichi Murayama2. Spontaneous cerebrospinal fluid otorrhea and pneumocephalus on the contralateral side of the previous cranial surgery. 15-Aug-2020;11:245. Available from: https://surgicalneurologyint.com/surgicalint-articles/10212/
Abstract
Background: Cerebrospinal fluid (CSF) leaks and pneumocephalus commonly occur due to head trauma or surgical procedures. Spontaneous CSF (sCSF) leaks, however, occur without any clear etiology and are relatively uncommon.
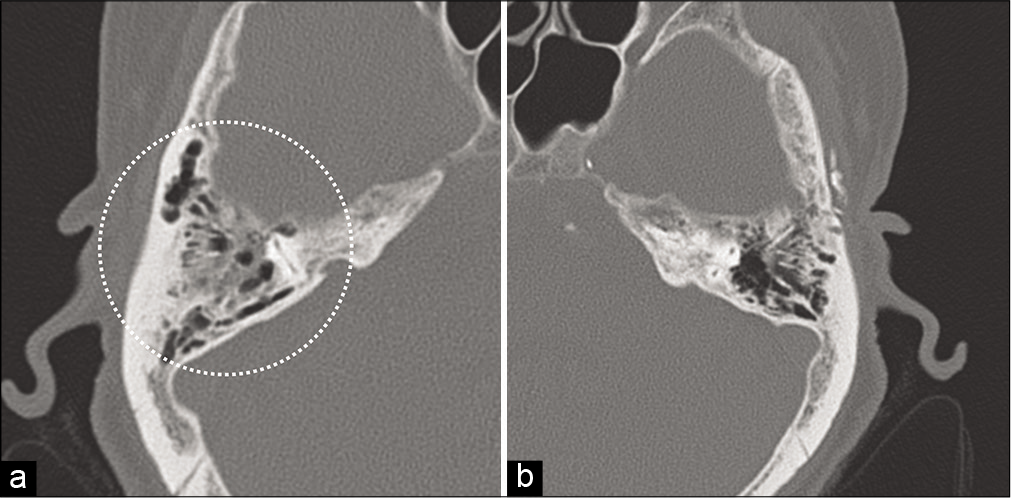
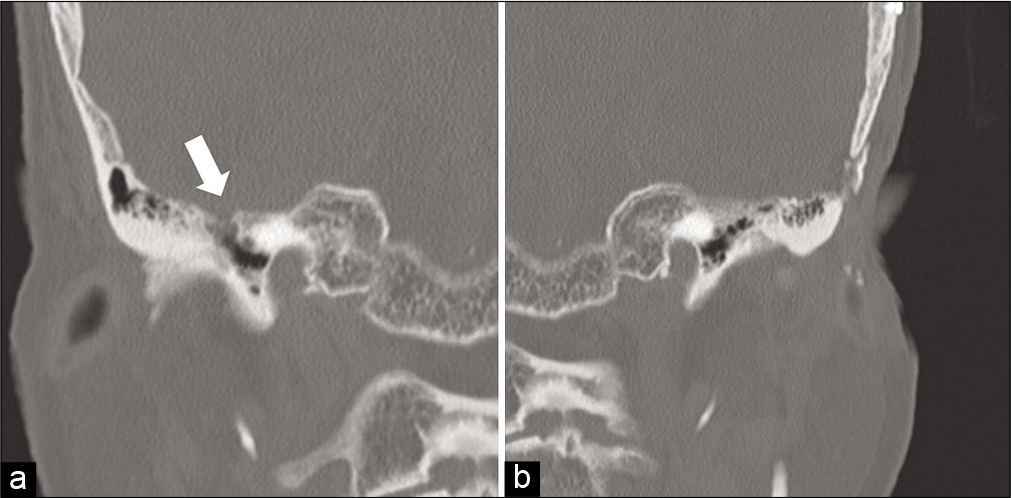
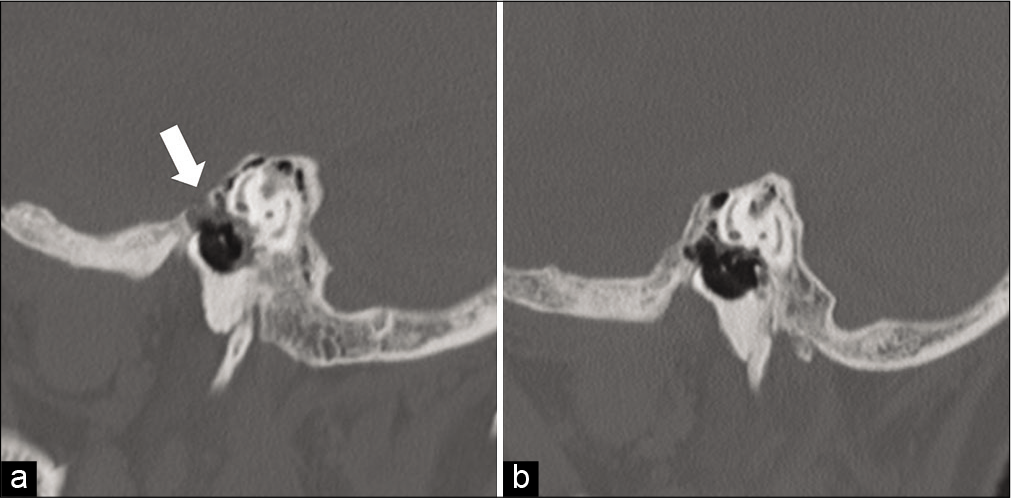
Case Description: An 84-year-old woman presented with the right-sided otorrhea. The patient had a history of a ventriculoperitoneal shunt placement following a subarachnoid hemorrhage treated by clip ligation of a left-sided ruptured cerebral aneurysm 7 years before presentation, with shunt catheter ligation after evidence of intraventricular pneumocephalus 6 years before presentation. At admission, computed tomography (CT) imaging of the head showed enlargement of the lateral ventricles, a right mastoid fluid collection, and a defect of the superior wall of the right petrous bone. We performed a right temporal craniotomy for the repair of the CSF leak. Intraoperatively, it was noted that temporal lobe parenchyma herniated into the mastoid air cells through lacerated dura and a partially defective tegmen mastoideum. The leak point was successfully obliterated with a pericranial graft and reinforced by a collagen sheet and fibrin glue. There was no recurrence of otorrhea postoperatively.
Conclusion: This report presents a very unique case of a patient with a CSF leak and pneumocephalus occurring on the contralateral side of a previous cranial surgery. We accurately identified the defect site with CT imaging and repaired the CSF leak by temporal craniotomy. Awareness of the mechanisms by which sCSF leaks can be caused by aberrant arachnoid granulations is imperative for neurosurgeons.
Keywords: Aberrant arachnoid granulation, Cerebrospinal fluid otorrhea, Pneumocephalus, Spontaneous cerebrospinal fluid leak
INTRODUCTION
Cerebrospinal fluid (CSF) leaks and pneumocephalus occur due to abnormal communication between the subarachnoid space and the adjacent paranasal sinuses.[
CASE PRESENTATION
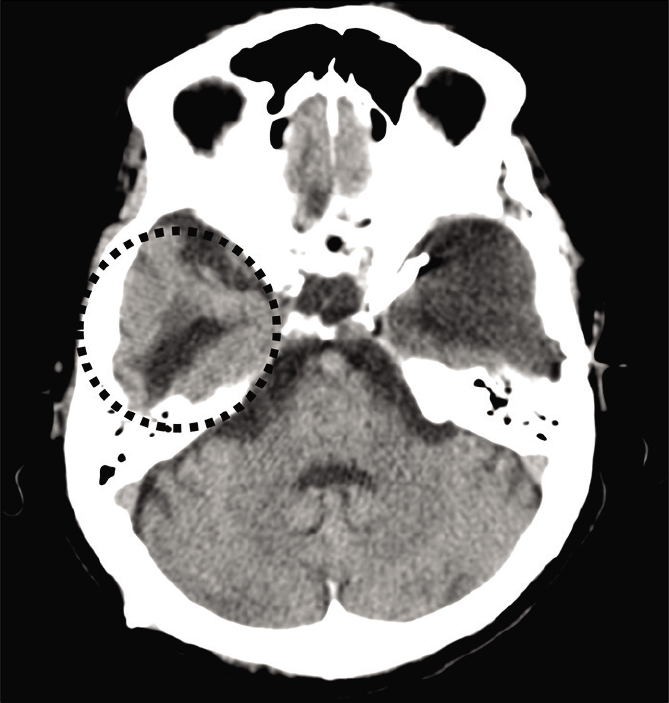
An 84-year-old woman presented to our hospital complaining of the right-sided clear otorrhea. The patient had a history of a VP shunt placement for hydrocephalus after a clip ligation for a left internal carotid-posterior communicating artery aneurysmal SAH 7 years before presentation. At 6 years before presentation, she had undergone ligation of the shunt catheter after complaining of the right-sided tinnitus with evidence of intraventricular pneumocephalus [
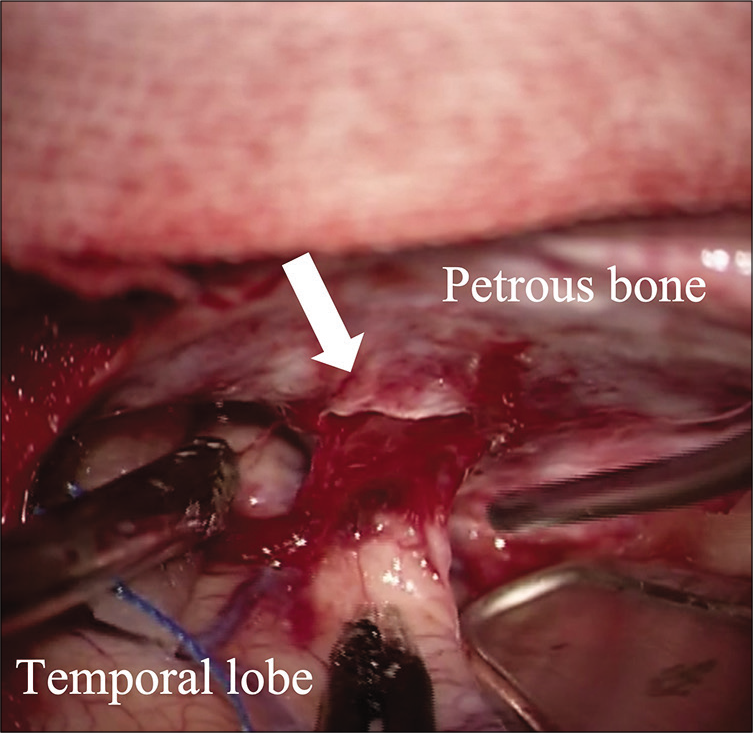
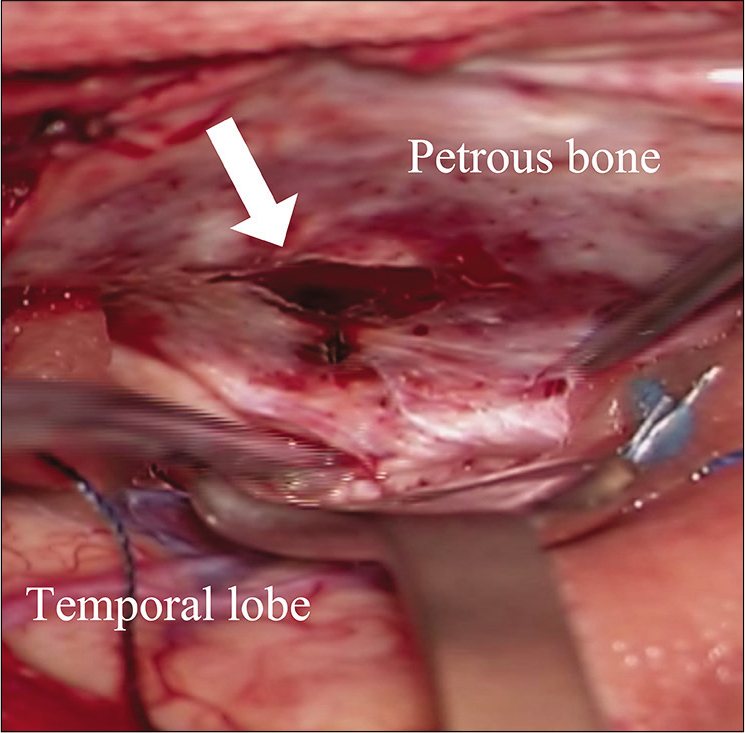
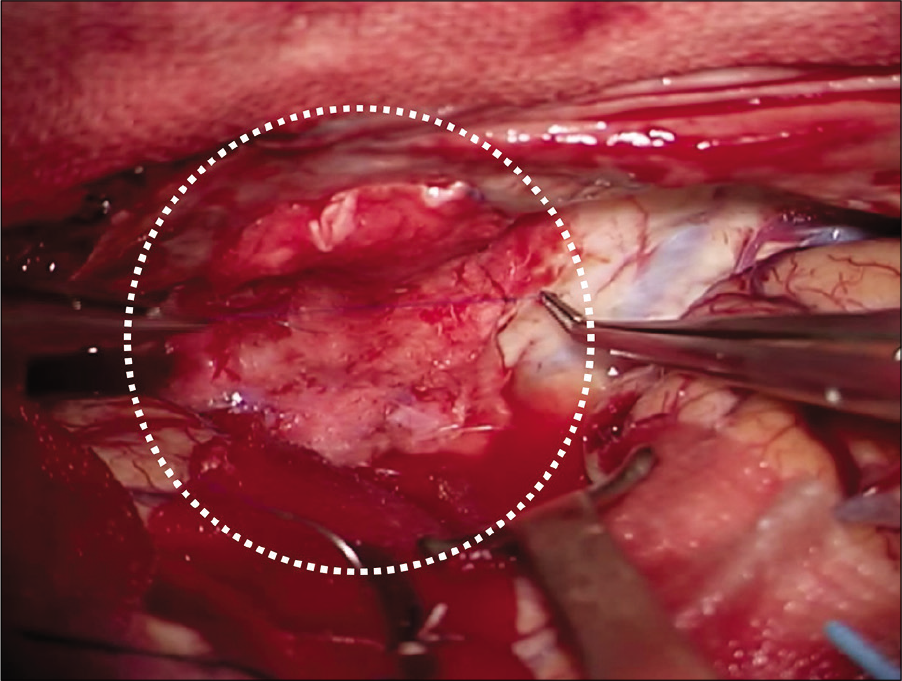
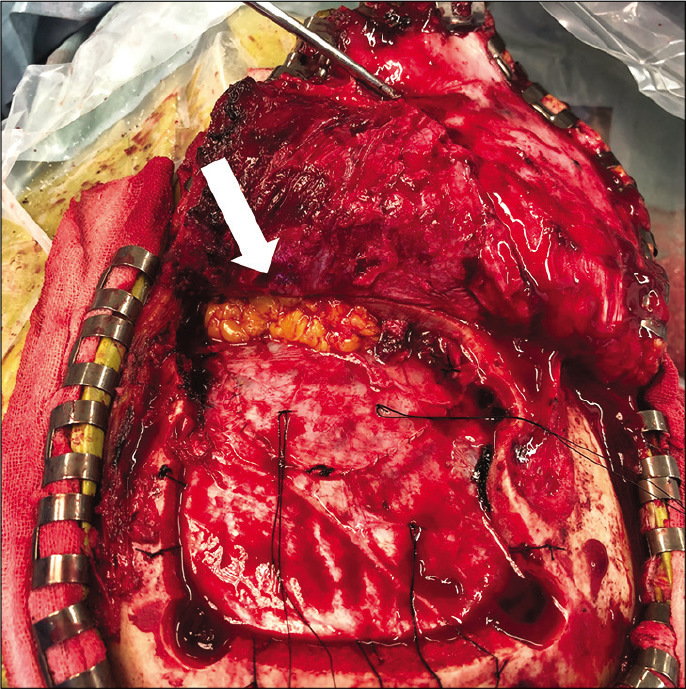
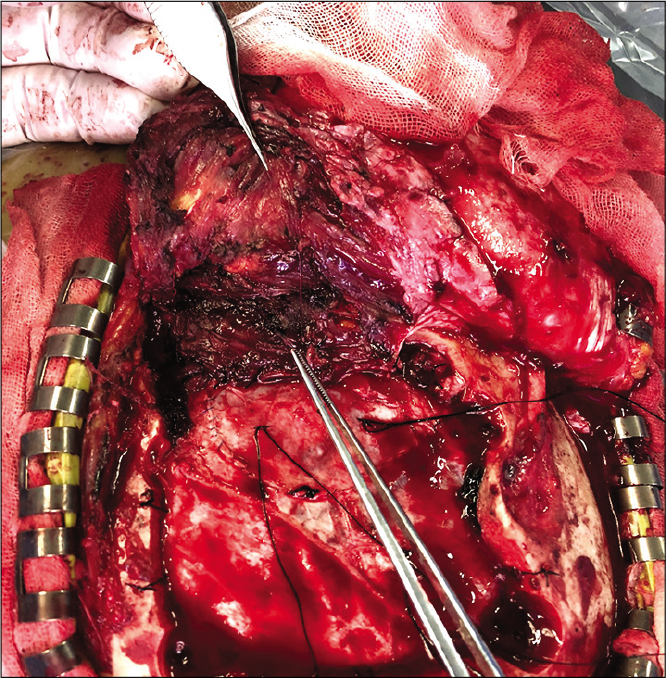
Three days after admission, we performed a right temporal craniotomy for a CSF leak repair. A lumbar drain was placed preoperatively. When the right temporal lobe was retracted, we identified the site of the leak, and it was noted that temporal lobe parenchyma herniated into the mastoid air cells through lacerated dura and a partially defective tegmen mastoideum [
DISCUSSION
CSF leaks result from abnormal communication between the subarachnoid space and the adjacent paranasal sinuses through osteodural defects. The etiologies of CSF leaks are commonly classified as either congenital or acquired.
Acquired CSF leaks can be further subdivided into traumatic, nontraumatic, and spontaneous subtypes.[
Although increased CSF leaks are thought to occur spontaneously, certain factors may predispose patients to this type of leak. It has been demonstrated that aberrant arachnoid granulations (AGs) that are surrounded by thin bony surfaces, including the cribriform plate, tegmen mastoideum, or sella turnica, can penetrate the adjacent bone to form fistulas.[
In this case, we consider that subclinical osteodural defect has been existed in the MCF, and there was an aberrant AG, which presented as a parenchymal herniation adjacent to the defect [
During repairs of temporal CSF leaks, either the MCF approach or the transmastoid approach are typically employed. The MCF approach, which facilitates extensive exposure of the MCF, a multilayer repair, and preservation of hearing, is preferred by many neurosurgeons and was adopted in this case. The transmastoid approach, which is an otological procedure, is less invasive and easier to be performed; however, the entire floor of the MCF can be difficult to visualize.[
CONCLUSION
In this patient, we successfully repaired a temporal bone CSF leak due to an aberrant AG by performing a temporal craniotomy. It is imperative for neurosurgeons to be aware of the mechanism by which sCSF leaks can be caused by aberrant AGs, and the surgical options for repairs of temporal bone CSF leaks.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Alonso RC, de la Peña MJ, Caicoya AG, Rodriguez MR, Moreno EA, de Vega Fernandez VM. Spontaneous skull base meningoencephaloceles and cerebrospinal fluid fistulas. Radiographics. 2013. 33: 553-70
2. Eljazzar R, Loewenstern J, Dai JB, Shrivastava RK, Iloreta AM Jr. Detection of cerebrospinal fluid leaks: Is there a radiologic standard of care? A systematic review. World Neurosurg. 2019. 127: 307-315
3. Gacek RR, Gacek MR, Tart R. Adult spontaneous cerebrospinal fluid otorrhea: Diagnosis and management. Am J Otol. 1999. 20: 770-776
4. Gacek RR. Arachnoid granulation cerebrospinal fluid otorrhea. Ann Otol Rhinol Laryngol. 1990. 99: 854-862
5. Gacek RR. Evaluation and management of temporal bone arachnoid granulations. Arch Otolaryngol Head Neck Surg. 1992. 118: 327-332
6. Kutz JW, Husain IA, Isaacson B, Roland PS. Management of spontaneous cerebrospinal fluid otorrhea. Laryngoscope. 2008. 118: 2195-9
7. Lobo BC, Baumanis MM, Nelson RF. Surgical repair of spontaneous cerebrospinal cerebrospinal fluid (CSF) leaks: A systematic review. Laryngoscope Investig Otolaryngol. 2017. 2: 215-224
8. Perez E, Carlton D, Alfarano M, Smouha E. Transmastoid repair of spontaneous cerebrospinal fluid leaks. J Neurol Surg B Skull Base. 2018. 79: 451-457