- Department of Neurosurgery, UPMC, Pittsburgh, Pennsylvania, United States.
- Department of Neurosurgery, Allegheny General Hospital, Pittsburgh, Pennsylvania, United States.
Correspondence Address:
Joseph Scott Hudson, Department of Neurosurgery, UPMC, Pittsburgh, Pennsylvania, United States.
DOI:10.25259/SNI_414_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Joseph Scott Hudson1, Seung Jeong2, Xiaoran Zhang1, Taylor J. Abel1. Spontaneous epidural pneumorrhachis in 14 years old. 06-Jul-2021;12:329
How to cite this URL: Joseph Scott Hudson1, Seung Jeong2, Xiaoran Zhang1, Taylor J. Abel1. Spontaneous epidural pneumorrhachis in 14 years old. 06-Jul-2021;12:329. Available from: https://surgicalneurologyint.com/surgicalint-articles/10949/
Abstract
Background: Pneumorrhachis is an exceedingly rare complication of pneumomediastinum as air tracks through tissue planes into the epidural (or subdural space). The majority of these patients present with a clear history of trauma, iatrogenic injury, pneumothorax, vomiting, or retching.
Case Description: A 14-year-old male presented with the asymptomatic spontaneous onset of pneumorrhachis associated with significant pneumomediastinum of unclear etiology.
Conclusion: Most patients with pneumorrhachis present with nonfocal neurological examinations. For these patients, it is critical to rule out infection as the cause of epidural gas. If other systemic signs are present, then urgent contrast-enhanced magnetic resonance imaging should be obtained. The majority of patients will demonstrate spontaneous radiographic resolution of pneumorrhachis within several days.
Keywords: Case report, Epidural, Pneumomediastinum, Pneumorrhachis, Pneumothorax
INTRODUCTION
Pneumorrhachis is defined as the presence of air/gas in the epidural or subdural space. There are a variety of potential etiologies including blunt trauma, infection with gas forming organisms, pneumothorax and pneumomediastinum, iatrogenic/post injection, inhalational injuries, and asthma exacerbation.[
Most instances of pneumorrhachis typically resolve radiographically within days (i.e., air resorbs directly into the blood stream). Rarely, it can be associated with pain and/or neurologic deficit.[
ILLUSTRATIVE CASE
A 14-year-old male presented with 2 weeks of mental status changes, chest pain, decreased oral intake, fatigue, and decreased urinary output. Laboratory data revealed prerenal azotemia and a chest X-ray demonstrated supraclavicular emphysema. On further questioning, he had previously experienced several episodes of coughing and choking while brushing his teeth.
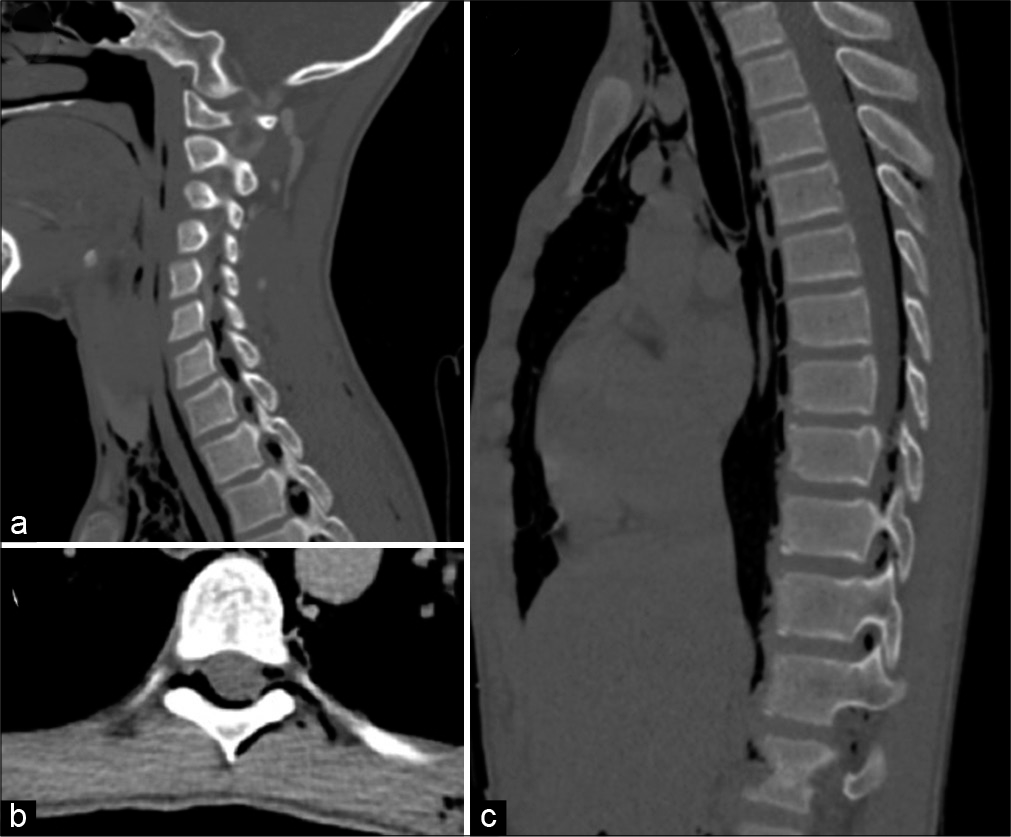
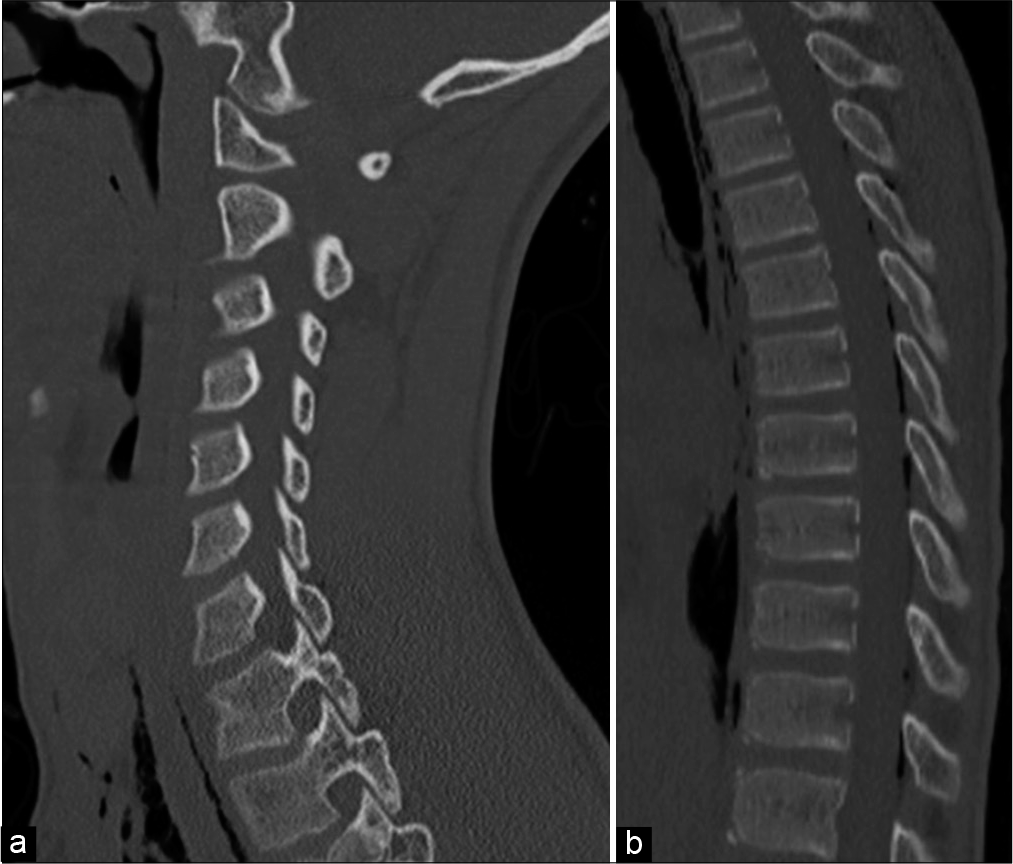
On physical examination, he was tall thin and cachectic (i.e., BMI of 11) but was neurologically intact. The CT scan of the neck and chest revealed a large pneumomediastinum, soft-tissue emphysema, and air in the retroperitoneum. Cervical, thoracic, and lumbar pneumorrhachis were also observed (i.e., both ventral and dorsal). Air was seen tracking through the neuroforamen bilaterally at multiple levels [
Figure 1:
Spontaneous pneumorrhachis in 14 years old with extensive mediastinum. (a) Sagittal CT view showing air tracking through the neuroforamina, (b) sagittal CT showing air throughout the dorsal epidural space in the thoracic spine, (c) axial CT of the thoracic spine showing air tracking through the dorsal epidural space out the bilateral neuroforamina.
DISCUSSION
Observations
It is extremely rare to observe, spontaneous pneumorrhachis involving the cervical or thoracic spine without an identifiable etiology. Typically, it is associated with trauma, iatrogenic injury, coughing/chest pain, or Boerhaave’s syndrome. The neurosurgical management of extensive epidural air in the neurologically asymptomatic patient involves observation with serial examination. If a patient develops symptoms, different management strategies may be warranted including steroids, percutaneous needle aspiration, and/or high fractions of inspired oxygen.[
CONCLUSION
Pneumorrhachis is an exceedingly rare complication of pneumomediastinum and occurs when air tracks through tissue planes into the epidural (or subdural space). Although it is critical to rule out infection gas and other causes of this problem, most cases are spontaneous in origin and will similarly, spontaneously regress as documented on serial imaging.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Oertel MF, Kornith MC, Reinges T, Krings T, Terbeck S, Gilsbach JM. Pathogenesis, diagnosis and management of pneumorrhachis. Eur Spine J. 2006. 15: 636-43