- Department of Neurosurgery, Kawasaki Medical School, Kurashiki,
- Department of Neurosurgery, Okayama Central Hospital, Okayama, Japan.
Correspondence Address:
Kenji Yagi
Department of Neurosurgery, Kawasaki Medical School, Kurashiki,
DOI:10.25259/SNI_212_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shodai Yamada1, Kenji Yagi1, Kazuhiro Hirano2, Masaaki Uno1. Spontaneous improvement of secondary empty sella syndrome due to re-expansion of an intrasellar cyst: A case report. 12-Sep-2020;11:282
How to cite this URL: Shodai Yamada1, Kenji Yagi1, Kazuhiro Hirano2, Masaaki Uno1. Spontaneous improvement of secondary empty sella syndrome due to re-expansion of an intrasellar cyst: A case report. 12-Sep-2020;11:282. Available from: https://surgicalneurologyint.com/surgicalint-articles/10258/
Abstract
Background: In patients with secondary empty sella syndrome (ESS), optic nerve herniation into the sella turcica is caused by shrinkage of the mass lesion at the sella turcica, resulting in visual disturbance. ESS is often surgically treated using chiasmapexy. Here, we report the first case of spontaneous improvement in a patient with ESS.
Case Description: A 69-year-old woman presented with a month-long history of visual disturbance in the right eye, poor visual acuity, and quadrantanopia in her upper temporal visual field. Magnetic resonance (MR) imaging showed herniation of her right optic nerve and gyrus rectus into the sella turcica. The visual disturbance gradually improved, and the patient’s vision became almost normal after a month without any treatment. On repeated MR imaging, it was observed that the herniation of the right optic nerve and gyrus rectus disappeared due to an intrasellar cyst re-expansion. The secondary ESS caused by the shrinkage of the intrasellar cyst resulted in the visual disturbance and re-expansion of the cyst resulted in spontaneous improvement of symptoms. The visual disturbance did not recur for a year.
Conclusion: Patients with secondary ESS without severe symptoms may be followed up conservatively. However, surgical treatment should be applied if symptoms deteriorate or do not improve.
Keywords: Chiasmapexy, Rathke’s cleft cyst, Secondary empty sella syndrome, Visual disturbance
INTRODUCTION
Empty sella syndrome (ESS) has been reported to occur in 5.5% of patients with pituitary disease.[
Patients with secondary ESS could theoretically recover if the intrasellar lesion re-expands and the herniated optic nerve returns to its original position. However, such a case has never been reported in the literature. Rather, patients with secondary ESS have been surgically treated by chiasmapexy to relocate and fix the herniated optic nerve at the suprasellar and its normal site.[
CASE DESCRIPTION
A 69-year-old woman presented with a month-long history of poor eye sight in her right eye. She had hypertension and diabetes mellitus and had previously undergone surgeries to remove cancers in her breast 9 years ago and in her lung 2 years ago. Her recovery from these past surgeries was uneventful with no recurrence.
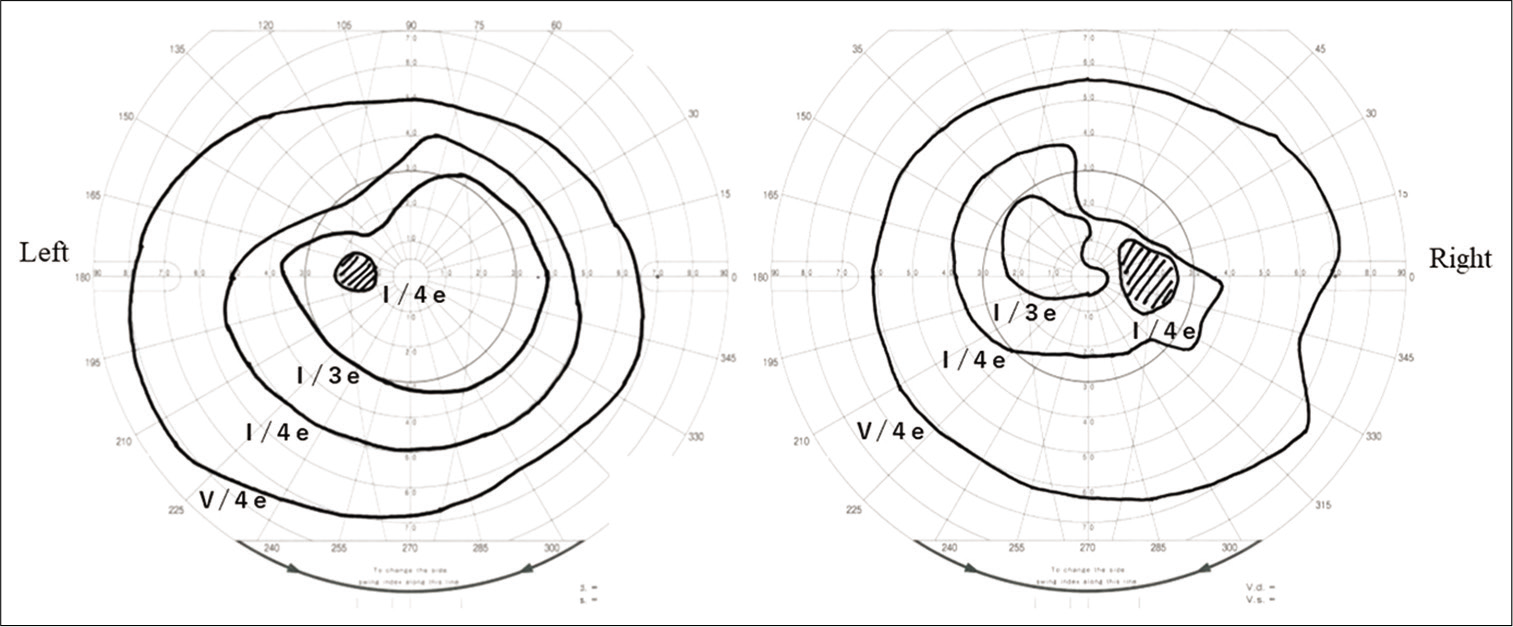
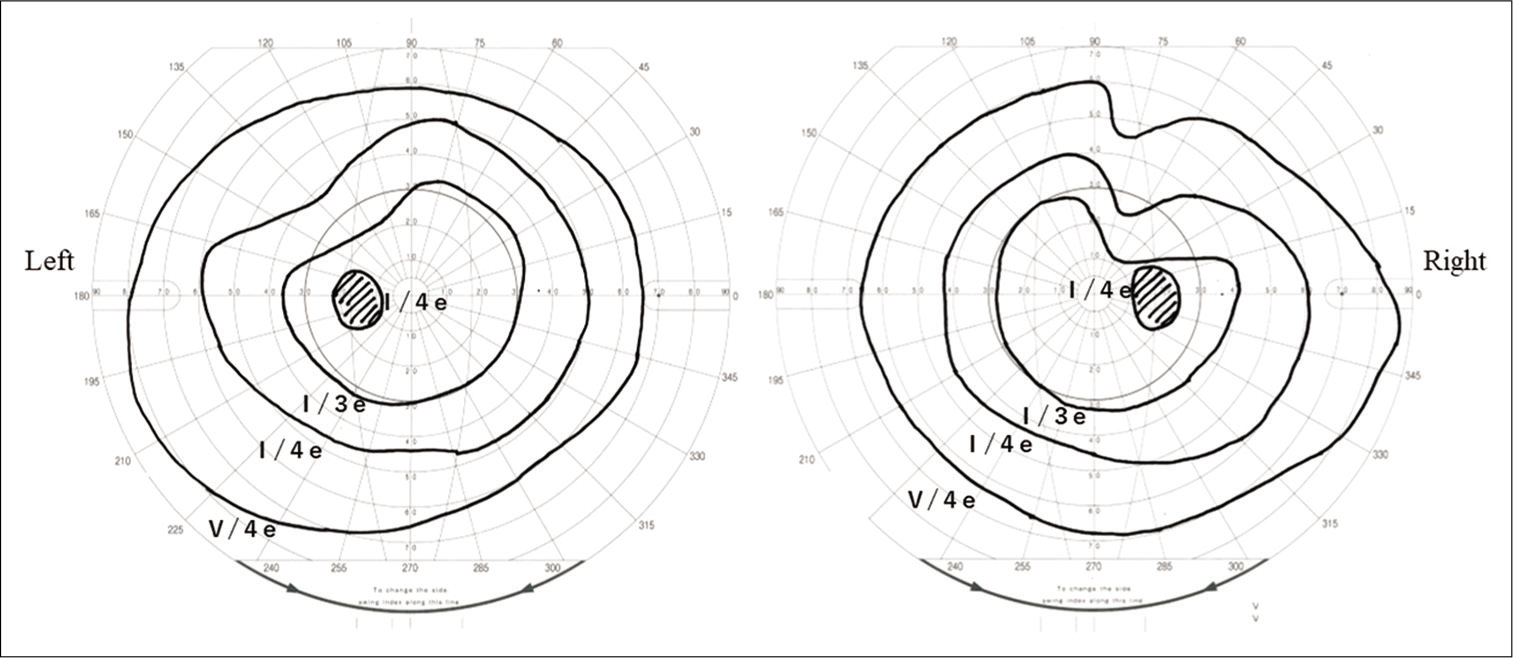
Her right eye vision was remarkably disturbed, while her left eye vision was not remarkably impaired. Corrected visual acuity in the right eye was 20/100, which was 20/25 previously. In a visual field test by Goldmann perimetry, a remarkable upper temporal visual field defect and slight defect were observed in the right and left eye, respectively [
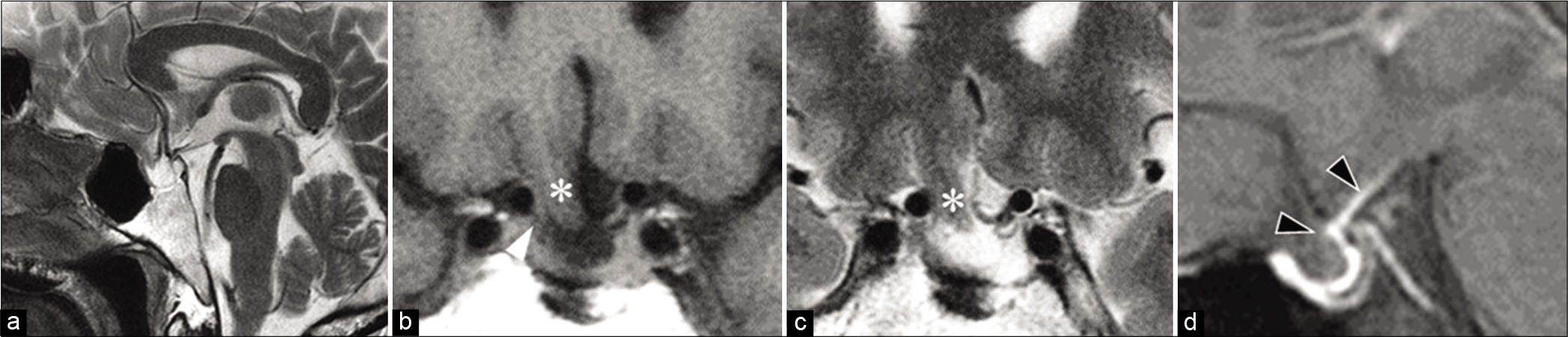
Figure 2:
Magnetic resonance (MR) imaging at presentation. On sagittal of T2-weighted image (a) and coronal sections of (b) T1- and (c) T2-weighted images, herniation of the gyrus rectus (*) and right optic nerves (white arrow head) is shown. The sagittal section of contrasted fat-saturated T1-weighted MR image (d) shows an enhancement at the diaphragm (black arrow head).
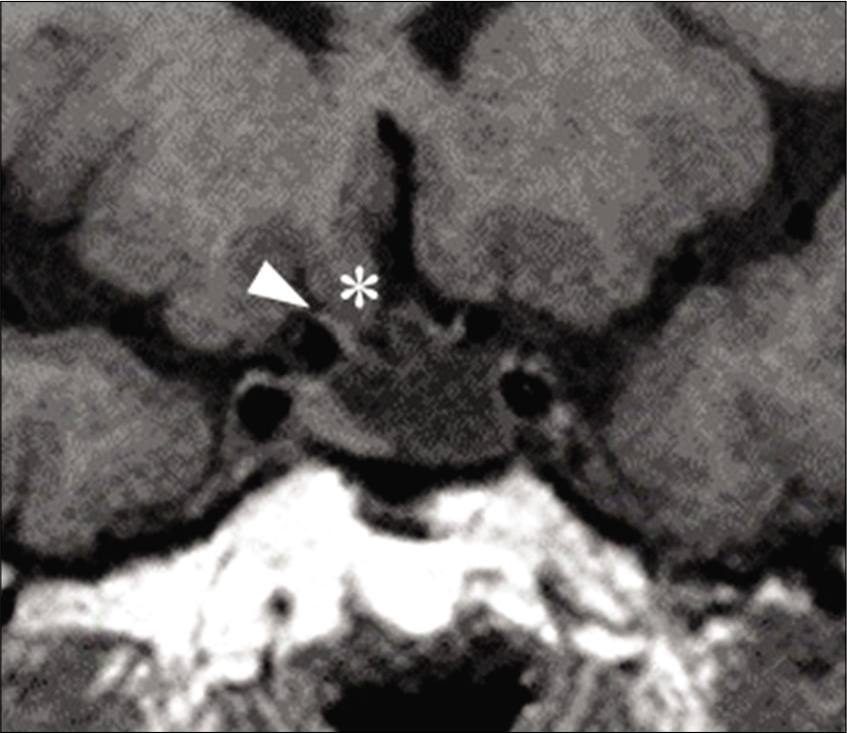
Figure 5:
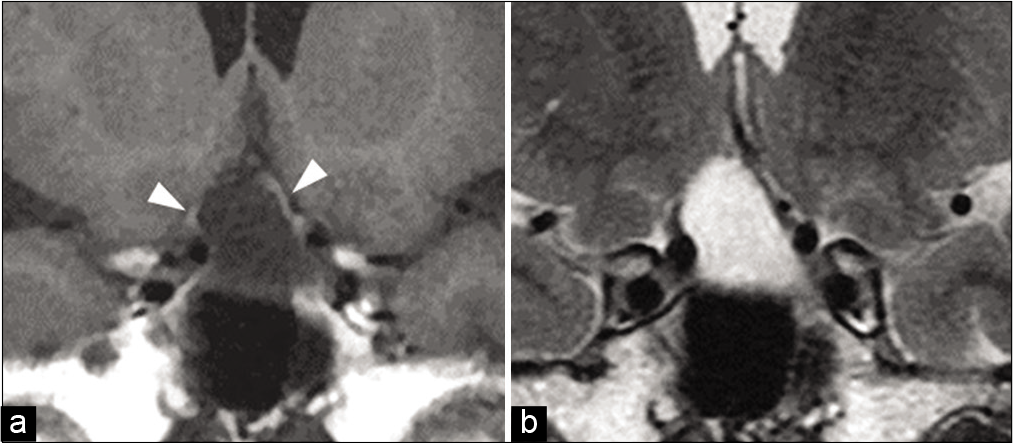
Coronal sections of repeated (a) T1- and (b) T2-weighted magnetic resonance images at 3 months post presentation. The bilateral optic nerves were cranially dislocated, resulting in remarkable expansion of the intrasellar cyst (arrow head). The contents of the cyst had a signal similar to signals of cerebrospinal fluid.
DISCUSSION
In our patient with secondary ESS, visual disturbance improved due to spontaneous expansion of the intrasellar cyst under a conservative follow-up. To the best of our knowledge, this is the first reported case of spontaneous improvement in a patient with ESS.
Secondary ESS is caused by downward herniation of the diaphragm adhered to the optic nerve.[
Surgeries have been performed for secondary ESS and various methods of chiasmapexy, to relocate and fix the herniated suprasellar tissue, including the optic nerve.[
CONCLUSION
A patient without a severe symptom may be followed up conservatively. However, surgical treatment should be applied if the symptoms deteriorate or do not improve.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from the individual participant included in the study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Barzaghi LR, Donofrio CA, Panni P, Losa M, Mortini P. Treatment of empty sella associated with visual impairment: A systematic review of chiasmapexy techniques. Pituitary. 2018. 21: 98-106
2. Busch W. Morphology of sella turcica and its relation to the pituitary gland. Virchows Arch Pathol Anat Physiol Klin Med. 1951. 320: 437-58
3. Fischer EG, DeGirolami U, Suojanen JN. Reversible visual deficit following debulking of a Rathke’s cleft cyst: A tethered chiasm?. J Neurosurg. 1994. 81: 459-62
4. Kaufman B, Tomsak RL, Kaufman BA, Arafah BU, Bellon EM, Selman WR. Herniation of the suprasellar visual system and third ventricle into empty sellae: Morphologic and clinical considerations. AJR Am J Roentgenol. 1989. 152: 597-608
5. Kubo S, Hasegawa H, Inui T, Tominaga S, Yoshimine T. Endonasal endoscopic transsphenoidal chiasmapexy with silicone plates for empty sella syndrome: Technical note. Neurol Med Chir (Tokyo). 2005. 45: 428-32
6. Olson DR, Guiot G, Derome P. The symptomatic empty sella. Prevention and correction via the transsphenoidal approach. J Neurosurg. 1972. 37: 533-7
7. Taniguchi H, Muguruma K, Hiura Y, Inoue T, Kawa G, Kinoshita H. Acquired male hypogonadotropic hypogonadism (MHH) in a patient with empty sella: A case report. Hinyokika Kiyo. 2008. 54: 791-3