- Department of Neurosurgery, NIMHANS, Bengaluru, Karnataka, India
Correspondence Address:
Amey R. Savardekar
Department of Neurosurgery, NIMHANS, Bengaluru, Karnataka, India
DOI:10.4103/2152-7806.195231
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Amey R. Savardekar, Rajesh Krishna, A. Arivazhagan. Spontaneous intraventricular rupture of pyogenic brain abscess: A short series of three cases and review of literature. 05-Dec-2016;7:
How to cite this URL: Amey R. Savardekar, Rajesh Krishna, A. Arivazhagan. Spontaneous intraventricular rupture of pyogenic brain abscess: A short series of three cases and review of literature. 05-Dec-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/spontaneous-intraventricular-rupture-of-pyogenic-brain-abscess-a-short-series-of-three-cases-and-review-of-literature/
Abstract
Background:Spontaneous intraventricular rupture of brain abscess (IVROBA) is a dreaded complication of pyogenic brain abscess (PBA) and is associated with very high mortality. We discuss the clinical, radiological, and therapeutic aspects associated with this potentially fatal complication of PBAs.
Case Descriptions:Three cases of spontaneous IVROBA presenting to our institute over a period of 6 months were reviewed with respect to their clinical and radiological presentation, their therapeutic plan, and neurological outcome. Individualized approach to our patients with IVROBA with abscess drainage/excision, intrathecal and intravenous antibiotic therapy, cerebrospinal fluid (CSF) diversion (if under high pressure), and close monitoring of clinical status, CSF reports, and computed tomography (CT) scan findings enabled us to achieve good neurological outcome in two patients presenting in conscious state; however, one patient presenting in poor neurological status succumbed to IVROBA due to fulminant septic arteritis.
Conclusion:In the present neurosurgical era, IVROBA is rarely encountered; however when it occurs, patient outcome is adversely affected. Early detection and prompt aggressive management, as seen in our short series, can give the patient a fighting chance and significantly improve the neurological outcome.
Keywords: Intraventricular rupture, outcome, pyogenic brain abscess, review of literature, ventriculitis
INTRODUCTION
Intraventricular rupture of brain abscess (IVROBA) is a potentially fatal complication of pyogenic brain abscess (PBA). Mortality rates after IVROBA have been reported to range between 39% and 80%.[
Individualized approach to patients with IVROBA with abscess drainage/excision, intrathecal and intravenous antibiotic therapy, cerebrospinal fluid (CSF) diversion (if under high pressure) and close monitoring of clinical status, CSF reports and computed tomography (CT) scan findings, helped us achieve good neurological outcome in two patients presenting in conscious state; whereas one patient presenting in poor neurological status (comatose) succumbed to IVROBA due to fulminant septic arteritis.
CASE REPORTS
Case 1
A 40-year-old gentleman presented with a history of intermittent high-grade fever and headache of 15 days’ duration. On clinical examination, he was conscious, alert, and neurologically intact, and investigations revealed that he was immune-competent. Total leucocyte count (TLC) was 14500/mm3. CT of the brain showed a ring-enhancing lesion in the right frontal region suggestive of brain abscess, which was communicating medially with the frontal horn of the right lateral ventricle. The “tell-tale” signs of IVROBA were ependymal enhancement seen in the right frontal horn [
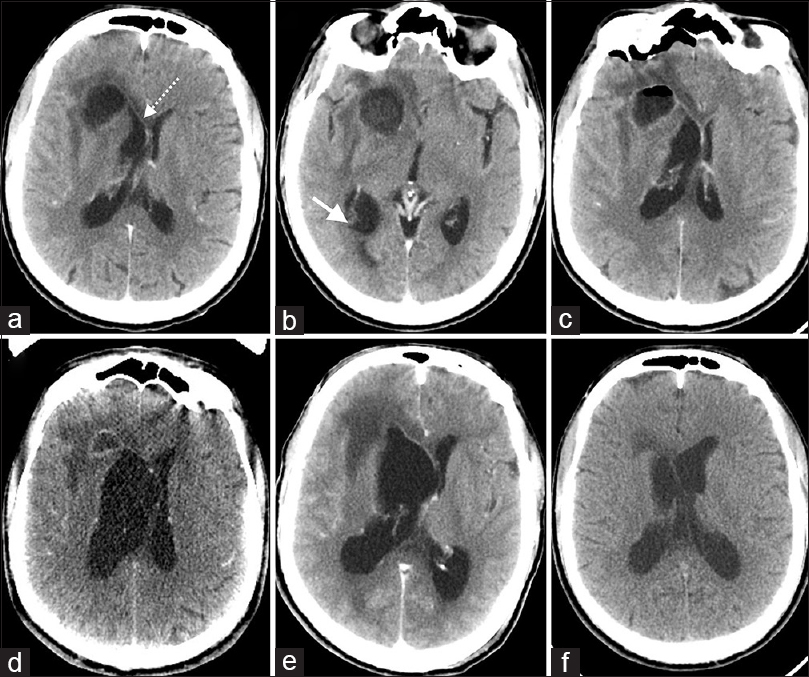
Figure 1
Case 1 – (a) and (b) Preoperative contrast-enhanced computed tomography (CECT) scan of the brain showing a right frontal abscess in close proximity to the frontal horn of the right lateral ventricle. The dotted line with closed arrow depicts the ependymal enhancement. The full line with closed arrow shows the “pus-fluid” level demonstrating debris in the dependent occipital horn. (c) Post-tapping CT showing air within the abscess cavity. (d and e) CECT scan during treatment showing the well-developed abscess wall communicating with the loculated right lateral ventricle. (f) Follow-up CECT shows resolution of the abscess and the ventriculitis
He was started on empirical intravenous antibiotics in appropriate meningitic doses after taking blood sample for culture. He underwent right frontal burr hole and tapping of the abscess; 30 ml of pus mixed CSF was aspirated. Gram stain showed gram positive cocci in clusters, however, pus culture yielded no growth. Treatment was continued with intravenous antibiotics (ceftriaxone, amikacin, and metronidazole); however, the gradually deteriorated in sensorium. Right frontal external ventricular drain (EVD) was placed and intraventricular colistin (dosage = 1 million units in 1:10 dilution) was administered twice daily for 7 days till the patient improved clinically and CSF parameters normalized. CSF cultures were sent daily but no organism was isolated. Simultaneously, intravenous colistin (dosage = 10 million units) twice a day was administered. After removal of the EVD, patient was continued on intravenous colistin for another 3 weeks till CT brain showed resolution of ependymal enhancement. Patient was discharged in fully functional status. Follow up imaging done at 3-months post discharge showed complete resolution of abscess and absence of ependymal enhancement [
Case 2
A 21-year-old gentleman, a known case of right chronic suppurative otitis media (CSOM), presented with history of headache, vomiting, and intermittent high-grade fever of 2-month duration. On presentation, he was conscious, alert with no focal neurological deficits and was immune-competent; TLC was 15100/mm3. CT brain showed a right posterior temporal abscess situated close to the temporal horn of the right lateral ventricle. The presence of ependymal enhancement of the right temporal horn [
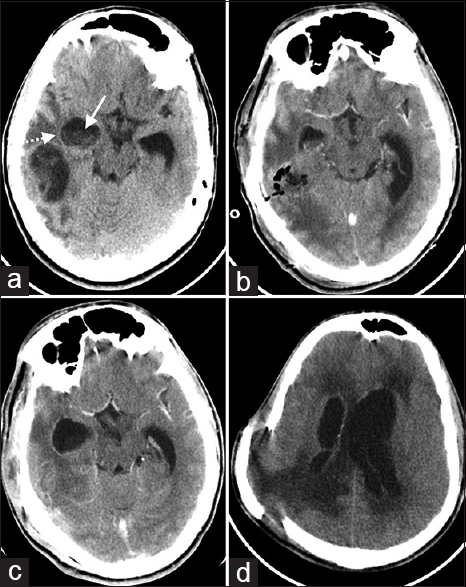
Figure 2
(a) Preoperative contrast-enhanced computed tomography (CECT) scan of Case 2 shows a superficially located brain abscess in the right temporal lobe; abscess shows well-formed lateral wall and ill-formed medial wall, with the temporal horn of the lateral ventricle showing ependymal enhancement (dotted line with closed arrow head) and presence of debris (full line with closed arrow). (b) Post-operative CECT scan shows excision of the abscess. (c) CECT during treatment showing loculated right temporal horn. (d) Follow-up CT scan at 3 weeks after stopping antibiotics showing loculated ventricles with hydrocephalus, elevated bone flap, and raised intracranial pressure
The patient was started on empirical intravenous antibiotics (ceftriaxone, amikacin, and metronidazole) in meningitic doses after collecting blood sample for culture sensitivity. He underwent right temporoparietal craniotomy and excision of the abscess. Intraoperatively, the abscess wall was seen to be communicating with the right temporal horn anteromedially; thorough “saline wash” was given in the cavity and inside the ventricle.
Right frontal EVD was placed. CSF was turbid with total cell count of 5000 cells/hpf (95% polymorphocytes); glucose was 2 mg/dl and protein was 575 mg/dl. Pus cultures from the brain abscess as well as pus from the ear (ear swab) yielded Streptococcus spp. as the offending organism. CSF culture yielded Enterococcus avium. EVD was kept for 2 weeks and the patient received intraventricular as well as intravenous antibiotics as per the culture sensitivity report (vancomycin and ciprofloxacin). Once the patient was afebrile, neurologically stable, and three consecutive CSF cultures were negative, the EVD was removed and intravenous vancomycin and ciprofloxacin (in meningitic doses) was continued for another 6 weeks at a local hospital.
Three weeks after stopping antibiotics, the patient presented to the casualty in altered sensorium. Fundus showed papilledema. CT scan of brain showed intraventricular septations with dilatation of contralateral lateral ventricle and third ventricle with cerebral edema. Bone flap at the operative site was raised suggestive of raised intracranial pressure (ICP) [
Case 3
A middle-aged male patient was brought to our casualty by the police after being found lying unconscious on the road; no further details were available. On clinical examination, his Glasgow coma score (GCS) was E1 M4 V1, vital signs were stable, and pupils were equal and reacting to light. There was profuse pus discharge from the right ear; TLC was 28900/mm3. He was evaluated with CT head which showed a left posterior temporal abscess, with rupture into the temporal horn of the left lateral ventricle [Figure
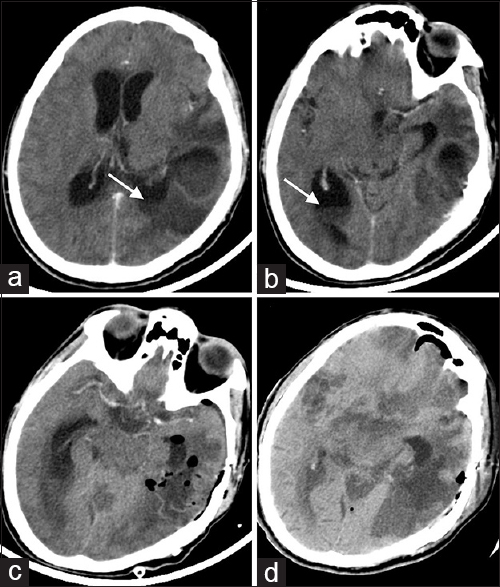
Figure 3
(a and b) Preoperative CECT scan of Case 3 shows a superficially located brain abscess in the left temporal lobe with clear-cut evidence of intraventricular rupture of brain abscess and debris in the dependent occipital horns (full line with closed arrow head). (c) Post-operative contrast-enhanced computed tomography (CECT) scan shows excision of the abscess and postlavage status of the ventricles. (d) CT scan done at 3 days after surgery reveals widespread patchy cerebral infarction secondary to septic arteritis
He underwent emergency twist drill craniostomy and tapping of the abscess, followed by left temporoparietal craniotomy and excision of the abscess. Postoperatively, the patient continued to be in poor neurological status and was admitted in the intensive care unit for ventilatory support. He was treated with empirical intravenous and intrathecal antibiotics (ceftriaxone, amikacin, and metronidazole) in meningitic dosages; however, his sensorium gradually deteriorated over the next 3 days to GCS of E1M1V1. The pus culture revealed Streptoccus pyogenes to be the offending organism, and appropriate antibiotic therapy was instituted. Histopathology revealed an organizing abscess in the left temporal lobe. CT brain (3 days after the surgery) showed multiple cerebral infarctions suggestive of septic arteritis [
DISCUSSION
IVROBA is a catastrophic complication of pyogenic brain abscess. The reported incidence of IVROBA ranges from 1% to 31%.[
In one of the very few studies dealing with the predictive factors associated with IVROBA, Takeshita et al. concluded that signs of meningeal irritation and localized enhancement of the ventricular wall adjacent to the abscess (observed on imaging studies) are events preceding the intraventricular rupture of a PBA.[
Mortality rate of IVROBA was reported to be up to 80% in many earlier series, however, with the advent of better diagnostic imaging and aggressive antibiotic therapy, it has come down to below 40%.[
In patients who tide over the acute crisis, intraventricular septations resulting in isolated ventricular dilatation is a late complication.[
Literature review, as well as our short case series, suggests that early identification of IVROBA is very important in determining the final outcome.[
Once diagnosis has been established, it is imperative to start simultaneous intrathecal and intravenous antibiotics, initially empirical, followed by appropriate ones recommended as per the culture sensitivity of the pus/CSF.[
The recurring point of contention noted in the sparse literature pertaining to IVROBA has been the lack of guidelines for managing these patients.[
Our short series of three cases does not itself lend any significant weight to the treatment guidelines for IVROBA; however, it does substantiate the present stance in the review of literature that the nihilistic attitude towards IVROBA needs to be re-considered. Early diagnosis and aggressive treatment can result in full neurological recovery of patients presenting with IVROBA (as seen in Cases 1 and 2). Patients presenting in later stages with IVROBA and fulminant meningoencephalitis still continue to have grave prognosis (as seen in Case 3).
CONCLUSION
Presently, the ubiquitous imaging for neurological disorders and the advances in neurosurgical techniques and antibacterial therapy appear to have resulted in early diagnosis of PBAs and their successful management. As such, IVROBA may be rarely encountered. However, when it occurs, the patient's prognosis is adversely affected. In spite of current advances in diagnosis and treatment, IVROBA remains a dreaded complication of PBA. Early detection and prompt aggressive management in the form of abscess drainage/excision followed by intrathecal and intravenous antibiotic therapy (as per sensitivity) can give the patient a fighting chance and significantly improve the outcome.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Britt RH, Enzmann DR. Neuropathological and computerized tomographic findings in experimental brain abscess. J Neurosurg. 1981. 55: 590-603
2. Isono M, Wakabayashi Y, Nakano T, Fujiki M, Mori T, Hori S. Treatment of brain abscess associated with ventricular rupture--three case reports. Neurol Med Chir. 1997. 37: 630-6
3. Lee TH, Chang WN, Su TM, Chang HW, Lui CC, Ho JT. Clinical features and predictive factors of intraventricular rupture in patients who have bacterial brain abscesses. J Neurol Neurosurg Psychiatry. 2007. 78: 303-9
4. Nishizaki T, Ikeda N, Nakano S, Sakakura T, Abiko M, Okamura T. Successful neuroendoscopic treatment of intraventricular brain abscess rupture. Clin Pract. 2011. 1: e52-
5. Schultz P, Leeds NE. Intraventricular septations complicating neonatal meningitis. J Neurosurg. 1973. 38: 620-6
6. Takeshita M, Kagawa M, Izawa M TK. Current treatment strategies and factors influencing outcome in patients with bacterial brain abscess. Acta Neurochir. 1998. 140: 1263-70
7. Takeshita M, Kawamata T, Izawa M HT. Prodromal signs and clinical factors influencing outcome in patients with intraventricular rupture of purulent brain abscess. Neurosurgery. 2001. 48: 310-7
8. Wood JH, Doppman JL, Lightfoote WE, Girton M OA. Role of vascular proliferation on angiographic appearance and encapsulation of experimental traumatic and metastatic brain abscesses. J Neurosurg. 1978. 48: 264-73
9. Zeidman SM, Geisler FH OA. Intra-ventricular rupture of a purulent brain abscess: Case report. Neurosurgery. 1995. 36: 189-93