- Departments of Neurosurgery, Federal Fluminense University, Rio de Janeiro, Brazil.
- Departments of Neurology, Federal Fluminense University, Rio de Janeiro, Brazil.
Correspondence Address:
Messias Gonçalves Pacheco Junior
Departments of Neurology, Federal Fluminense University, Rio de Janeiro, Brazil.
DOI:10.25259/SNI_58_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Messias Gonçalves Pacheco Junior, Bruno Lima Pessoa, Jose Alberto Landeiro, Pedro Henrique de Abreu Macedo, Marco Antônio Araújo Leite. Spontaneous resolution of chronic subdural hematoma: Does only the size matter?. 04-Oct-2019;10:194
How to cite this URL: Messias Gonçalves Pacheco Junior, Bruno Lima Pessoa, Jose Alberto Landeiro, Pedro Henrique de Abreu Macedo, Marco Antônio Araújo Leite. Spontaneous resolution of chronic subdural hematoma: Does only the size matter?. 04-Oct-2019;10:194. Available from: http://surgicalneurologyint.com/surgicalint-articles/9683/
Abstract
Background: Chronic subdural hematomas (CSDHs) usually occur late in adults and older after mild head trauma. Surgical intervention is the first treatment option in CSDH with conservative management being adopted in few cases.
Case Description: We report a case of a 71-year-old man who presented a spontaneous resolution of a large CSDH. He presented with a difficulty of speech and an ataxic gait. Head (computed tomography scan) showed a low-density lesion located in the right frontal-temporal-parietal region.
Conclusion: In this report, we discuss the spontaneous resolution of a large CSDH in elderly patients, without surgical intervention. Gradually, several successful nonsurgical therapies for the treatment of these hematomas are reported, although further studies are essential to establish the role of these nonsurgical treatments of CSDHs.
Keywords: Chronic subdural hematoma, Nonsurgical treatment, Spontaneous resolution
INTRODUCTION
Chronic subdural hematoma (CSDH) is a common condition in neurosurgery, occurring more commonly in the elderly.[
CSDHs are more frequent in elderly patients, where cerebral compliance is higher than in young patients. This higher compliance may lead to a great variety of clinical presentations, with diagnostic and therapeutic difficulties being imposed.[
Its incidence is estimated at 1.72/100,000/year in the general population and 7.35/100,000/year in the 70–79 age groups. Given the progressive aging of the population, there is a tendency to increase its prevalence.[
Surgical treatment is the conduct of choice in the majority of cases, allowing immediate brain decompression and significant improvement of symptoms. However, the nonsurgical treatment is admitted in exceptional situations such as asymptomatic cases, small CSDH, and patients with very advanced age or with clinical conditions that contraindicate the surgery itself.[
Besides, the spontaneous resolution of CSDHs may occur in some cases without surgical intervention. However, there are few studies in literature concerning the spontaneous resolution of CSDHs, with an extremely different incidence, ranging from <1% to 20% of cases.[
The reasons for the spontaneous resolution of CSDHs are unclear. Herein, we report a patient with spontaneous resolution of a large CSDH, discussing the possible causes and consequences of such spontaneous resolution and nonsurgical approach.
We retrospectively analyzed the patient’s records, including images throughout Picture Archiving and Communication System – Phillips database, as well as information collected in outpatient return visits. For the review of literature, we used as a database: PubMed, LILACS, and SciELO. The search was based on the following keywords: CSDH, spontaneous resolution, and nonsurgical treatment.
CASE REPORT
A 71-year-old male presented to the neurology outpatient clinic of Hospital Universitário Antônio Pedro (HUAP) to monitor and optimize therapy for Parkinson’s disease. At 2014, he mentioned in his first consult a sudden onset of dysarthria and gait ataxia and underwent imaging tests, although he had not returned to consult for 4 years after that, with no possibility of follow-up by the inicial physicians.
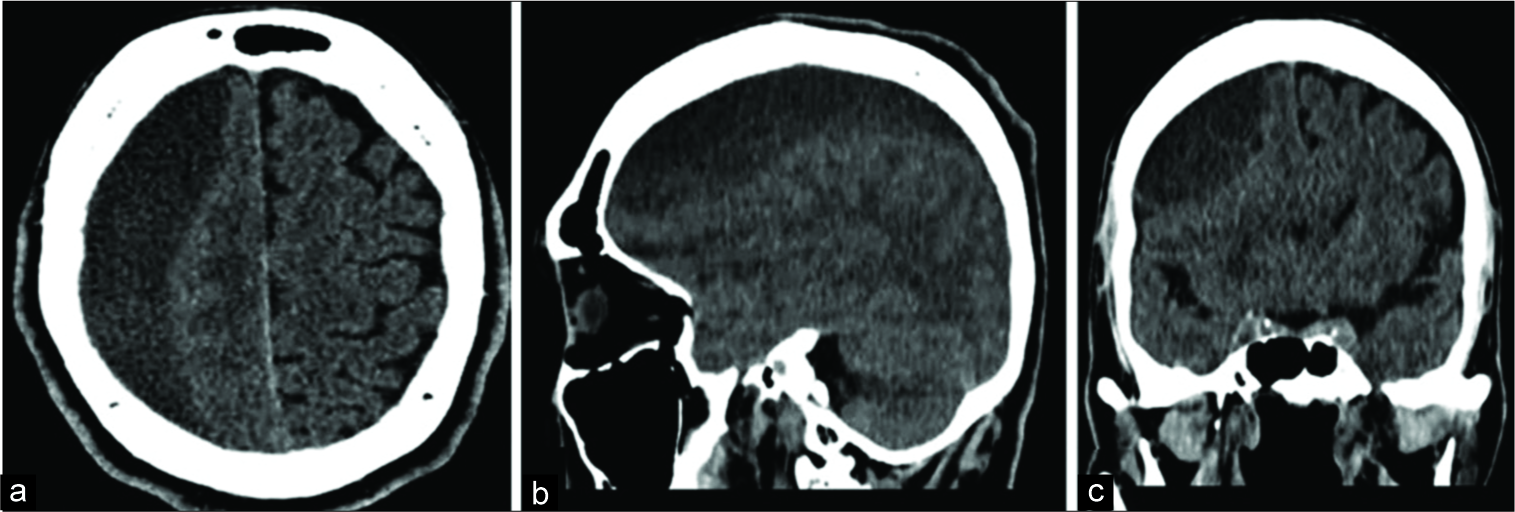
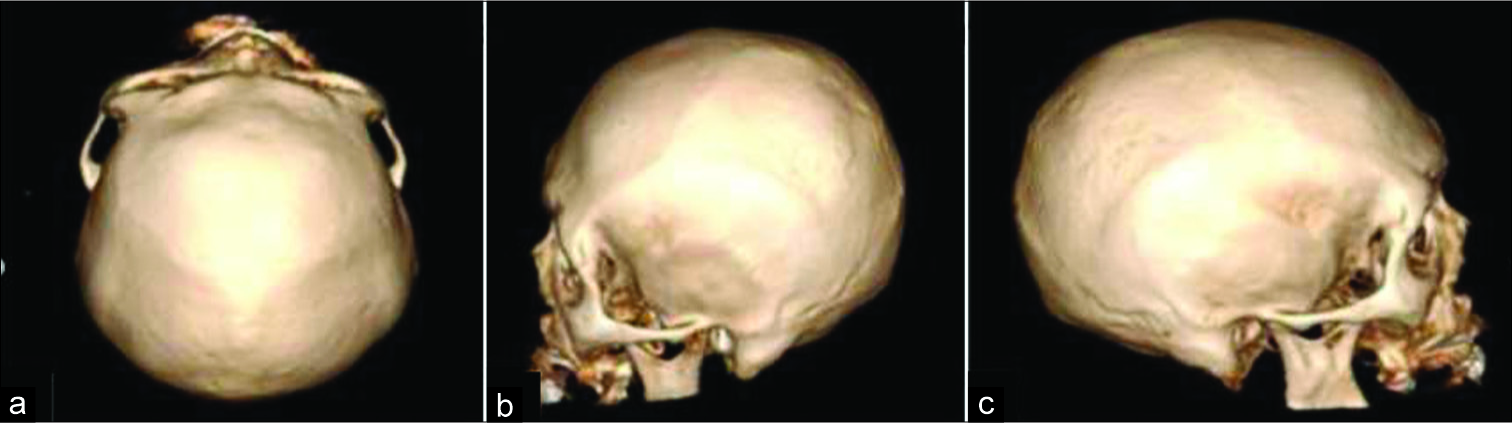
At the examination, a cautious gait was observed with small turns and waning of arms. The static and balance were reasonable and dysmetria on the right side was present. The rest of the neurological examination was clear. A computed tomography (CT) scan performed in 2014 displayed a hypodense image on the right hemisphere, extending from the frontal to the occipital region, which corresponded to a massive CSDH [
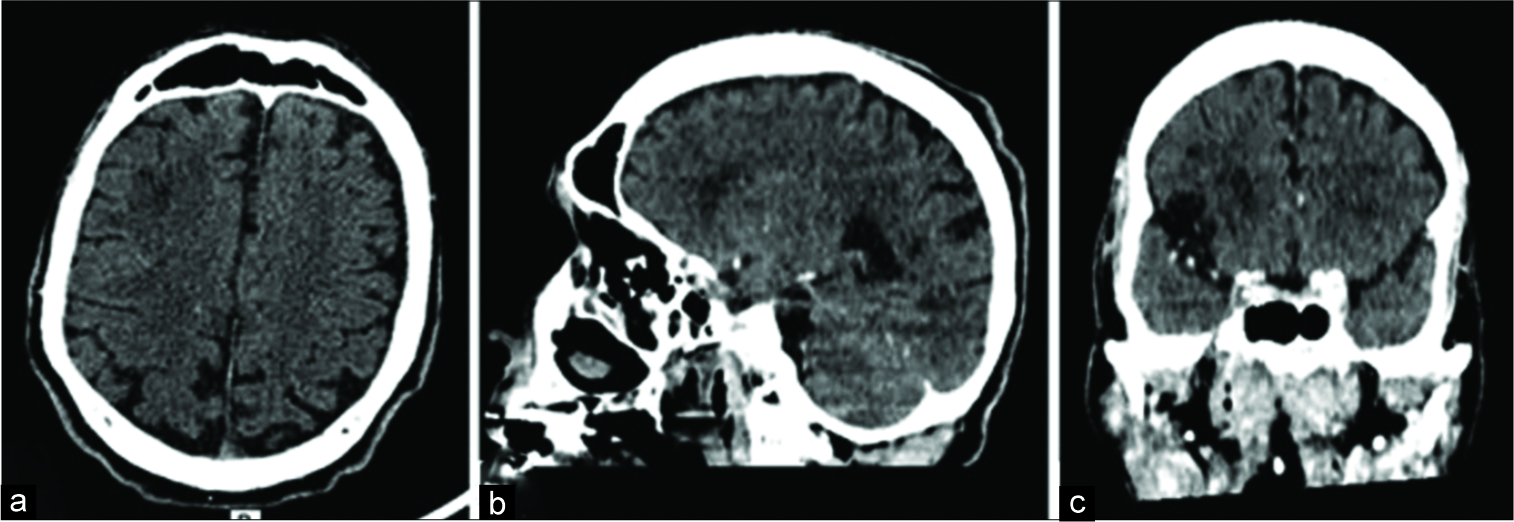
Thus, the patient was referred to the HUAP emergency department to perform a new CT scan to define the appropriate therapy. However, the new CT scan revealed complete reabsorption of the CSDH, with no evidence of a previous surgical approach on the first image and with no surgical trepanation viewed on bone window on the second image [
Therefore, the patient was discharged with follow-up attention to the outpatient neurology clinic.
DISCUSSION
CSDH originates from dural border cells, between the dura mater and arachnoid. Bridge veins that fill this space are stretched due to underlying cerebral atrophy. Traumatic microruptures of the bridge veins lead to extravasation of the blood, creating a real subdural space; otherwise, virtual that happens because a loose cellular layer located in the subdural space is devoid of collagen that fills the third space with dense cellular connections. This absence of collagen, in turn, leads to a decrease of resistance for hematomas formation in that space, favoring its expansion. Due to the imbalance between the mechanisms of injury and tissue repair, there is a propagation of the process and formation of the visceral and parietal neomembranes involving the CSDH. As a consequence, vascular neoformation and enzymatic hyperfibrinolysis occur, resulting in progressive propagation and increase of the hematoma.[
CSDHs are usually treated through a surgical approach, especially in the presence of neurological deficits, hematomas larger than 1 cm in thickness, significant mass effect, and midline deviation. In literature, spontaneous resolution of the CSDH has been rarely reported. However, some theories have been proposed to explain the mechanisms of spontaneous resolution of CSDH.[
The current trend of using nonsurgical therapies has motivated some authors to seek alternative pharmacological treatments. Several alternative treatments to surgery are standard, including clinical observation, relative rest, suspension of anticoagulants, and correction of coagulation disorders. Furthermore, the use of medications such as atorvastatin, corticosteroids, ACE inhibitors, tranexamic acid, and mannitol has been described.[
The predictors that indicate that the CSDH will resolve spontaneously are small volumes, minimal mass effect, settlement in the frontal region, low density in the tomography, and absence of deviation in the midline. Clinically, spontaneous resolution tends to occur in asymptomatic patients or with minimal neurological symptoms.[
In a prospective analysis of 23 patients with CSDH treated with atorvastatin, 22 patients had reduced hematoma volume without surgery. The results of this preliminary study show that oral administration of atorvastatin is safe and effective in the treatment of CSDH, offering a nonsurgical alternative for the treatment of this condition. However, the authors emphasize the need for further randomized studies to support their findings.[
Glover and Labadie suggested that corticosteroids inhibit the formation of the protein permeable membrane and decrease the size of hematoma in an animal model.[
The hypothesis of hyperangiogenesis plays an essential role in the formation of CSDH. Angiotensin-converting enzyme (ACE) inhibitors are believed to be capable of inhibiting this process, disrupting growth, and recurrence after that. A retrospective observational study analyzed the recurrence rate of CSDHs. A total of 310 patients were analyzed, of whom 81 were using ACE inhibitors. The recurrence rate was lower in patients who used ACE inhibitors (5%) than those who did not use (18%).[
It is noteworthy that in the case described herein, Enalapril, an ACE, had been taken for years before the initial diagnosis. It is worth mentioning that the image characteristics, as well as the patient’s clinics, did not corroborate a good prognosis regarding the spontaneous reabsorption of the hematoma. Besides, there was no additional adjuvant or any supportive treatment beyond the use of Enalapril itself. It is exclusively and nonintentionally use in the case herein presented supports the idea of possible action of Enapril, an ACE, as an adjuvant treatment of CSDHs.
Tranexamic acid can be safely used as primary medical therapy to prevent the progression of CSDH in cases without the need for surgical intervention. It acts through the inhibition of hyperfibrinolytic activity and increased vascular permeability, which favors the progressive increase of the lesion. Therefore, they can stabilize the hematoma and allow it to be gradually reabsorbed.[
Importantly, bed rest after the evacuation of CSDH is prescribed for many surgeons throughout the world. Abouzari et al. conducted a prospective randomized study with a 3-month follow-up with 84 patients. The recurrence rate was 19% in the sitting group and 2.3% in the supine group. There were significant differences in the incidence of clinical complications such as atelectasis, pneumonia, bedsores, and deep venous thrombosis among the supine group.[
These results suggest that there is a role for postoperative bed rest, but it is not known whether the same reduction in risk of recurrence could be obtained with <3 days, which could minimize the complications that come together. Therefore, prospective studies are demanding to evaluate the precise time for bed rest where a decrease of recurrence rate of the hematoma happens along with acceptable side effects.[
Even though bed rest is described after the surgery of CSDHs, there is a lack of information about it in a context of nonsurgical patients. Would be bed rest as helpful as seen in postoperative patients? If so, does the volume of hematoma impact the efficacy of exclusively bed rest and medical treatment?
That said, one wonder if conservative treatment would be more often implemented even in cases where large hematomas are identified and no signs of intracranial hypertension are present. Altogether, these unanswered questions stress the need for new studies. These studies should address many variables before implementing conservative treatment as a stand of care in patients otherwise with surgical hematomas.
CONCLUSION
The surgical treatment is still the gold standard and the first option in CSDH >1 cm in diameter, with ventricular compression, midline deviation, and neurological deficit. However, conservative treatment can be a possibility on case of CSDH >1 cm without clinic manifestation or anatomic alterations on investigation. Gradually, several successful nonsurgical therapies for the treatment of these hematomas are reported, although further studies are essential to establish the role of these nonsurgical treatments of CSDHs. In this sense, the pathophysiology of these hematomas and their spontaneous resolution should be better elucidated before adapting conservative treatment for all hematomas >1 cm.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/ have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abouzari M, Rashidi A, Rezaii J, Esfandiari K, Asadollahi M, Aleali H. The role of postoperative patient posture in the recurrence of traumatic chronic subdural hematoma after burr-hole surgery. Neurosurgery. 2007. 61: 794-7
2. Bansal H, Mahajan A, Singh A, Chaudhary A. Spontaneous disappearance of a large chronic subdural hematoma: A Pleasant surprise. Indian J Surg. 2015. 77: 532-4
3. Göksu E, Akyüz M, Uçar T, Kazan S. Spontaneous resolution of a large chronic subdural hematoma: A case report and review of the literature. Turk J Trauma Emerg Surg. 2009. 15: 95-8
4. Gusmão SN, Braga FM, de Melo PM.editors. Complicações tardias do traumatismo cranioencefálico. Manole: Guia de Medicina Ambulatorial e Hospitalar Escola Paulista de Medicina: Neurocirurgia. 2005. p. 21-30
5. Kim HC, Ko JH, Yoo DS, Lee SK. Spontaneous resolution of chronic subdural hematoma: Close observation as a treatment strategy. J Korean Neurosurg Soc. 2016. 59: 628-36
6. Lee GS, Park YS, Min KS, Lee MS. Spontaneous resolution of a large chronic subdural hematoma which required surgical decompression. J Korean Neurosurg Soc. 2015. 58: 301-3
7. Rabelo N, Pereira V, Dos Passos GS, Filho LS, Cicilini A, Rabelo N. Chronic subdural hematoma spontaneous resolution. Arq Bras Neurocir Braz Neurosurg. 2017. 36: 96-100
8. Santarius T, Kirkpatrick PJ, Kolias AG, Hutchinson PJ. Working toward rational and evidence-based treatment of chronic subdural hematoma. Clin Neurosurg. 2010. 57: 112-22
9. Sousa EB.editors. Perfil Epidemiológico Dos Pacientes Submetidos À Drenagem De Hematoma Subdural Crônico No Distrito Federal: Análise De Uma Série Moncêntrica De 778 Pacientes. 2013. 92 F., IL. Dissertação (Mestrado em Ciências Médicas) Universidade De Brasília, Brasília. 2013. p.
10. Teles A, Falavigna A, Kraemer J. Surgical treatment of chronic subdural hematoma: Systematic review and meta-analysis of the literature. Arq Bras Neurocir Braz Neurosurg. 2016. 35: 118-27
11. Wang D, Li T, Tian Y, Wang S, Jin C, Wei H. Effects of atorvastatin on chronic subdural hematoma: A preliminary report from three medical centers. J Neurol Sci. 2014. 336: 237-42
12. Yasuda CL, Morita ME, Nishimori FY, Yasuda AM, Alves HL. Hematoma subdural crônico: Estudo de 161 pacientes operados e a relação com alterações no coagulograma. Arq Neuropsiquiatr. 2003. 61: 1011-4
13. Yilmaz H, Boyali O, Atci IB, Kocaman U. Spontaneous resolution of post-traumatic chronic subdural hematoma: A case report. Pan Afr Med J. 2017. 28: 167-