- Department of Neurosurgery, Ohnishi Neurological Centre, Akashi, Hyogo, Japan
- Department of Neurosurgery, Nara Medical University, Kashihara, Nara, Japan.
Correspondence Address:
Ryosuke Maeoka, Department of Neurosurgery, Ohnishi Neurological Centre, Akashi, Hyogo, Japan.
DOI:10.25259/SNI_572_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ryosuke Maeoka1,2, Ichiro Nakagawa2, Hiroyuki Ohnishi1, Hideyuki Ohnishi1. Staged strategy using a transcarotid approach for acute tandem occlusions with left common carotid artery origin steno-occlusive lesion. 19-Jul-2021;12:364
How to cite this URL: Ryosuke Maeoka1,2, Ichiro Nakagawa2, Hiroyuki Ohnishi1, Hideyuki Ohnishi1. Staged strategy using a transcarotid approach for acute tandem occlusions with left common carotid artery origin steno-occlusive lesion. 19-Jul-2021;12:364. Available from: https://surgicalneurologyint.com/surgicalint-articles/10974/
Abstract
Background: Endovascular treatment for acute tandem occlusion (ATO) of the combination of an ipsilateral extracranial internal carotid artery (ICA) steno-occlusive lesion with concurrent intracranial artery occlusion is challenging. Whether extracranial lesions, especially in cases of the left common carotid artery (LCCA) origin steno-occlusive lesions, should be treated after recanalization of an occluded intracranial artery by mechanical thrombectomy simultaneously in the same session has not been established. We report two cases of successful ATO with LCCA origin steno-occlusive lesions treated by staged retrograde transcarotid LCCA stenting followed emergent mechanical thrombectomy in two sessions because of the tortuous aortic arch.
Case Description: A 61-year-old man with left ICA occlusion and an 82-year-old woman with left middle cerebral artery occlusion underwent emergent mechanical thrombectomy for ATO with LCCA origin stenoocclusive lesions. We achieved recanalization of large vessels, but severe stenosis of LCCAs remained. Because of the tortuous aortic arch, we decided to treat LCCA origin steno-occlusive lesions with staged stenting in the other session followed emergent mechanical thrombectomy. Postoperative courses were uneventful, and their symptoms improved. We performed stenting using a transcarotid approach through CCA cut down for LCCA steno-occlusive lesions without any complications.
Conclusion: The staged strategy leaving LCCA origin stenosis seems to offer a better strategy than the simultaneous strategy for ATO with LCCA origin steno-occlusive lesions. A retrograde transcarotid approach through CCA cut down is recommended for LCCA stenting.
Keywords: Acute tandem occlusion, Left common carotid artery origin steno-occlusive lesions, Retrograde transcarotid approach, Staged strategy
INTRODUCTION
In acute ischemic stroke (AIS) with large vessel occlusion (LVO), recanalization results in good clinical outcomes.[
CASE PRESENTATION
Case 1
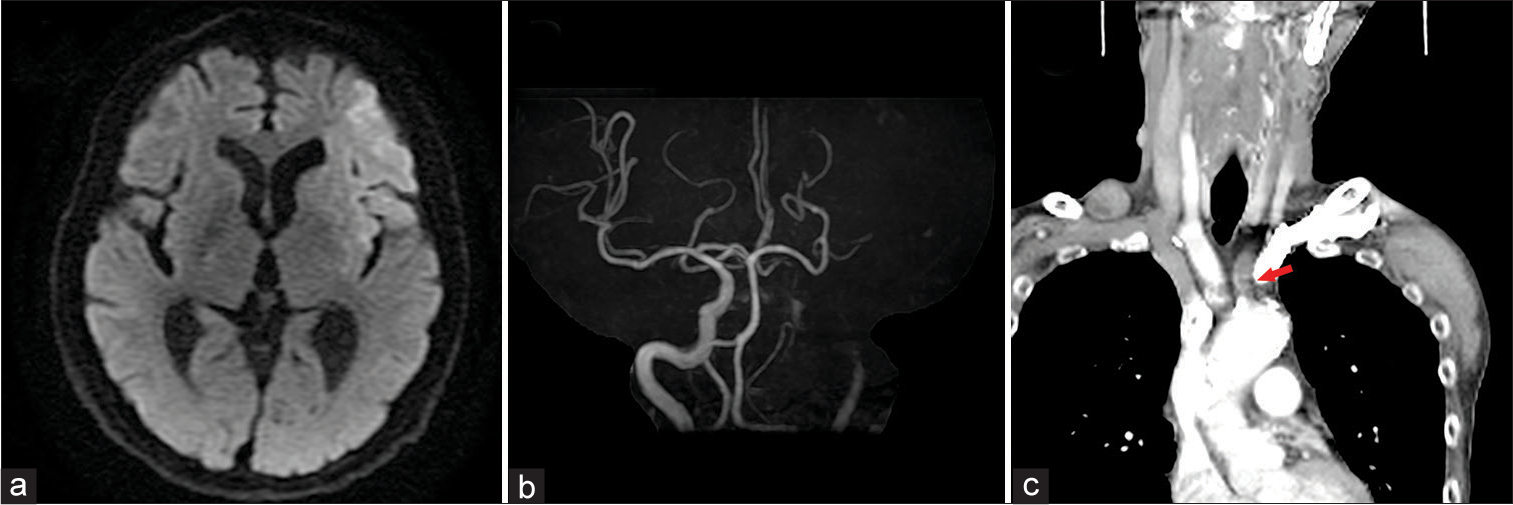
A 61-year-old man with a history of hypertension presented with right hemiparesis and total aphasia within 1 h after symptom onset. National Institutes of Health Stroke Scale (NIHSS) score was 19. Magnetic resonance imaging (MRI) showed acute and subacute infarctions in the left frontal lobe with an Alberta stroke program early computed tomography score (ASPECTS) of 7 on diffusion-weighted imaging (DWI) [
Figure 1:
(a) Magnetic resonance imaging shows acute infarction in the left frontal lobe with an Alberta stroke program early computed tomography score of 7 on diffusion-weighted imaging. (b) Magnetic resonance angiography shows occlusion of the left internal carotid artery. (c) Computed tomography angiography reveals occlusion of the left common carotid artery origin without aortic dissection.
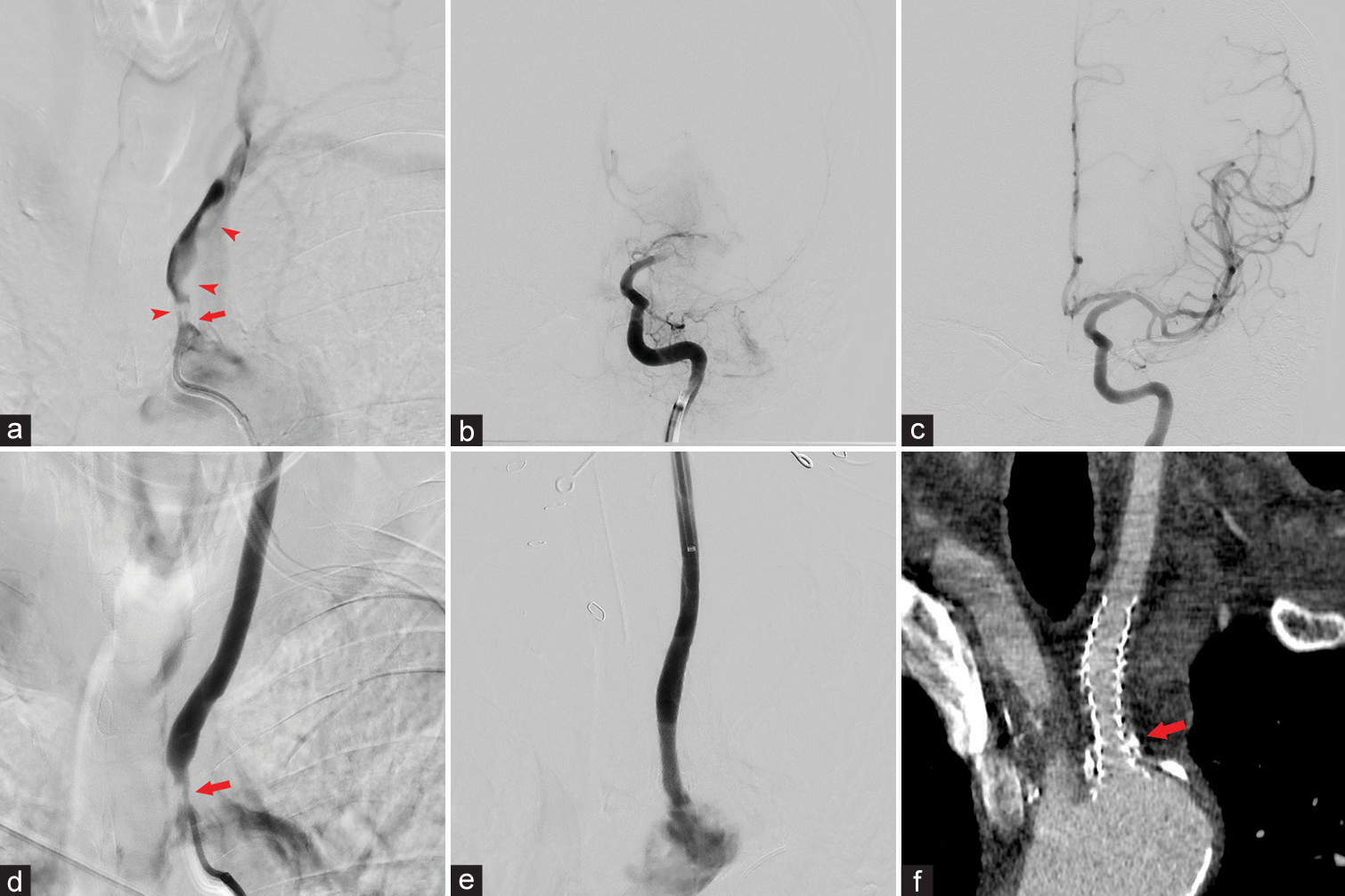
Figure 2:
(a) Angiography of the left common carotid artery (LCCA) demonstrates severe stenosis visualization of the LCCA (red arrow) and thrombus (red arrowhead). (b) Angiography of the internal carotid artery (ICA) reveals occlusion of the left ICA terminus with ICA flow stagnation. (c) Reperfusion of the left middle cerebral artery territory is confirmed. (d) Angiography of the LCCA confirms patency of the LCCA origin (red arrow) at the end of endovascular treatment. (e) We placed a double-layered micromesh stent under breath-hold to prevent misalignment. Angiography confirms successful revascularization of the LCCA. (f) Postoperative computed tomography angiography reveals revascularization of the LCCA origin (red arrow) by successful stenting.
Case 2
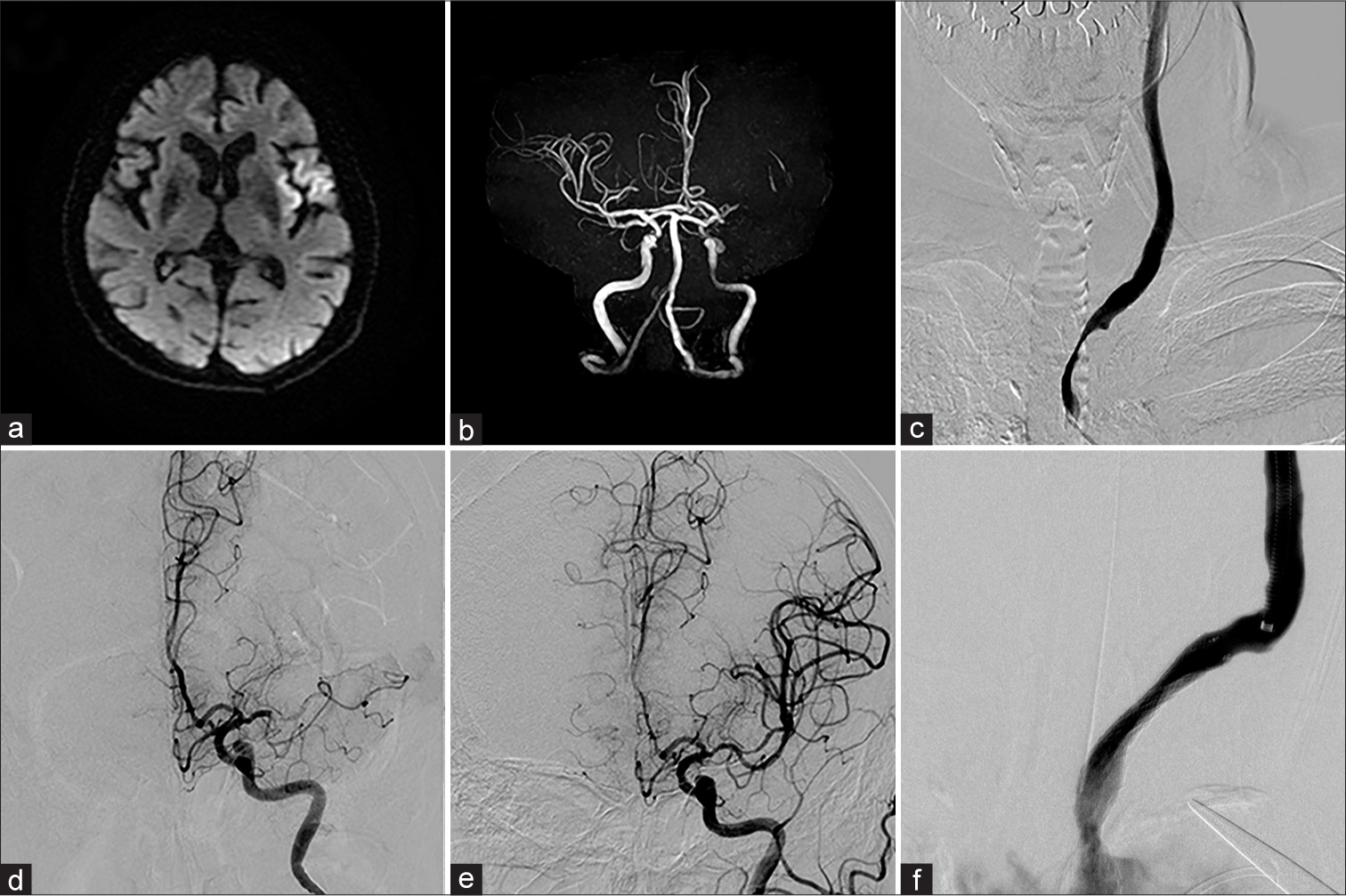
An 82-year-old woman with a history of dyslipidemia, chronic heart failure, and cardiac arrhythmias presented with right hemiparesis and motor aphasia 2.5 h after symptom onset. NIHSS was 11. MRI/MRA showed acute infarction with a DWI-ASPECTS of 8 and occlusion of the left MCA [
Figure 3:
(a) Magnetic resonance imaging (MRI) shows acute infarction in the left frontal lobe with an Alberta stroke program early computed tomography score of 8 on diffusion-weighted imaging. Magnetic resonance angiography (MRA) shows occlusion of the left middle cerebral artery (MCA). (b) MRI shows acute infarction in the left frontal lobe with an Alberta Stroke Program Early Computed Tomography score of 8 on diffusion-weighted imaging. MRA shows occlusion of the left MCA. (c) Angiography of the left common carotid artery (LCCA) demonstrates severe stenosis of the LCCA origin. (d) Angiography of the internal carotid artery reveals left MCA occlusion. (e) Reperfusion of the left MCA territory is confirmed. (f) Angiography confirms successful revascularization of the LCCA by successful stenting.
DISCUSSION
We have presented two cases of successful ATO with LCCA origin steno-occlusive lesions treated under a staged strategy. LCCA origin occlusive lesions are generally atherosclerotic, but Takayasu arteritis or radiation arteritis and aortic dissection should also be considered.[
During LCCA stenting using a trans-femoral approach, anatomical limitations and the lack of guiding catheter support make stenting difficult. Aortic arch manipulation represents the greatest risk for microembolization in carotid artery stenting.[
CONCLUSION
We must consider LCCA origin steno-occlusive lesions as one cause of AIS with LVO. The staged strategy leaving LCCA origin stenosis seems to offer a better strategy than the simultaneous strategy for ATO with LCCA origin stenoocclusive lesions. A retrograde trans-carotid approach via CCA cut down was recommended for LCCA stenting.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Al-Mubarak N, Roubin GS, Vitek JJ, Iyer SS, New G, Leon MB. Effect of the distal-balloon protection system on microembolization during carotid stenting. Circulation. 2001. 104: 1999-2002
2. Anadani M, Spiotta A, Alawieh A, Turjman F, Piotin M, Steglich-Arnholm H. Effect of extracranial lesion severity on outcome of endovascular thrombectomy in patients with anterior circulation tandem occlusion: Analysis of the TITAN registry. J Neurointerv Surg. 2019. 11: 970-4
3. Gonzalez Garcia A, Moniche F, Escudero-Martinez I, Mancha F, Tomasello A, Ribo M. Clinical predictors of hyperperfusion syndrome following carotid stenting: Results from a national prospective multicenter study. JACC Cardiovasc Interv. 2019. 12: 873-82
4. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM. Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet. 2016. 387: 1723-31
5. Naylor AR, Ricco JB, de Borst GJ, Debus S, de Haro J, Halliday A.editors. Editor’s choice-management of atherosclerotic carotid and vertebral artery disease: 2017 Clinical practice guidelines of the european society for vascular surgery (ESVS). Eur J Vasc Endovasc Surg. 2018. 55: 3-81
6. Papanagiotou P, Ntaios G. Endovascular thrombectomy in acute ischemic stroke. Circ Cardiovasc Interv. 2018. 11: e005362
7. Saadoun D, Lambert M, Mirault T, Resche-Rigon M, Koskas F, Cluzel P. Retrospective analysis of surgery versus endovascular intervention in Takayasu arteritis: A multicenter experience. Circulation. 2012. 125: 813-9
8. van de Weijer MA, Vonken EJ, de Vries JP, Moll FL, Vos JA, de Borst GJ. Technical and clinical success and long-term durability of endovascular treatment for atherosclerotic aortic arch branch origin obstruction: Evaluation of 144 procedures. Eur J Vasc Endovasc Surg. 2015. 50: 13-20