- Department of Neurosurgery, Shiga University of Medical Science, Otsu, Shiga, Japan
Correspondence Address:
Naoki Nitta
Department of Neurosurgery, Shiga University of Medical Science, Otsu, Shiga, Japan
DOI:10.4103/2152-7806.181822
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kawano H, Nitta N, Nozaki K. Straight sinus thrombosis during neurosurgical operation. Surg Neurol Int 05-May-2016;7:50
How to cite this URL: Kawano H, Nitta N, Nozaki K. Straight sinus thrombosis during neurosurgical operation. Surg Neurol Int 05-May-2016;7:50. Available from: http://surgicalneurologyint.com/surgicalint_articles/straight-sinus-thrombosis-during-neurosurgical-operation/
Abstract
Background:Perioperative straight sinus thrombosis is extremely rare.
Case Description:A 59-year-old female was admitted to our department because of incidentally found small anterior cerebral artery (A1) aneurysm with microbleeding. After clipping the cerebral aneurysm, she had delayed emergence from anesthesia, total aphasia, and right hemiparesis. Fluid-attenuated inversion recovery (FLAIR) magnetic resonance imaging (MRI) of the head showed hyperintensity in the bilateral caudate nuclei, putamina, and thalami, and computed tomography of the head showed a hyperdense straight sinus, suggesting straight sinus thrombosis. Her neurologic symptoms improved gradually, and she achieved a full clinical recovery, with radiological evidence of recanalization of the straight sinus at follow-up.
Conclusion:The possibility of straight sinus thrombosis should be considered in postoperative patients with unexplained postoperative deficits when MRI demonstrates hyperintensity in the bilateral basal ganglia and thalami on FLAIR signal images.
Keywords: Basal ganglia, bilateral, postoperative, straight sinus thrombosis, thalamus
INTRODUCTION
Cerebral venous sinus thrombosis (CVST) is an infrequent form of stroke with several risk factors such as oral conceptive, postpartum state, infection, and malignancies. CVST has been reported to be extraordinary rare after an intracranial surgery.[
CASE REPORT
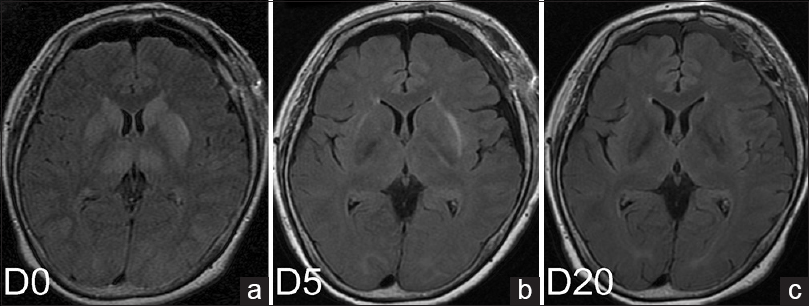
A 59-year-old woman was admitted in our Neurosurgical Department because of a small left A1 aneurysm suspected of microbleeding. The patient had a history of Graves’ disease and hypothyroidism. She underwent clipping of the aneurysm using pterional approach. There were no intraoperative complications; no cerebral contusion, premature rupture, or brain swelling. After the operation, she had delayed emergence from anesthesia, total aphasia, and right hemiparesis (the Medical Research Council scale; upper and lower limbs: 1/5). Glasgow coma scale scored 7 (E: 2; V: 1; M: 4). A plane computed tomographic (CT) scan of the head, obtained immediately after the operation, showed no intracerebral hemorrhage. Fluid-attenuated inversion recovery (FLAIR) magnetic resonance imaging (MRI) of the head after the CT scan showed moderate hyperintensity in the bilateral caudate nuclei, putamina, and thalami [
Although we suspected straight sinus thrombosis after reviewing the postoperative CT and MRI images, a repeat MRI scan the day after surgery showed normal enhancement of the straight sinus on postcontrast T1-weighted images (T1WIs), which looked the same as the straight sinus shown by preoperative digital subtraction angiography (DSA). DWI showed hyperintense basal ganglia, and we treated her with a thromboxane A2 inhibitor. Results of hematologic test; tests of coagulation, renal function, and liver function; electrolyte levels; complement levels, C3, and C4; levels of thyroid-stimulating hormone, free T3 and free T4; anti-DNA antibodies; levels of protein S and protein C; levels of anticardiolipin antibodies; and level of rheumatoid factor were normal. At 5 days after the operation, FLAIR showed decreased hyperintensity in the basal ganglia and thalami, DWI no new lesion, and postcontrast T1WI no CVST [
At 6 days after the operation, postcontrast CT of the abdomen showed a thrombus in the right femoral vein, we started administration of heparin and then warfarin. We continued the administration of warfarin, and the prothrombin time-international normalized ratio was between 1.5 and 2.5. At 20 days after the operation, FLAIR showed no hyperintensity in the basal ganglia or thalami [
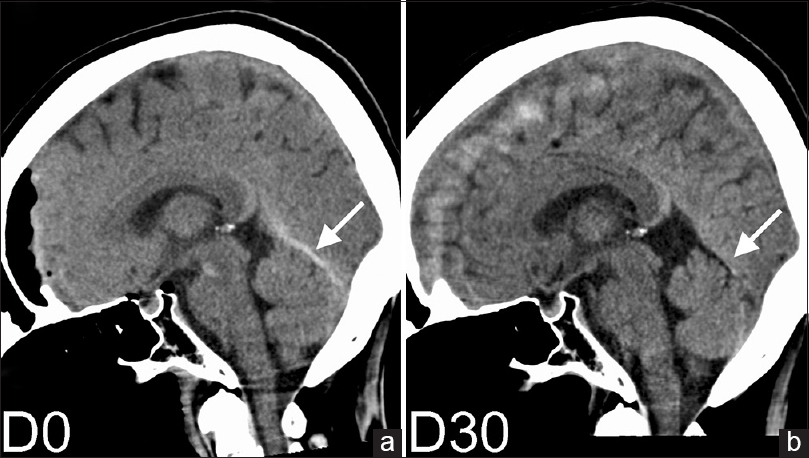
We reviewed postoperative sagittal plane CT images, and we found that the CT immediately after the operation revealed transient hyperdensity in the straight sinus, which hyperdensity was not observed on CT at 1 month after the operation [Figure
DISCUSSION
The present report describes a case of straight sinus thrombosis after an intracranial surgery. Although we did not recognize the patient's condition at the onset or treat her with any anticoagulants or endovascular intervention, the straight sinus appears to have rapidly recanalized leading to the resolution of symptoms.
The patient had no major risk factors such as pregnancy, puerperium, oral conceptive use, infection, malignancy, or trauma.[
Why did neurosurgery trigger CVST in the present case? Almost all CVST after brain surgery followed procedures performed in the vicinity of the sinuses.[
Although we could not initially consider straight sinus thrombosis in this case; fortunately, it resolved spontaneously. In the previous two cases of perioperative straight sinus thrombosis, the patients also had sagittal sinus thrombosis and died on the 2nd and 9th postoperative days, respectively.[
CONCLUSION
We report a case of a 59-year-old woman with straight sinus thrombosis after a neurosurgical operation. If sagittal plane CT image shows a hyperdense straight sinus or FLAIR shows hyperintensity in the bilateral basal ganglia and/or thalami, we should consider the possibility of straight sinus thrombosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We are grateful to Toshihiro Yokoi and Hiroki Matsui for fruitful discussions and helpful comments.
References
1. Ben-Dov M, Inbar E, Steiner I. Cerebral straight sinus thrombosis: An unusual cause of confusion. JAMA Neurol. 2015. 72: 1527-
2. Canhão P, Batista P, Falcão F. Lumbar puncture and dural sinus thrombosis – A causal or casual association?. Cerebrovasc Dis. 2005. 19: 53-6
3. Coutinho JM, Zuurbier SM, Stam J. Declining mortality in cerebral venous thrombosis: A systematic review. Stroke. 2014. 45: 1338-41
4. Ferro JM, Canhão P, Bousser MG, Stam J, Barinagarrementeria F, Stolz E. ISCVT Investigators. Cerebral venous thrombosis with nonhemorrhagic lesions: Clinical correlates and prognosis. Cerebrovasc Dis. 2010. 29: 440-5
5. Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F. ISCVT Investigators. Prognosis of cerebral vein and dural sinus thrombosis: Results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke. 2004. 35: 664-70
6. Hegde AN, Mohan S, Lath N, Lim CC. Differential diagnosis for bilateral abnormalities of the basal ganglia and thalamus. Radiographics. 2011. 31: 5-30
7. Iwashita T, Kitazawa K, Koyama J, Nagashima H, Koyama T, Tanaka Y. Subtle computed tomography abnormalities in cerebral deep sinus thrombosis. J Clin Neurosci. 2007. 14: 68-71
8. Kozasa Y, Takaseya H, Koga Y, Hiraki T, Mishima Y, Niiyama S. A case of delayed emergence from anesthesia caused by postoperative brain edema associated with unexpected cerebral venous sinus thrombosis. J Anesth. 2013. 27: 764-7
9. Lega BC, Yoshor D. Postoperative dural sinus thrombosis in a patient in a hypercoagulable state.Case report. J Neurosurg. 2006. 105: 772-4
10. Ohata K, Haque M, Morino M, Nagai K, Nishio A, Nishijima Y. Occlusion of the sigmoid sinus after surgery via the presigmoidal-transpetrosal approach. J Neurosurg. 1998. 89: 575-84
11. Redhu S, Mohd Abdul M, Pandey P, Devaragudi TS. Distant cerebral venous sinus thrombosis in meningioma surgery: A rare complication. Neurol India. 2013. 61: 180-1
12. Schuenke M, Schulte E, Schumacher U, Rude J.editors. Atlas of Anatomy; Head and Neuroanatomy. Stuttgart: Thieme; 2007. p.
13. Sidhu M, Footitt D, Donaldson I, Hughes S, Wuppalapati S, Emsley HC. Intact neurological outcome after neurointerventional treatment for intracranial venous thrombosis with straight sinus involvement. BMJ Case Rep 2013. 2013. p.