- Department of Neurosurgery, Saiseikai Kumamoto Hospital, Kumamoto, Japan
- Department of Neurosurgery, School of Medicine, Kumamoto University, Kumamoto, Japan
Correspondence Address:
Hiroki Uchikawa
Department of Neurosurgery, School of Medicine, Kumamoto University, Kumamoto, Japan
DOI:10.4103/2152-7806.160320
Copyright: © 2015 Uchikawa H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Uchikawa H, Kai Y, Ohmori Y, Kuratsu J. Strategy for endovascular coil embolization of a penetrating vertebral artery injury. Surg Neurol Int 08-Jul-2015;6:117
How to cite this URL: Uchikawa H, Kai Y, Ohmori Y, Kuratsu J. Strategy for endovascular coil embolization of a penetrating vertebral artery injury. Surg Neurol Int 08-Jul-2015;6:117. Available from: http://surgicalneurologyint.com/surgicalint_articles/strategy-for-endovascular-coil-embolization-of-a-penetrating-vertebral-artery-injury/
Abstract
Background:Penetrating vertebral artery injuries (VAIs) are even rarer than carotid artery injuries. For anatomical reasons, the surgical management of VAI is difficult, and endovascular management often yields a good outcome. We report our strategy for the endovascular treatment of a patient with a penetrating VAI at the V2 segment of the left vertebral artery.
Case Description:In a fall on a large rake, a 76-year-old man was stabbed in the left neck by three tines. Although he manifested no neurological deficits, computed tomography (CT) suggested penetrating VAI. Digital subtraction angiography confirmed VAI and extravasation, and he underwent endovascular coil embolization. Two microcatheters, inserted proximal and distal to the injury sites, were used for successful endovascular coil embolization. Postoperative magnetic resonance imaging - and single photon emission CT studies denied cerebral infarction and a decrease in cerebral perfusion. The patient exhibited no neurological deficits and was able to leave the hospital on foot.
Conclusion:This is the rare documentation of a patient whose penetrating VAI was treated by simultaneous coil embolization and foreign body removal. Imaging studies confirmed the patency and perfusion of the intracranial artery. Our treatment strategy produced a good outcome in this unusual patient.
Keywords: Embolization, penetrating neck trauma, stab wound, traumatic vertebral artery injury
INTRODUCTION
Only approximately 0.5% of all trauma patients present with traumatic vertebral artery injury (VAI) which is even more rare than carotid artery injury.[
CASE REPORT
In a fall on a large rake, this 76-year-old man was stabbed in the left neck by three tines [
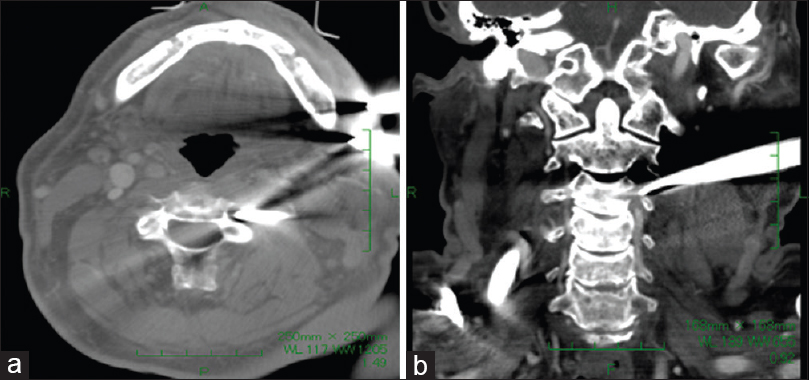
A plain computed tomography (CT) scan showed that one of the tines penetrated between the C3/4 transverse foramen suggesting left vertebral artery damage. The other tine was attached to the hyoid bone and thyroid cartilage. His epiglottis was slightly swollen; there was no air leak, and he reported no respiratory discomfort. Other important structures such as the spinal cord and other major arteries and veins were intact. CT angiography (CTA) demonstrated obstruction of the left vertebral artery at the V2 segment proximal to the penetrating tine [
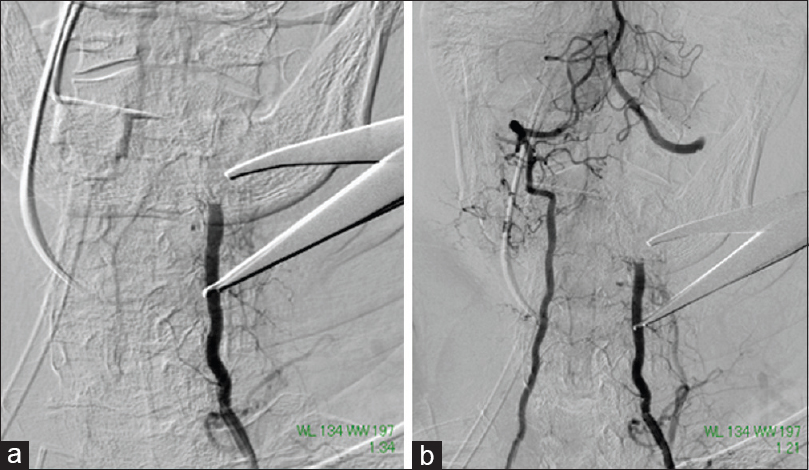
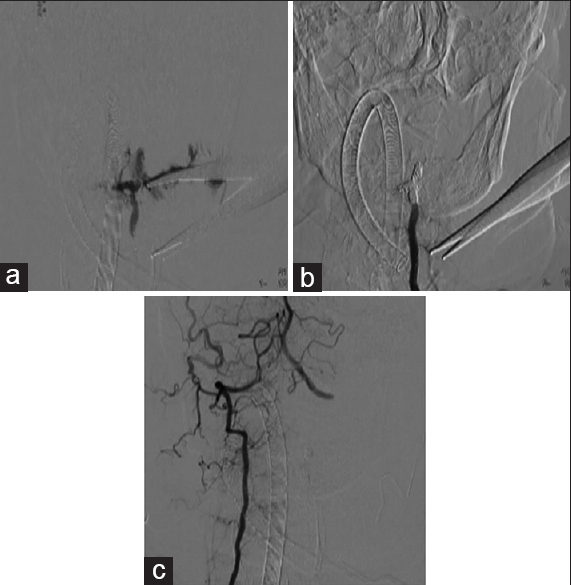
After inserting a 6-Fr guiding catheter (Slim guide®, Medikit, Japan) into the left vertebral artery, we navigated two microcatheters (Excelsior®, Stryker Neurovascular, USA) into the proximal and distal sides to the injury point. It might be better that we use a stent to suppress the bleeding point and preserve anterograde blood flow, but vertebral artery at the injury point was too narrow to pass the stent device. A 4-Fr catheter was then inserted into the right vertebral artery for evaluation of the contralateral circulation. In the middle of slowly and carefully withdrawing the metal tine, we noted extravasation and decided that endovascular embolization was indicated. We first performed coil embolization at the entry - and the proximal side using the microcatheter inserted at the proximal side. Then we embolized the distal side to the site of entry using the distal microcatheter. Extravasation ceased after complete embolization of the left vertebral artery [
Figure 4
(a) Digital subtraction angiography (DSA) performed after injecting the left vertebral artery via a microcatheter showed extravasation from the vessel upon removal of the tine. (b) DSA performed after injecting the left vertebral artery via a guiding catheter showed no extravasation from the left vertebral artery after embolization. (c) DSA performed after right vertebral artery injection showed good contralateral vertebral artery flow. The damaged vessel was not contrast-enhanced
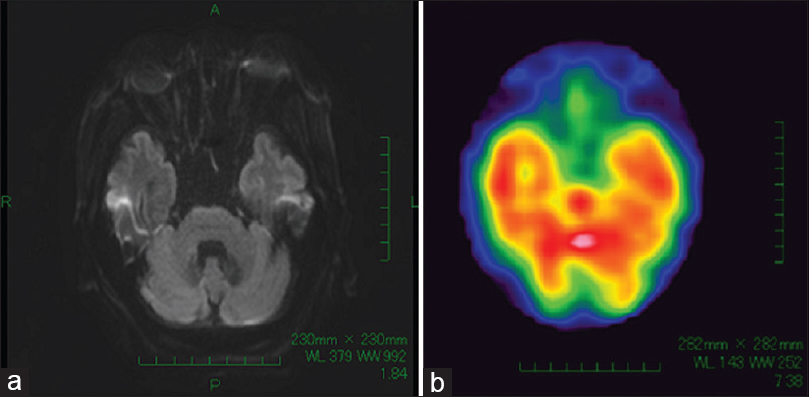
Postoperative magnetic resonance imaging showed no evidence of cerebral infarction and single photon emission CT (SPECT) demonstrated normal cerebral perfusion [
DISCUSSION
Traumatic VAIs are seen in approximately 0.5% of all trauma patients.[
The major problem in the management of VAI is the severe limitation with direct open access to the vertebral artery. Because these vessels pass into the transverse foramen, proximal and distal - and surgical local control is difficult.[
In our patient, plain cervical CT revealed no severe spinal or vertebral damage. However, immediate withdrawal of the tines would have worsened our patient's situation. We confirmed our suspicion of VAI by performing CTA before their removal. DSA showed no flow in the posterior circulation on the affected side. Collateral circulation from the right vertebral artery was good, and the bilateral posterior communicating arteries were of the fetal type. These findings indicated that safe embolization of the left vertebral artery was possible. If symptomatic case of the vertebrobasilar ischemia, we treated in the same way, because active bleeding was most fatal. Furthermore, it would be difficult to rescue ischemia because it took too long time from the onset. We inserted two microcatheters at sites proximal and distal to the damaged artery to embolize both sides simultaneously because their proximal introduction alone would not have allowed control of the distal flow after embolization of the proximal side. Although distal control might not always be necessary, we purposely inserted microcatheter at the distal side to the damaged point for safety. If microcatheter could not be inserted at the distal side anterogradely, we would insert microcatheter from right vertebral artery retrogradely. Our use of the 6-Fr guiding catheter, which facilitates the application of advanced techniques that involve multiple microdevices rendered endovascular treatment safe and easy.[
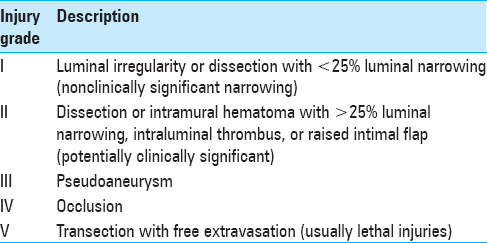
Traumatic VAI can be endovascularly treated with coils, balloons, or stents.[
References
1. Atar E, Griton I, Bachar GN, Bartal G, Kluger Y, Belenky A. Embolization of transected vertebral arteries in unstable trauma patients. Emerg Radiol. 2005. 11: 291-4
2. Albuquerque FC, Javedan SP, McDougall CG. Endovascular management of penetrating vertebral artery injuries. J Trauma. 2002. 53: 574-80
3. Biffl WL, Moore EE, Elliott JP, Ray C, Offner PJ, Franciose RJ. The devastating potential of blunt vertebral arterial injuries. Ann Surg. 2000. 231: 672-81
4. Biffl WL, Moore EE, Offner PJ, Brega KE, Franciose RJ, Burch JM. Blunt carotid arterial injuries: Implications of a new grading scale. J Trauma. 1999. 47: 845-53
5. Cothren CC, Moore EE, Biffl WL, Ciesla DJ, Ray CE, Johnson JL. Cervical spine fracture patterns predictive of blunt vertebral artery injury. J Trauma. 2003. 55: 811-3
6. de los Reyes RA, Moser FG, Sachs DP, Boehm FH. Direct repair of an extracranial vertebral artery pseudoaneurysm: Case report and review of the literature. Neurosurgery. 1990. 26: 528-33
7. Desouza RM, Crocker MJ, Haliasos N, Rennie A, Saxena A. Blunt traumatic vertebral artery injury: A clinical review. Eur Spine J. 2011. 20: 1405-16
8. Eastman AL, Chason DP, Perez CL, McAnulty AL, Minei JP. Computed tomographic angiography for the diagnosis of blunt cervical vascular injury: Is it ready for primetime?. J Trauma. 2006. 60: 925-9
9. Fassett DR, Dailey AT, Vaccaro AR. Vertebral artery injuries associated with cervical spine injuries: A review of the literature. J Spinal Disord Tech. 2008. 21: 252-8
10. Gracias VH, Reilly PM, Philpott J, Klein WP, Lee SY, Singer M. Computed tomography in the evaluation of penetrating neck trauma: A preliminary study. Arch Surg. 2001. 136: 1231-5
11. Herrera DA, Vargas SA, Dublin AB. Endovascular treatment of traumatic injuries of the vertebral artery. AJNR Am J Neuroradiol. 2008. 29: 1585-9
12. Kai Y, Ohmori Y, Watanabe M, Kaku Y, Morioka M, Hirano T. A 6-fr guiding catheter (slim guide(®)) for use with multiple microdevices. An experimental study. Interv Neuroradiol. 2013. 19: 7-15
13. Karadag O, Gürelik M, Berkan O, Kars HZ. Stab wound of the cervical spinal cord and ipsilateral vertebral artery injury. Br J Neurosurg. 2004. 18: 545-7
14. Lee YJ, Ahn JY, Han IB, Chung YS, Hong CK, Joo JY. Therapeutic endovascular treatments for traumatic vertebral artery injuries. J Trauma. 2007. 62: 886-91
15. Miller PR, Fabian TC, Bee TK, Timmons S, Chamsuddin A, Finkle R. Blunt cerebrovascular injuries: Diagnosis and treatment. J Trauma. 2001. 51: 279-85
16. Xia X, Zhang F, Lu F, Jiang J, Wang L, Ma X. Stab wound with lodged knife tip causing spinal cord and vertebral artery injuries: Case report and literature review. Spine (Phila Pa 1976). 2012. 37: E931-4