- Department of Neurosurgery, Cristo Redentor Hospital, Porto Alegre, Brazil
- Federal University of Pelotas, Pelotas, Brazil
- Brazilian Lutheran University, Canoas, Brazil
- McGill Scoliosis and Spine Group, McGill University, Montreal, QC, Canada.
- Department of Neurosurgery, Caxias do Sul University, RS, Brazil,
Correspondence Address:
Otávio Garcia Martins
Department of Neurosurgery, Caxias do Sul University, RS, Brazil,
DOI:10.25259/SNI_512_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Guilherme Finger, Andre Martins de Lima Cecchini, Ericson Sfreddo, Felipe Martins de Lima Cecchini, Otávio Garcia Martins, Tiago Paczko Bozko Cecchini, Alisson Roberto Teles, Asdrubal Falavigna. Subaxial spine arthrodesis in patients with spine fractures and facet joint dislocations: Is magnetic resonance imaging required to determine the optimal surgical approach?. 06-Dec-2019;10:239
How to cite this URL: Guilherme Finger, Andre Martins de Lima Cecchini, Ericson Sfreddo, Felipe Martins de Lima Cecchini, Otávio Garcia Martins, Tiago Paczko Bozko Cecchini, Alisson Roberto Teles, Asdrubal Falavigna. Subaxial spine arthrodesis in patients with spine fractures and facet joint dislocations: Is magnetic resonance imaging required to determine the optimal surgical approach?. 06-Dec-2019;10:239. Available from: http://surgicalneurologyint.com/surgicalint-articles/9784/
Abstract
Background: The medical literature suggests that facet dislocations (FDs) must be managed surgically, even in the absence of spinal cord injury. In fact, there is no standard guideline for managing FD cases and whether magnetic resonance imaging (MRI) should be utilized for optimizing treatment planning.
Methods: Fifteen cases of FD were evaluated twice by nine spine surgeons. The first assessment included computed tomography (CT) images only. Secondarily, original CT studies were supplemented with MRI. In each case, the participating surgeon had to acknowledge whether and what surgical treatment they would offer. Data for the two responses from all nine surgeons were then compared.
Results: Based on CT images alone, there was no consensus regarding treatment choices in 13 cases, and a trend toward consensus in just two instances (κ = 0.01). When MRI scans were added to CT studies, among the 15 cases evaluated, 10 cases demonstrated a trend toward consensus, and in 1 case consensus was achieved. The Kappa interpersonal agreement based on MRI was 0.13. The analysis of the answers by each contributor in each case demonstrated that in 58.51% of cases the surgical treatment options were changed when analyzed by CT + MRI, in comparison to the options indicated based on CT alone.
Conclusion: It appears that obtaining an MRI in addition to a CT before spine surgery for FD is essential mandatory, as it changed the treatment option in nearly 60% of cases.
Keywords: Arthrodesis, Cervical vertebrae, Fracture dislocation, Spinal fusion, Spine
INTRODUCTION
The Subaxial Injury Classification System and Severity Score (SLICS) suggests that unilateral or bilateral facet dislocations (FD) should be managed surgically, even in the absence of a spinal cord injury (SCI).[
MATERIALS AND METHODS
Contributors profile questionnaire
Nine spine surgeons, members of the Brazilian Spine Society (2018), responded to questionnaires; they provided personal data and obtained Institutional Review Board/Hospital consent to participate in the study.
Study design
A cross-sectional study surveyed 15 cases of traumatic subaxial unilateral or bilateral FD (2016–2017). Each surgeon was asked to evaluate each case at two different intervals, using the first CT alone followed by both CT and MR studies. They subsequently recommend anterior, posterior, or circumferential cervical surgery. If the latter was chosen, they had to choose the order in which to perform the anterior and posterior cervical procedures. They first analyzed the 15 cases; secondarily, the cases were presented in a different order (typically within the next 30 days). Following the second questionnaire, the authors were asked if they believed that their indications for each case were similar utilizing CT versus CT and MR findings.
Statistical analysis
Statistical analysis was performed using the SPSS program (IBM v22.0, Chicago, IL). Categorical data will be presented as counts and percentages. The Fleiss’ kappa index was used to analyze the intrapersonal concordance between the first and second questionnaires and the interpersonal concordance. The Fleiss’ kappa index concordance ranges from 0 to 1 and is classified as low (0–0.4), moderate (0.5–0.7), or high concordance (0.8–1). The clinical scenarios were allocated in three different categories according to the agreement of the responses: established consensus (>80%), consensus tendency (between 60% and 80%), and no consensus (<60%).
RESULTS
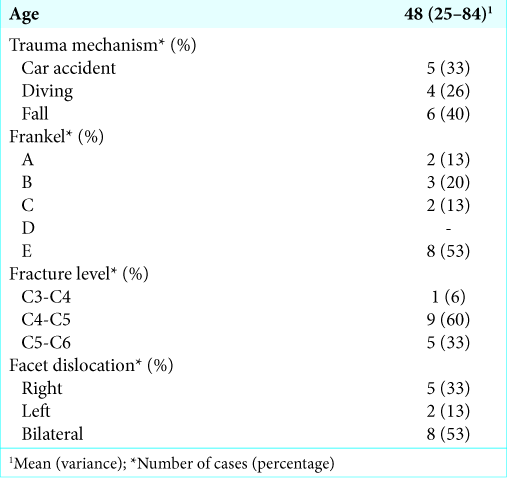
Sample characteristics
Contributors profile
The mean age of the contributors was 45.66 years-old with a mean of 15.33 (+10.35) years of experience with spine surgery. The mean number of the annual spine and cervical spine surgeries per contributors was 185.33 (+82.04) and 33.33 (+25.49), respectively.
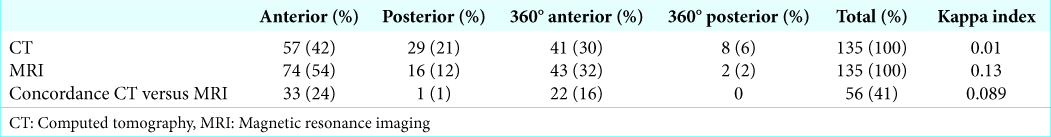
Treatment indications based on clinical data and CT images
When contributors analyzed clinical data and CT images, there was no consensus achieved in any of the 15 cases in this survey. Kappa statistic measures of interpersonal agreement of the answers based on CT evidenced a value of 0.01 [
Treatment indication based on clinical data, CT, and MRI
When contributors analyzed the cases based on clinical data, and both CT and MRI studies, there was a more uniform pattern of treatment recommendations, with a trend toward consensus or consensus achievement in 10 cases and 1 case, respectively. The kappa statistic measure of the interpersonal agreement for the answers based on MRI was 0.13 [
Comparison of answers in the two moments
The authors compared the answers by each contributor in each case when analyzing the CT versus CT + MRI. Surgical approach remained the same in 56 instances (41, 48%). However, in 79 (58, 51%) instances, the surgical treatment based on CT alone was different versus CT + MRI. The kappa index for the comparison of surgical approach indicated by CT and CT + MRI was 0.089.
Of interest, most surgeons did not notice the change of indication for the surgical approach and believed that the treatment proposed was the same for each case regardless of the exam. A total of 79 indications changed when contributors analyzed the MRI. However, in only 33 cases, this modification was noticed. The kappa index for self-perception of treatment change and real treatment change was 0.081.
DISCUSSION
The authors identified a lack of uniformity regarding the optimal surgical approach to FD among experienced spine surgeons (e.g. anterior, posterior, circumferential) when the case analysis was based on CT alone. Notably, however, there was a tendency towards consensus in most cases when MRI scans were additionally performed. Here, most critically, MRI studies in addition to CT scans changed the surgical choice in nearly 60% of FD cases.
The literature reports no significant differences in neurological recovery, fusion rates or long-term complains when anterior or posterior stabilization and fusion were compared.[
Even though creating a protocol is beyond the scope of this study, authors believe that, according to this study, MRI proved to be critical to the management of cervical spine trauma with FD. The higher therapeutic concordance among spine surgeons when MRI was added to the case demonstrates that MRI shows details (such as disc herniations ventral to the spinal cord or ligamentous injury) that help the spine surgeon to get a better understanding of the case and are important to the final therapeutic decision.
CONCLUSION
No single surgical technique/approach best provides surgical decompression/alignment for FD accompanying cervical SCI. However, adding MR to CT examinations before making the final surgical decision altered the surgeon plan in nearly 60% of patients in this series.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Authors appreciate Paulo Valdeci Worm MD Ph.D., Tobias Ludwig does Nascimento MD MSc, Pedro Antonelli MD, Vinicius Benites MD, Marcelo Simões MD, and Sérgio Zylbersztejn MD, for their contribution in this article.
References
1. Brodke DS, Anderson PA, Newell DW, Grady MS, Chapman JR. Comparison of anterior and posterior approaches in cervical spinal cord injuries. J Spinal Disord Tech. 2003. 16: 229-35
2. Dvorak MF, Fisher CG, Fehlings MG, Rampersaud YR, Öner FC, Aarabi B. The surgical approach to subaxial cervical spine injuries: An evidence-based algorithm based on the SLIC classification system. Spine (Phila Pa 1976). 2007. 32: 2620-9
3. Khezri N, Ailon T, Kwon BK. Treatment of facet injuries in the cervical spine. Neurosurg Clin N Am. 2017. 28: 125-37
4. Lins CC, Prado DT, Joaquim AF. Surgical treatment of traumatic cervical facet dislocation: anterior, posterior or combined approaches?. Arq Neuropsiquiatr. 2016. 74: 745-9