- Department of Neurological Surgery, University of Wisconsin-Madison, Madison, Wisconsin, United States.
DOI:10.25259/SNI_136_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Evalina Bond, James A. Stadler. Subdural empyema caused by Morganella morganii. 01-Aug-2020;11:216
How to cite this URL: Evalina Bond, James A. Stadler. Subdural empyema caused by Morganella morganii. 01-Aug-2020;11:216. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10169
Abstract
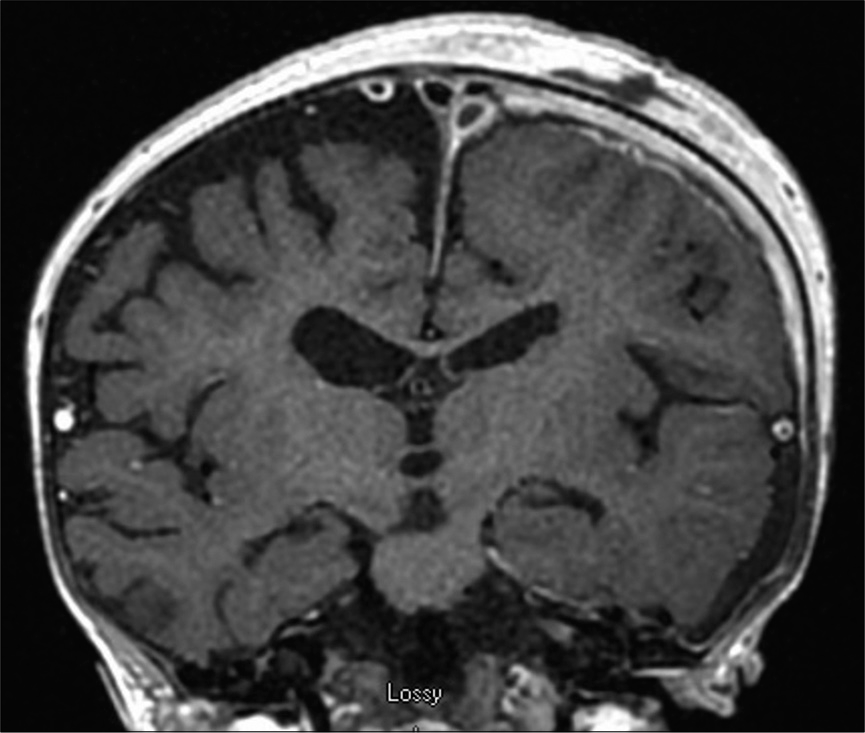
Background: Morganella morganii is a species of Gram-negative enteric rod found in normal human gut flora. Pathologically, this most often presents as urinary tract infections, wound infections, and bacteremia. It is highly uncommon for M. morganii to be implicated in a central nervous system infection, with only 12 reported cases of parenchymal abscesses or meningitis.
Case Description: A previously healthy 13-month-old female presented with fever of unknown origin and had a witnessed seizure during evaluation. A large left subdural fluid collection was identified, and the patient underwent emergent burr hole drainage and subdural drain placement. Cultures demonstrated M. morganii empyema, and she subsequently completed a course of directed antibiotics. Six months following surgery, she has no further clinical or radiographic evidence of infection, seizures, or neurological sequelae.
Conclusion: We describe the first reported case of isolated subdural empyema caused by M. morganii. The child was successfully treated with the evacuation of the empyema and direct antibiotics with no lasting neurological injury.
Keywords: Infection, Morganella morganii, Pediatric neurosurgery, Subdural empyema
INTRODUCTION
Subdural empyema (SE) is a pyogenic fluid collection that can result in rapid and significant cerebral compression, while rare, these infections represent neurosurgical emergencies.[
CASE DESCRIPTION
A 13-month-old female with no significant prior medical history, prior significant infections, or developmental concerns presented with worsening fatigue and intermittent fevers. The initial evaluation demonstrated leukocytosis, anemia, and elevated inflammatory markers. Infectious evaluation, including chest X-ray, monospot test, rapid streptococcal screen, HSV testing, and UA, was unremarkable. A viral etiology was considered most likely and the patient was discharged home with return precautions. Over the following week, the patient had no significant improvement, and she was admitted to the hospital for further evaluation after repeated laboratory investigations yielded similar results.
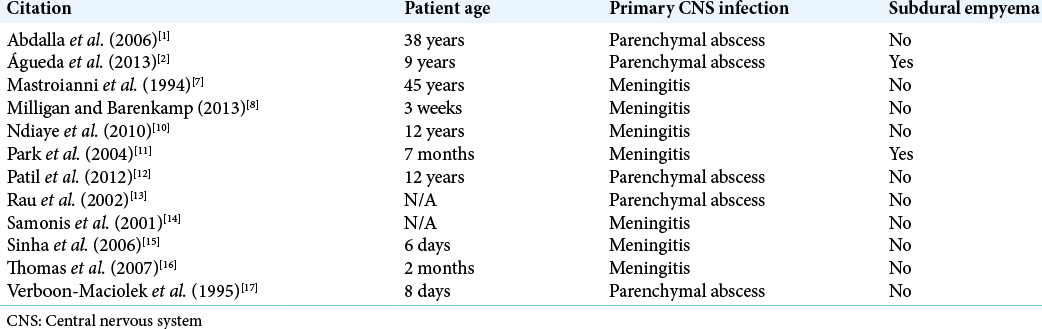
On admission, her symptoms included intermittent fevers with concurrent irritability, fatigue, and decreased solid food intake; she appeared at her baseline when not febrile. No signs or symptoms of localized infection were present at that time, and her family denied sick contacts. On the morning following admission, the patient experienced a right upper extremity focal seizure requiring prompting immediate brain MRI. MRI demonstrated an extensive left subdural fluid collection consistent with a subdural hematoma and associated left to right midline shift [
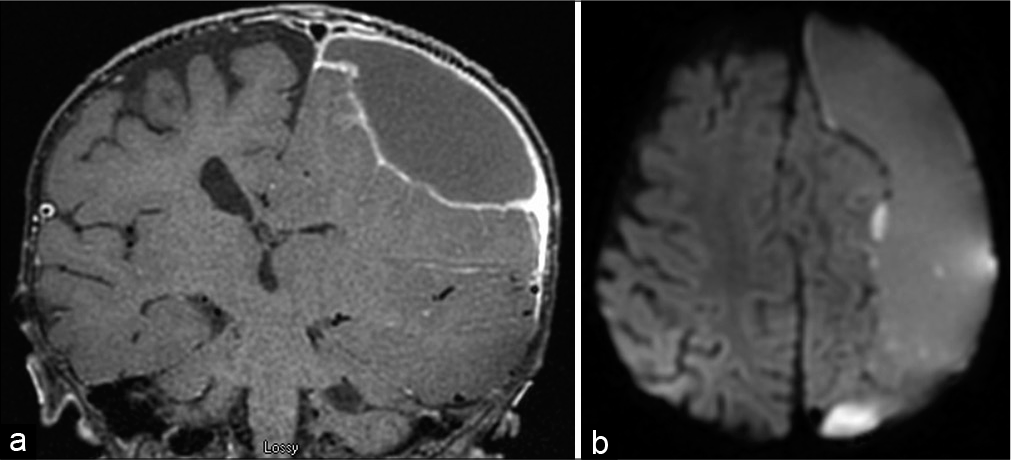
Given the concern for a chronic subdural hematoma, the patient underwent further trauma evaluation, including retinal examination, skeletal survey, skin examination, and spine MRI which were all unremarkable. MR angiogram showed no evidence of underlying high flow vascular abnormality. Further, history revealed potential trauma 2 weeks before the onset of symptoms, when the patient tipped over in a toy car onto cement; no other history of trauma was identified. Repeat imaging the day after surgery demonstrated near-complete decompression of the left hemisphere [
DISCUSSION
Morganella species is uncommon causes of disease in humans and is notably rare as intracranial pathogens. In a review of the literature, there are 12 prior reports of M. morganii intracranial infections, with all prior described cases being parenchymal abscesses or meningitis.[
While the underlying source for this infection remains unclear, the clinical and radiographic findings suggest a superimposed infection of a chronic subdural hematoma. Interestingly, blood is one of two agar media frequently used to culture Morganella species for diagnosis, with the other being MacConkey agar. Alternatively, given the novel presentation and uncertain premorbid trajectory, in this case, hemorrhagic expansion of the subdural space secondary to the infection itself remains possible. The etiology of this infection is even more obscured by the patient’s immunocompetence and lack of extracranial infection.
The patient, in this case, responded well to traditional management of the SE with emergent surgical drainage and directed antibiotic therapy. Surgical approaches to SEs typically favor craniotomy to ensure complete evacuation of the infection, though, in this patient, the homogenous fluid signal on imaging and intraoperative ultrasound confirmation of appropriate resolution allowed burr hole drainage.[
CONCLUSION
We describe the first reported case of isolated SE caused by M. morganii. In this patient, the infection possibly represented a superinfection of a chronic subdural hematoma. This case description adds to the minimal literature regarding M. morganii as a rare intracranial pathogen and reports a novel presentation of this pathogen with isolated SE.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abdalla J, Saad M, Samnani I, Lee P, Moorman J. Central nervous system infection caused by Morganella morganii. Am J Med Sci. 2006. 331: 44-7
2. Águeda S, Leitão A, Rocha G, Guimarães H. Cerebral abscess and empyema due to Morganella morganii. Pediatr Ther. 2013. 3: 147
3. Gupta S, Vachhrajani S, Kulkarni AV, Taylor MD, Dirks P, Drake JM. Neurosurgical management of extraaxial central nervous system infections in children. J Neurosurg Pediatr. 2011. 7: 441-51
4. Jim KK, Brouwer MC, van der Ende A, van de Beek D. Subdural empyema in bacterial meningitis. Neurology. 2012. 79: 2133-9
5. Konar S, Gohil D, Shukla D, Sadashiva N, Uppar A, Bhat DI. Predictors of outcome of subdural empyema in children. Neurosurg Focus. 2019. 47: E17
6. Liu H, Zhu J, Hu Q, Rao X. Morganella morganii a non-negligent opportunistic pathogen. Int J Infect Dis. 2016. 50: 10-7
7. Mastroianni A, Coronado O, Chiodo F. Morganella morganii meningitis in a patient with AIDS. J Infect. 1994. 29: 356-7
8. Milligan KL, Barenkamp SJ. Neonatal meningitis due to Morganella morganii. Clin Pediatr (Phila). 2013. 52: 462-4
9. Muzumdar D, Biyani N, Deopujari C. Subdural empyema in children. Childs Nerv Syst. 2018. 34: 1881-7
10. Ndiaye M, Sène MS, Sow AD, Seck LB, Coulibaly T, Diagne NS. Meningoencephalitis due to Morganella morganii A case report. Bull Soc Pathol Exot. 2010. 103: 230-2
11. Park EY, Lee SJ, Oh PS, Kim KN, Moon SM. A case of subdural abscess caused by Morganella morganii. Clin Exp Pediatr. 2004. 47: 1024-7
12. Patil AB, Nadagir SD, Lakshminarayana S, Syeda FM. Morganella morganii subspecies morganii, biogroup a: An unusual causative pathogen of brain abscess. J Neurosci Rural Pract. 2012. 3: 370-2
13. Rau CS, Chang WN, Lin YC, Lu CH, Liliang PC, Su TM. Brain abscess caused by aerobic Gram-negative Bacilli Clinical features and therapeutic outcomes. Clin Neurol Neurosurg. 2002. 105: 60-5
14. Samonis G, Anatoliotaki M, Apostolakou H, Souglakos J, Georgoulias V. Fatal septicemia and meningitis due to Morganella morganii in a patient with Hodgkin’s disease. Scand J Infect Dis. 2001. 33: 553-5
15. Sinha AK, Kempley ST, Price E, Sharma BK, Livermore DM. Early onset Morganella morganii sepsis in a newborn infant with emergence of cephalosporin resistance caused by depression of AMPC beta-lactamase production. Pediatr Infect Dis J. 2006. 25: 376-7
16. Thomas VA, Sathish KT, Agarwal I, Chacko AG. Unusual cause of brain abscess in an infant. J Pediatr Neurosci. 2007. 2: 94-5
17. Verboon-Maciolek M, Vandertop WP, Peters AC, Roord JJ, Geelen SP. Neonatal brain abscess caused by Morganella morgagni. Clin Infect Dis. 1995. 20: 471