- Department of Neurosurgery, Puerta de Hierro University Hospital, Madrid, Spain.
- Department of Surgery, Puerta de Hierro University Hospital, Madrid, Spain.
Correspondence Address:
Ruth Prieto
Department of Surgery, Puerta de Hierro University Hospital, Madrid, Spain.
DOI:10.25259/SNI_620_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ruth Prieto1, Matias Cea Soriano2, Celia Ortega1, Teresa Kalantari1, Alberto Pueyo Rabanal2. Subdural fluid accumulation caused by ventriculoperitoneal shunt underdrainage: A rare and paradoxical complication. 22-Dec-2020;11:451
How to cite this URL: Ruth Prieto1, Matias Cea Soriano2, Celia Ortega1, Teresa Kalantari1, Alberto Pueyo Rabanal2. Subdural fluid accumulation caused by ventriculoperitoneal shunt underdrainage: A rare and paradoxical complication. 22-Dec-2020;11:451. Available from: https://surgicalneurologyint.com/surgicalint-articles/10475/
Abstract
Background: Subdural fluid collection in patients with internal cerebrospinal fluid (CSF) shunts has generally been linked to overdrainage and more rarely to pus accumulation. The authors present a previously unrecognized condition leading to extra-axial CSF accumulation: shunt underdrainage. Treatment of coexisting subdural fluid collection and hydrocephalus, disorders that have previously only been reported concurrently following head trauma or subarachnoid hemorrhage, is controversial. In addition, we intend to provide insight into the physiopathology of abnormal CSF accumulation within both the subdural space and ventricles simultaneously.
Case Description: A 42-year-old female with a history of hypothalamic glioma and obstructive hydrocephalus during childhood presented with headache, vomiting, and gait disturbance. Following the insertion of her first ventriculoperitoneal shunt (VPS) by the age of 8, she underwent several surgeries due to shunt failure, all of them associating ventriculomegaly. Ventricles remained notably enlarged following insertion of her most recent VPS, and the computed tomography scan performed 2 months later at her admission showed a large subdural collection. Afterward, a malpositioned distal catheter causing shunt blockage was confirmed. Both, the subdural accumulation and hydrocephalus, were resolved following adequate placement of the peritoneal catheter.
Conclusion: This case demonstrates that subdural fluid accumulations may occur following VPS underdrainage with hydrocephalus. Development of such extra-axial collection was probably caused by pressure related to CSF spillage from the ventricles into the subdural space. Our case also supports that a mass-effect subdural accumulation with hydrocephalus can be satisfactorily treated with adequate VPS alone, without directly treating the subdural collection.
Keywords: Cerebrospinal fluid, External hydrocephalus, Shunt malfunction, Subdural accumulation, Ventriculoperitoneal shunt
INTRODUCTION
Subdural fluid accumulation in patients carrying artificial diversion systems generally corresponds to the abnormal collection of cerebrospinal fluid (CSF) in the subdural space secondary to shunt overdrainage and exceptionally to subdural empyema.[
We present the first case report of VPS malfunction secondary to malposition of the distal catheter in a patient presenting with concomitant hydrocephalus and a large subdural accumulation. The underlying physiopathology and surgical strategy implemented are also discussed.
CASE DESCRIPTION
We present a 42-year-old female with a history of hypothalamic glioma and resultant obstructive hydrocephalus that had been subjected to multiple surgeries since her childhood due to CSF shunt malfunction. Following her last VPS implantation, symptoms of high intracranial pressure (ICP) notably improved but ventricle enlargement remained almost unchanged on computed tomography (CT) [
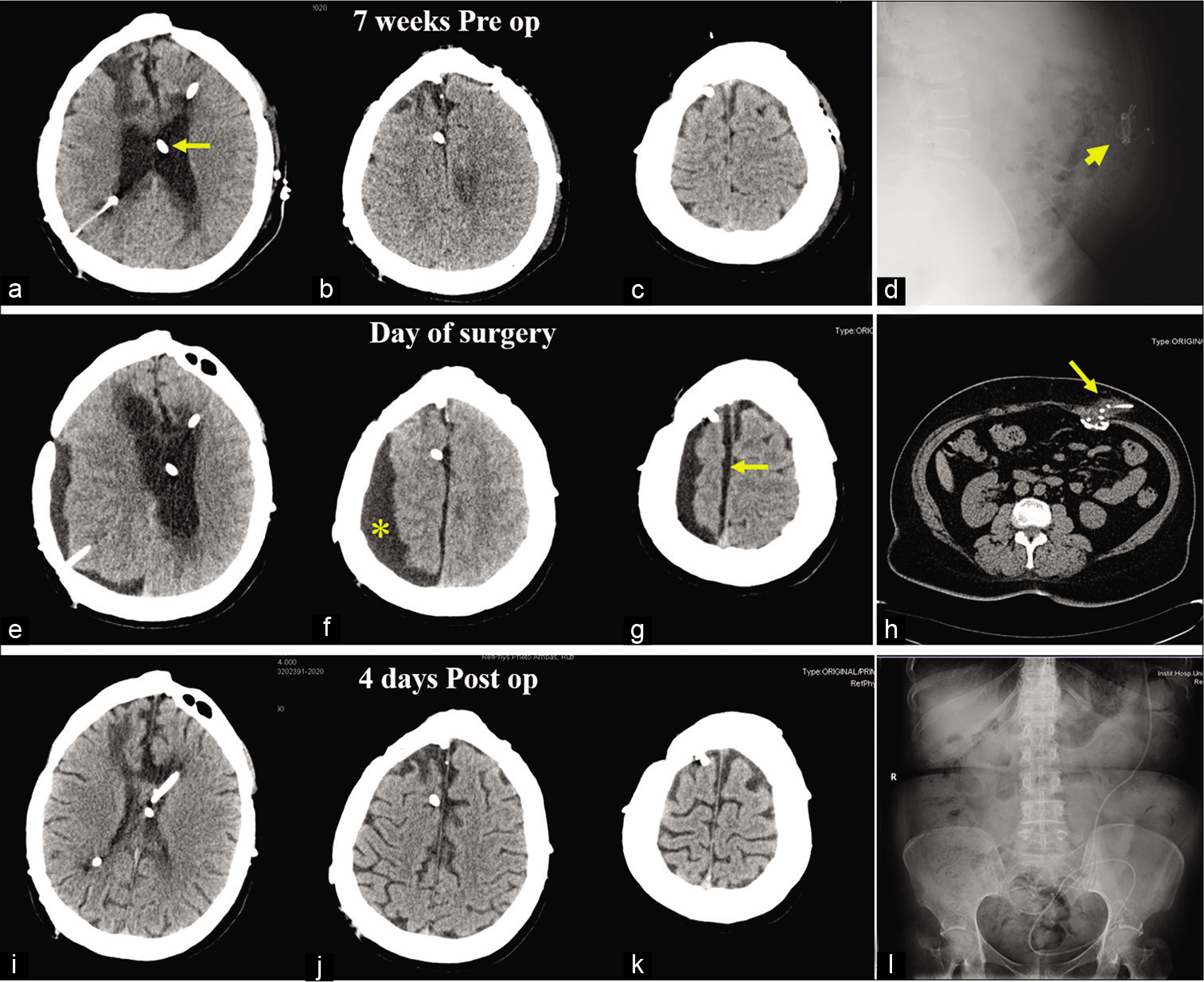
Figure 1:
Preoperative and postoperative radiological studies. (a-c) Axial head computed tomography (CT) images obtained 7 weeks before current admission, that is, 1 week after placement of the latest ventriculoperitoneal shunt (VPS) (arrow), show persistence of hydrocephalus. (d) Lateral abdominal X-ray showing a coiled distal catheter (head arrow). (e-g) Head scan performed at admission demonstrating enlargement of the ventricular system in addition to a large extra-axial low-density collection over the right hemisphere (asterisk) with underlying effaced sulci and a minor subdural interhemispheric component (arrow). (h) Abdominal CT scan displaying multiple loops of the distal end of the VPS at the abdominal wall (arrow). (i-k) Postoperative CT scan performed after 4 days after intraperitoneal repositioning of the distal catheter demonstrates complete resolution of both hydrocephalus and the subdural collection. (l) Postoperative X-ray confirms correct intra-abdominal position of the VPS.
In the present admission, 2 months after the latest VPS placement, the patient complained of severe headache, vomiting, and gait disturbance. An urgent cranial CT demonstrated hydrocephalus in addition to a large low-density subdural collection over the right hemisphere with a minor right interhemispheric component [
The paradox of finding a subdural accumulation (typically associated with VPS overdrainage) and hydrocephalus in a patient with distal VPS malposition generated perplexity and uncertainty for us regarding the most appropriate surgical strategy. Draining the subdural accumulation was considered in addition to repositioning the peritoneal catheter. Nevertheless, the delayed development of the subdural collection following several weeks of hydrocephalus in a patient with shunt malfunction led us to consider that both abnormal fluid accumulations might be related to the blocked CSF flow. Thus, we finally recommended VPS revision alone. We first performed a minilaparotomy, which revealed a pseudocyst encompassing the distal end of the catheter. Once adequate CSF outflow was verified, the fibrous capsule was partially resected, and the catheter repositioned intraperitoneally. Following surgery, all symptoms resolved, and postoperative CT performed on day 4 showed resolution of both hydrocephalus and subdural CSF accumulation [
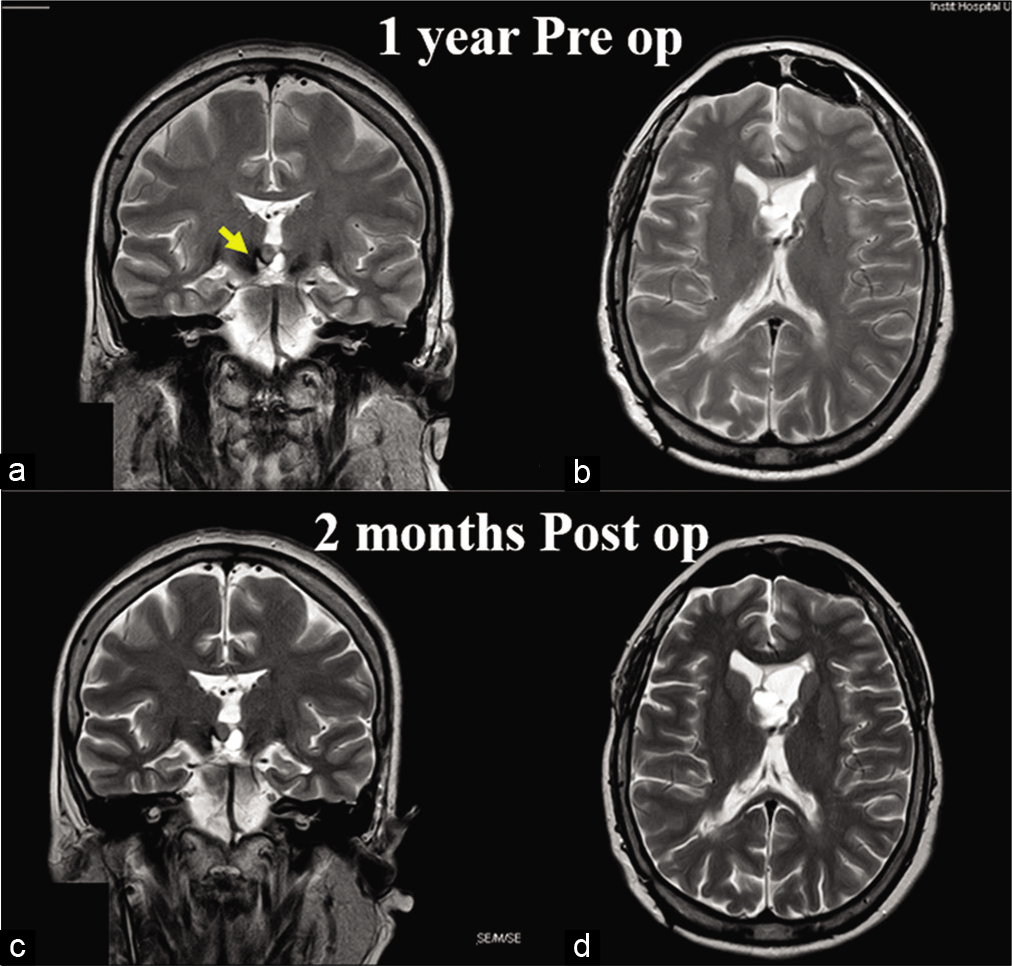
Figure 2:
Preoperative and postoperative magnetic resonance imaging studies. (a and b) T2-weighted MR images obtained 1 year before current admission (at a time with adequate functioning of her internal cerebrospinal fluid diversion system). Note the tumor occupying the third ventricle (arrow). (c and d) Images obtained 2 months after correct placement of the distal catheter demonstrates recovery of previous ventricular size and lack of subdural accumulation.
We wish to highlight both the time frame of the development and resolution of the subdural accumulation, as well as the successful surgical strategy chosen. CSF accumulation occurred in a delayed fashion following several weeks of ventriculomegaly, and it was completely resolved by the 4th postoperative day after only VPS revision, which points to a shift of excessive CSF from the ventricles to the subdural compartment as the underlying mechanism for subdural fluid accumulation in our patient.
DISCUSSION
Malfunction of CSF shunting devices is still a common and challenging problem in neurosurgery.[
Treatment strategy of concomitant hydrocephalus and subdural CSF accumulations
The preferred treatment strategy for mass effect subdural collections associated with hydrocephalus has been through two different surgical stages, each one directed at each type of abnormal CSF accumulation. Initial surgical procedures are usually focused on subdural surgical drainage, either through subdural-peritoneal shunts or single burr holes. In a later stage, after the mass effect of the extra-axial collection has been solved, treatment is focused on ventricular dilatation, usually with VPS placement.[
An increasing number of neurosurgeons advocate VPS as a sole surgical procedure in patients with concomitant hydrocephalus and subdural CSF accumulation. Some reports demonstrating successful resolution of hydrocephalus and subdural collections, either related to SAH,[
Physiopathology underlying abnormal CSF accumulation within the ventricular and subdural cavities
Development of subdural fluid collections in patients with concomitant hydrocephalus following SAH or head trauma has been related to a communication between the ventricles and the subdural space, either through traumatic arachnoid tearing or surgical violation of parachiasmatic/Liliequist membranes.[
Nonetheless, in the case that we report, enlargement of the ventricles preceded the development of the subdural collection. Extra-axial CSF accumulation was probably related to a low resistance transparechymal path between the ventricles (where CSF was accumulated at a high pressure due to VPS blockage) and the subdural space (a low-pressure compartment). Such a path could be either the surgical transfrontal route used to approach the tumor or along the old parietal ventricular catheter, both of which associate surgical violation of the arachnoid membranes. Moreover, recent studies have described a new mechanism involved in physiological CSF drainage along Virchow-Robin perivascular spaces toward meningeal and cervical lymphatic vessels. This glymphatic CSF drainage seems to predominate in patients with hydrocephalus.[
Complete resolution of the subdural collection once the VPS in our patient recovered normal functioning supports that communication between the ventricles and the subdural space is two way and unobstructed. Finally, its rapid disappearance within only 4 days of VPS revision is probably related to the elasticity of a young brain.
CONCLUSION
To the best of our knowledge, this is the first case report documenting a subdural fluid collection coexisting with hydrocephalus secondary to CSF shunt underdrainage. Satisfactory clinical course with complete resolution of both subdural CSF accumulation and hydrocephalus following a single surgery aimed at fixing shunt malposition supports that such an extra-axial collection was secondary to pressure-related CSF spillage from the ventricles into the subdural space. Awareness of this rare and paradoxical type of VPS malfunction is essential to expedite accuracy in diagnosis and provide adequate treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We wish to express our gratitude to Ana Puerto and Cristina Escudero, librarians of Puerta de Hierro University Hospital (Madrid, Spain) for their kind assistance during the process of retrieving some of the original articles used in this study. We are also grateful to George Hamilton for his critical review of the language and style of the manuscript.
References
1. Akins PT, Guppy KH. Are hygromas and hydrocephalus after decompressive craniectomy caused by impaired brain pulsatility, cerebrospinal fluid hydrodynamics, and glymphatic drainage? Literature overview and illustrative cases. World Neurosurg. 2019. 130: e941-52
2. Broggi M, Zattra CM, Schiariti M, Acerbi F, Tringali G, Falco J. Diagnosis of ventriculoperitoneal shunt malfunction: A practical algorithm. World Neurosurg. 2020. 137: e478-86
3. Cardoso ER, Shubert R. External hydrocephalus in adults. Report of three cases. J Neurosurg. 1996. 85: 1143-7
4. Escosa-Bagé M, Sola RG. Physiopathology of adult onset external hydrocephalus. Rev Neurol. 2002. 35: 141-4
5. Feletti A, d’Avella D, Wikkelsø C, Klinge P, Hellström P, Tans J. Ventriculoperitoneal shunt complications in the European idiopathic normal pressure hydrocephalus multicenter study. Oper Neurosurg (Hagerstown). 2019. 17: 97-102
6. Huh PW, Yoo DS, Cho KS, Park CK, Kang SG, Park YS. Diagnostic method for differentiating external hydrocephalus from simple subdural hygroma. J Neurosurg. 2006. 105: 65-70
7. Kawaguchi T, Fujita S, Hosoda K, Shibata Y, Komatsu H, Tamaki N. Treatment of subdural effusion with hydrocephalus after ruptured intracranial aneurysm clipping. Neurosurgery. 1998. 43: 1033-8
8. Naffziger HC. Subdural fluid accumulation following head injury. J Am Med Assoc. 1924. 82: 1751-2
9. Samuelson S, Long DM, Chou SN. Subdural hematoma as a complication of shunting procedures for normal pressure hydrocephalus. J Neurosurg. 1972. 37: 548-51
10. Tsuang FY, Huang AP, Tsai HY, Chen JY, Lee JE, Lu YK. Treatment of patients with traumatic subdural effusion and concomitant hydrocephalus. J Neurosurg. 2012. 116: 558-65
11. Tzerakis N, Orphanides G, Antoniou E, Sioutos PJ, Lafazanos S, Seretis A. Subdural effusion with hydrocephalus after severe head injury: Successful treatment with ventriculoperitoneal shunt placement: Report of 3 adult cases. Case Rep Med. 2010. 2010: 743784
12. Weller RO, Djuanda E, You HY, Carare RO. Lymphatic drainage of the brain and the pathophysiology of neurological disease. Acta Neuropathol. 2009. 117: 1-14
13. Wu R, Ye Y, Ma T, Jia G, Qin H. Management of subdural effusion and hydrocephalus following decompressive craniectomy for posttraumatic cerebral infarction in a patient with traumatic brain injury: A case report. BMC Surg. 2019. 19: 26
14. Yoshimoto Y, Wakai S, Hamano M. External hydrocephalus after aneurysm surgery: Paradoxical response to ventricular shunting. J Neurosurg. 1998. 88: 485-9
15. Zanini MA, de Lima Resende LA, de Souza FA, Gabarra RC. Traumatic subdural hygromas: Proposed pathogenesis based classification. J Trauma. 2008. 64: 705-13