- Department of Neurosurgery, Avicenne Military Hospital of Marrakech, Marrakech and Mohammed V University, Rabat, Morocco
- Department of Neurosurgery, State University of New York (SUNY), Upstate Medical University, Syracuse, New York, United States
DOI:10.25259/SNI-31-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ali Akhaddar, Walter Hall, Mohammed Boucetta. Subgaleal and brain abscesses due to Salmonella enteritidis following craniotomy for giant cell glioblastoma multiforme: A case report and literature review. 26-Mar-2019;10:37
How to cite this URL: Ali Akhaddar, Walter Hall, Mohammed Boucetta. Subgaleal and brain abscesses due to Salmonella enteritidis following craniotomy for giant cell glioblastoma multiforme: A case report and literature review. 26-Mar-2019;10:37. Available from: https://surgicalneurologyint.com/surgicalint-articles/9247/
Abstract
Background: Cranial surgical site infections due to Salmonella species are rarely reported. Only eight cases of Salmonella enteritidis infection following intracranial surgery for brain tumor have been reported to date. We describe a unique case of both subgaleal and brain abscesses caused by S. enteritidis following craniotomy for a parafalcine giant cell glioblastoma multiforme. A literature review of the previously published cases is also provided.
Case Description: A 36-year-old previously healthy man presented with a posterior parietal parafalcine giant cell glioblastoma multiforme. 5 weeks after craniotomy for tumor resection, the patient presented with worsening headache and painful swelling at the cranial operative site. Head computed tomography and magnetic resonance imaging scans revealed both scalp and brain abscesses in the previous surgical site. He was treated with aspiration of the subgaleal abscess and ciprofloxacin antibiotic therapy; he made a full recovery. Cultures of the aspirate identified S. enteritidis, although the primary site of infection was not detected.
Conclusions: Although postoperative S. enteritidis infections are rare, the large numbers of patients with malignant brain tumors who require tumor resections and receive corticosteroids are at great risk. Adequate drainage (if possible), early isolation of the pathogens, and control of the infection by antibiotic therapy guided by antimicrobial susceptibility testing are vital components to prevent this potentially fatal condition.
Keywords: Brain abscess, complication, giant cell glioblastoma multiforme, infection, Salmonella enteritidis, Salmonella infection, scalp abscess, surgical site infection
INTRODUCTION
Central nervous system (CNS) infections due to Salmonella species are uncommon.[
CASE DESCRIPTION
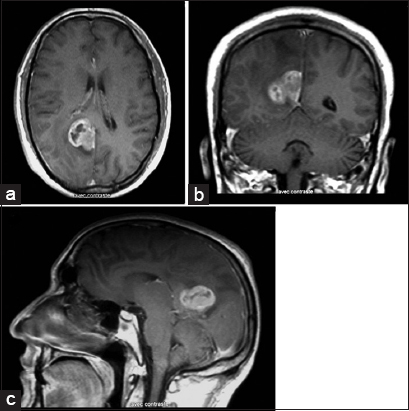
A 36-year-old man with no significant medical history, presented to our medical center with headache, nausea, episodic seizures, and personality changes for 1 month. He was afebrile, had no focal neurologic deficits, and had no systemic abnormalities on clinical examination. Magnetic resonance imaging (MRI) of the head revealed a 3-cm diameter right posterior parietal parafalcine, dura based, enhancing lesion, suggesting an extra-axial tumor [
Figure 1
Following gadolinium injection, axial. (a) Coronal. (b) And sagittal. (c) Sections of T1-weighted magnetic resonance imaging demonstrating the parafalcine tumor localized in the right posterior parietal region before the first operation. Note the close spatial relationship of the tumor to the falx cerebri.
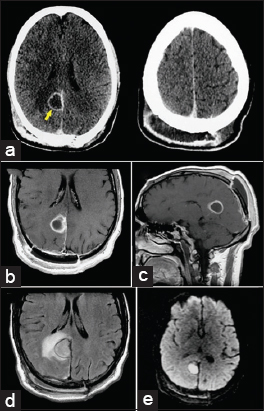
5 weeks after surgery, the patient presented with worsening headache and painful swelling at the cranial operative site. Head computed tomography (CT) scan demonstrated a subgaleal extracranial homogenous low-density lesion with rim enhancement following contrast administration. There was also another intracranial ring-enhancing collection at the glioblastoma resection cavity, suggesting a brain abscess [
Figure 2
Postoperative axial computed tomography following contrast administration. (a) Revealing a subgaleal extracranial homogenous low-density lesion with rim enhancement (right). There was also another intracranial ring-enhancing collection at the site of the tumor resection cavity (left), suggesting a brain abscess (arrow). Postoperative magnetic resonance imaging showing both extracranial and parafalcine cystic masses with homogenous, low-intensity signal on T1-weighted images. (b and c) And high-intensity signal on the fluid-attenuated inversion recovery sequence. (d) There was peripheral enhancement after gadolinium injection (b and c) and significant cerebral edema surrounding the resection cavity. (d) Note the restricted diffusion-weighted image (bright signal) of the extracranial and parafalcine collections (e).
DISCUSSION
Salmonellosis is usually a self-limited disease that generally causes gastrointestinal tract infection in humans through the oral route. Extraintestinal infections are uncommon, especially in the CNS, and may remain undetected due to a lack of fever and gastroenteritis.[
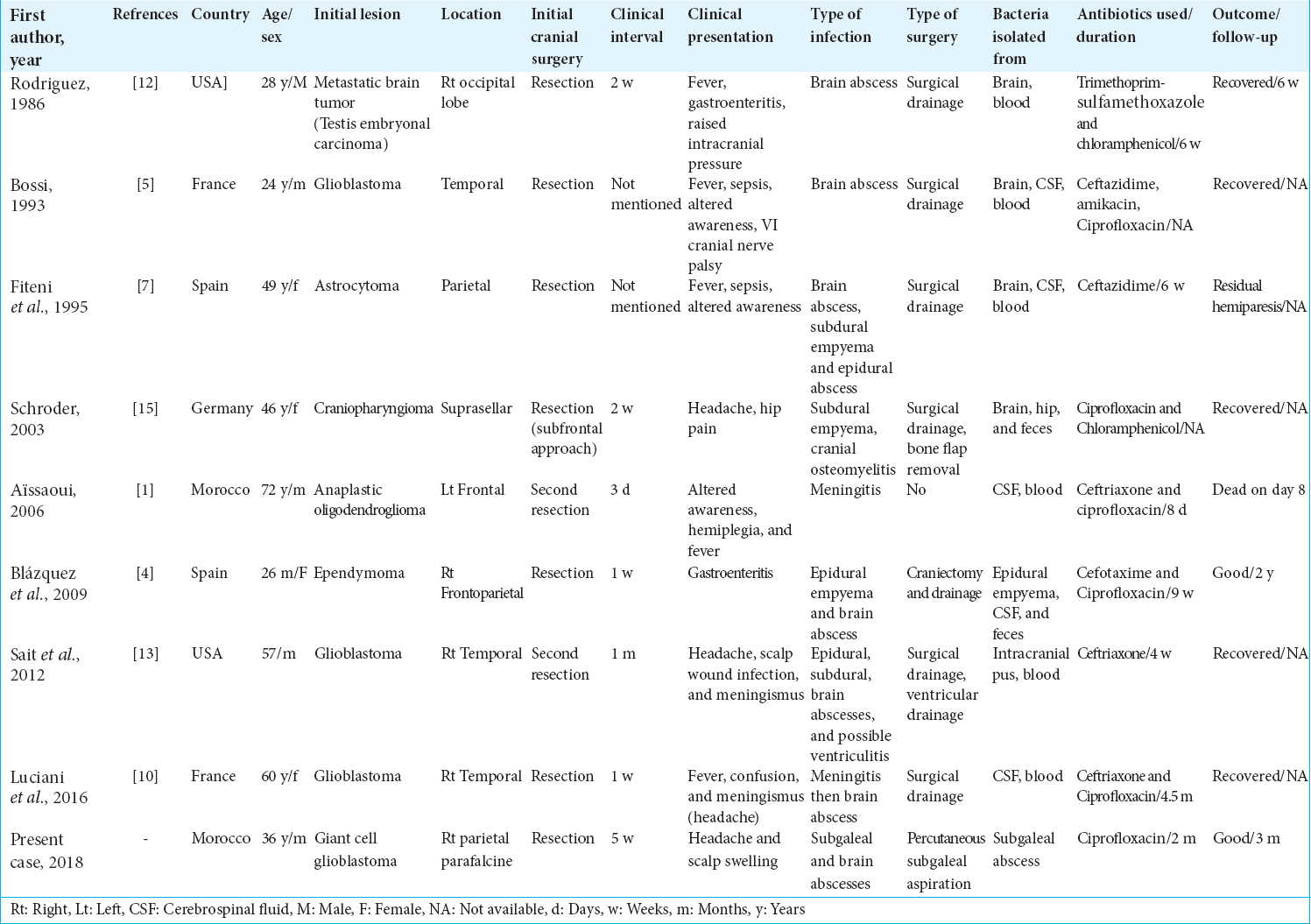
All patients had a cranial surgical site infection (SSI). In addition, two cases also had gastroenteritis and one patient had concomitant infectious arthritis of the hip. The organism was identified from samples of the cranial SSI in all patients and also from samples outside the SSI in eight cases (six from blood cultures and two from stool cultures). The most common predisposing factors to infection were corticosteroid use and malignancy, but no patient was seropositive for HIV infection.
The clinical features of these patients did not differ from those with SSI caused by other bacteria.[
Adequate drainage (if possible), early isolation of the pathogens, and control of the infection by antibiotic therapy guided by antimicrobial susceptibility testing are essential to prevent this potentially fatal condition.[
Among the few cases of reported S. enteritidis infection following craniotomy in literature, this is the first case of the simultaneous occurrence of brain abscess and extracranial scalp abscess. The ability of these bacteria to produce a cranial SSI remains unexplained. Although the origin of infection was unclear in our previously healthy patient, the course of corticosteroids that he received and the original malignant intracranial tumor could have predisposed him to infection followed by potential hematogenous spread to the cranial surgical site. Furthermore, the absence of underlying systemic disease seems to be crucial for the cure of our patient. Finally, the possibility of postoperative Salmonella infection should be considered in patients with malignant brain tumor having surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aissaoui Y, Azendour H, Balkhi H, Haimeur C, Atmani M. Postoperative meningitis caused by an unusual etiological agent Salmonella enteritidis. Neurochirurgie. 2006. 52: 547-50
2. Akhaddar A, Zalagh M, Gazzaz M, Boucetta M. Brain abscess as a complication of intranasal ethmoidectomy for sinonasal polyposis. Surg Infect (Larchmt). 2010. 11: 483-5
3. Akhaddar A, Akhaddar A.editors. Surgical site infections in cranial surgery. Atlas of Infections in Neurosurgery and Spinal surgery. Switzerland: Springer International Publishing; 2017. p. 191-215
4. Blázquez D, Muñoz M, Gil C, Ruibal JL, El Knaichi F, Aleo E. Brain abscess and epidural empyema caused by Salmonella enteritidis in a child: Successful treatment with ciprofloxacin: A case report. Cases J. 2009. 2: 7131-
5. Bossi P, Mion G, Brinquin L, Bonsignour JP. Postoperative brain abscess caused by Salmonella enteritidis. Presse Med. 1993. 22: 130-
6. Diebold P, Humbert J, Djientcheu Vde P, Gudinchet F, Rilliet B. Salmonella epidural abscess in sickle cell disease: Failure of the nonsurgical treatment. J Natl Med Assoc. 2003. 95: 1095-1098
7. Fiteni I, Ruiz FJ, Crusells MJ, Sanjoaquin I, Guillen G. Salmonella enteritidis multifocal infection of the central nervous system. Efficacy of new cephalosporins. Presse Med. 1995. 24: 309-11
8. Hanel RA, Araújo JC, Antoniuk A, da Silva Ditzel LF, Flenik Martins LT, Linhares MN. Multiple brain abscesses caused by Salmonella typhi : Case report. Surg Neurol. 2000. 53: 86-90
9. Lloret MD, Escudero JR, Hospedales J, Viver E. Mycotic aneurysm of the carotid artery due to Salmonella enteritidis associated with multiple brain abscesses. Eur J Vasc Endovasc Surg. 1996. 12: 250-2
10. Luciani L, Dubourg G, Graillon T, Honnorat E, Lepidi H, Drancourt M. Salmonella enterica serovar enteritidis brain abscess mimicking meningitis after surgery for glioblastoma multiforme: A case report and review of the literature. J Med Case Rep. 2016. 10: 192-
11. Millward CP, McMullan NK, Vaiude P, da Rosa SP, Riordan A, Burn SC. Extradural abscess secondary to Salmonella enteritidis in a child following fronto-orbital facial advancement and remodeling surgery. J Craniofac Surg. 2014. 25: 489-91
12. Noguerado A, Cabanyes J, Vivancos J, Navarro E, Lopez F, Isasia T. Abscess caused by Salmonella enteritidis within a glioblastoma multiforme. J Infect. 1987. 15: 61-3
13. Rodriguez RE, Valero V, Watanakunakorn C. Salmonella focal intracranial infections: Review of the world literature (1884-1984) and report of an unusual case. Rev Infect Dis. 1986. 8: 31-41
14. Sait M, Rahmathulla G, Chen TL, Barnett GH. Rare case of intracranial Salmonella enteritidis abscess following glioblastoma resection: Case report and review of the literature. Surg Neurol Int. 2011. 2: 149-
15. Sarria JC, Vidal AM, Kimbrough RC. Salmonella enteritidis brain abscess: Case report and review. Clin Neurol Neurosurg. 2000. 102: 236-9
16. Schröder J, Palkovic S, Kipp F, Wassmann H. Salmonella enteritidis causing brain abscess and coxitis following intracranial surgery. Acta Neurochir (Wien). 2003. 145: 919-21