- Department of Neurosurgery, Helsinki University Central Hospital, Helsinki, Finland
- Department of Neurosurgery, Umberto I General Hospital, Università Politecnica delle Marche, Ancona, Italy
Correspondence Address:
Joham Choque-Velasquez
Department of Neurosurgery, Helsinki University Central Hospital, Helsinki, Finland
DOI:10.4103/sni.sni_444_16
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Joham Choque-Velasquez, Roberto Colasanti, Anna Piippo, Mika Niemelä. Suboccipital osteoblastoma: Microsurgical resection of a rare entity. 14-Mar-2017;8:33
How to cite this URL: Joham Choque-Velasquez, Roberto Colasanti, Anna Piippo, Mika Niemelä. Suboccipital osteoblastoma: Microsurgical resection of a rare entity. 14-Mar-2017;8:33. Available from: http://surgicalneurologyint.com/?post_type=surgicalint_articles&p=8314
Abstract
Background:Osteoblastomas are rare lesions comprising 1% of all bone tumors. The occipital bone is one of the rarest affected bone, with only 11 cases reported during the last 40 years.
Case Description:Here, we describe the clinical presentation and the radiological features of a suboccipital osteoblastoma that was successfully resected in a 30-year-old man. A short video shows the microsurgical removal of the lesion. There was no recurrence during a 12-month follow-up.
Conclusions:Even if osteoblastomas are benign tumors, a complete removal has to be achieved to reduce the risk of recurrences. This makes necessary an appropriate monitoring of the patient.
Keywords: Occipital bone, osteoblastoma, park bench position, suboccipital approach
INTRODUCTION
Osteoblastomas are rare lesions comprising 1% of all bone tumors. Skull bones are affected in only approximately 3% of the cases, and the occipital bone is far less involved than facial, temporal, frontal, and skull base bones.[
CASE REPORT
A 30-year-old man, without significant medical history, was admitted to our department for a painful left occipitocervical swelling, progressively worsening over the past several months. A physical examination revealed an occipital hard mass covered by the normal skin, without any neurological deficit.
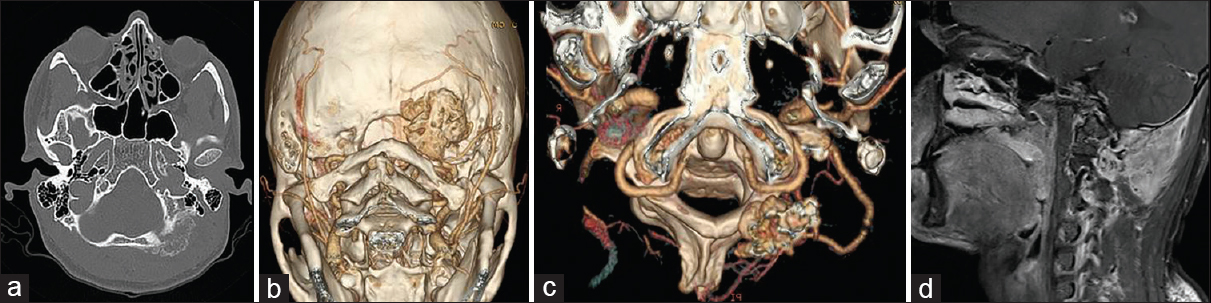
A computerized tomography (CT) scan showed an osteolytic lesion inside the diploic space surrounded by sclerotic tissue expanded to the left squamous portion of the occipital bone around the foramen magnum. In addition, the CT angiography with three-dimensional (3D) reconstruction revealed a close relation between the tumor and the vertebral and occipital arteries [
Figure 1
Preoperative images. (a) Axial CT scan showing a left osteolytic occipital lesion surrounded by sclerotic tissue extended inferiorly up to the foramen magnum. (b and c) 3D reconstructions of the CT angiogram illustrating the close relationship between the tumor and the vertebral and occipital arteries. (d) Sagittal post-contrast T1-weighted MRI scan revealing an avidly enhancing occipital extra-axial mass
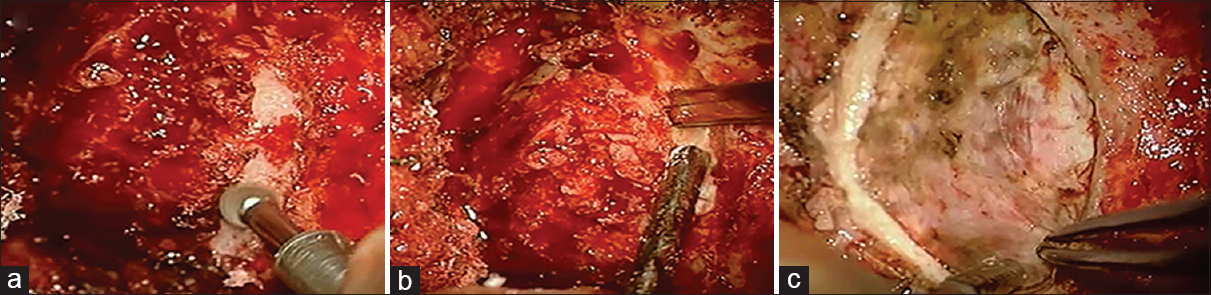
The patient underwent a left suboccipital approach in the park bench position. After the dissection of the soft tissues, the lesion was targeted according to anatomic landmarks. Under the operating microscope, the tumor was progressively removed, using high speed drills and rongeurs, up to the normal dura and surrounding normal bone. However, the left occipital condyle was left undisturbed [
Figure 2
Intraoperative photographs. (a) Initial removal of the lesion with a high speed drill. (b) Removal of the lesion using a kerrison rongeur, once the dura is reached, in order to prevent inadvertent dural lacerations. (c) Surgical field at the end of the resection with the surrounding normal bone
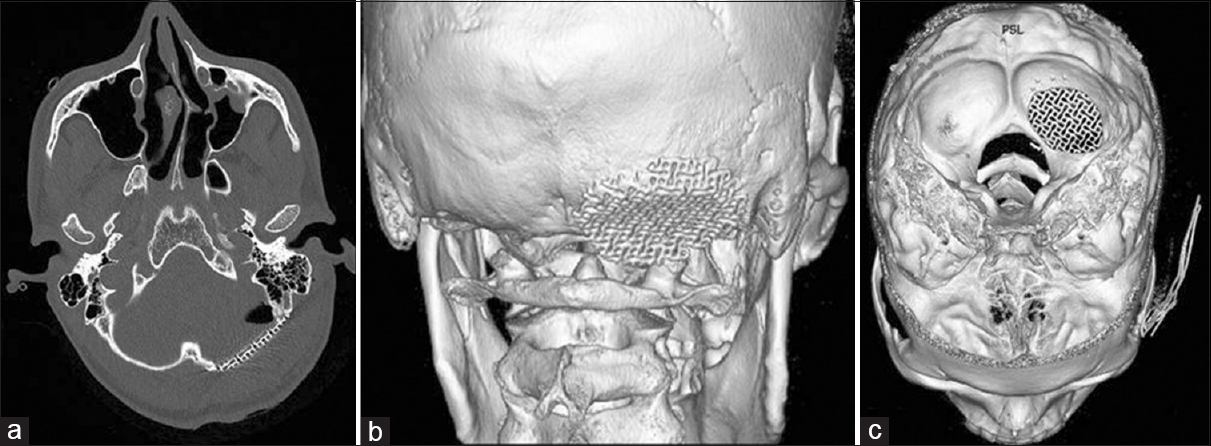
The postoperative course was uneventful, and the patient's symptoms disappeared. The histopathological examination was consistent with benign osteoblastoma, and the postoperative CT scan showed the complete resection of the lesion [
DISCUSSION
Osteoblastomas comprise 1% of all bone tumors. Skull bones are affected in only 3% of the cases, and occipital osteoblastomas are even rarer. To the best of our knowledge, this is the 12th case reported in the last 40 years.[
The presentation of the tumor is more frequent in men less than 30 years old; calvarian osteoblastomas essentially share the same characteristics of the osteoblastomas in other locations,[
Occipital osteoblastomas present as circumscribed expansive intraosseous lesions between the inner and outer table of the occipital bone, with lytic and sclerotic appearance in plain radiographs and CT scans.[
Even though giant osteoid osteomas are reported, unlike osteoblastomas,[
The recurrence of osteoblastomas after surgery is approximately 9.8–15%.[
In summary, occipital osteoblastomas are extreme rare benign bone tumors with typical histological features, sometimes hypervascularized, and with a high tendency to recur when they are not completely resected. At times, their treatment may require presurgical embolization, occipitocervical fusion, and/or transposition of the vertebral artery. Their high risk of recurrence makes necessary an appropriate monitoring of the patient.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Video Available on: www.surgicalneurologyint.com
References
1. Akhaddar A, Gazzaz M, Rimani M, Mostarchid B, Labraimi A, Boucetta M. Benign fronto-orbital osteoblastoma arising from the orbital roof: Case report and literature review.Surg. Neurol. 2004. 61: 391-7
2. Alli A, Johnson P, Reeves A. Imaging characteristics of occipital bone osteoblastoma. Case Rep Radiol 2013. 2013. p. 930623-
3. Bruneau M, Polivka M, Cornelius JF, George B. Progression of an osteoid osteoma to an osteoblastoma. Case report. J Neurosurg Spine. 2005. 3: 238-41
4. Erten F, Hasturk AE, Pak I, Sokmen O. Giant occipital osteoid osteoma mimicking calcified meningioma. Neurosciences. 2011. 16: 363-5
5. Han X, Dong Y, Sun K, Lu Y. A huge occipital osteoblastoma accompanied with aneurysmal bone cyst in the posterior cranial fossa. Clin Neurol Neurosurg. 2008. 110: 282-5
6. Hernesniemi J, Niemelä M, Karatas A, Kivipelto L, Ishii K, Rinne J. Some collected principles of microneurosurgery: Simple and fast, while preserving normal anatomy: A review. Surg Neurol. 2005. 64: 195-200
7. Jackson RP. Recurrent osteoblastoma: A review. Clin Orthop. 1978. 131: 229-33
8. Lot G, George B. The extent of drilling in lateral approaches to the cranio-cervical junction area from a series of 125 cases. Acta Neurochir. 1999. 141: 111-8
9. Low Y, Foo CL, Seow WT. Childhood temporal bone osteoblastoma: A case report. J. Pediatr Surg. 2000. 35: 1127-9
10. Lucas DR, Unni KK, McLeod RA, O’Connor MI, Sim FH. Osteoblastoma: Clinicopathologic study of 306 cases. Hum Pathol. 1994. 25: 117-34
11. McDonald PJ, Matouk CC, Papsin B, Rutka JT. Clival osteoblastoma in a child. Case illustration. J Neurosurg. 2003. 98: 1133-
12. McLeod RA, Dahlin DC, Beabout JW. The spectrum of osteoblastoma. AJR Am J Roentgenol. 1976. 126: 321-5
13. Mitchell ML, Ackerman LV. Metastatic and pseudomalignant osteoblastoma: A report of two unusual cases. Skeletal Radiol. 1986. 15: 213-8
14. Moon KS, Jung S, Lee JH, Jung TY, Kim I, Kim SH. Benign osteoblastoma of the occipital bone: Case report and literature review. Neuropathology. 2006. 26: 141-6
15. Muzumdar D, Balasubramaniam S, Jhawar S, Goel A. Massive benign osteoblastoma of the suboccipital bone and foramen magnum region. Pediatr Neurosurg. 2010. 46: 232-7
16. Narita T, Ishii N, Mayuzumi H, Kobayashi H, Ikeda J, Iwasaki Y. Occipitoparietal benign osteoblastoma: Should entire lesion be resected when magnetic resonance images reveal wide abnormal signal intensity in surrounding bone marrow?. Surg Neurol. 2005. 64: 180-3
17. Tawil A, Comair Y, Nasser H, Hourani R, Rebeiz J, Chamoun R. Periosteal osteoblastoma of the calvaria mimicking a meningioma. Pathol Res Pract. 2008. 204: 413-22
18. Velasquez JC, Lau J, Kozyrev D, Sharafeddin F, Colasanti R, Luostarinen T. Clean, fast and preserving normal anatomy: “The Helsinki revolution” in microneurosurgery. J Neurosurg Sci. 2016. 60: 44-53
19. Wang YC, Huang JS, Wu CJ, Jeng CM, Fan JK, Resnick D. A huge osteoblastoma with aneurysmal bone cyst in skull base. Clin Imaging. 2001. 25: 247-50
20. Zileli M, Cagli S, Basdemir G, Ersahin Y. Osteoid osteomas and osteoblastomas of the spine. Neurosurg Focus. 2003. 15: E5-