- Department of Neurosurgery, Tokyo Women’s Medical University, Tokyo, Japan.
Correspondence Address:
Isamu Miura, Department of Neurosurgery, Tokyo Women’s Medical University, Tokyo, Japan.
DOI:10.25259/SNI_474_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Isamu Miura, Shiro Horisawa, Takakazu Kawamata, Takaomi Taira. Successful treatment of focal hand dystonia after cervical whiplash injury by thalamotomy. 26-Aug-2022;13:387
How to cite this URL: Isamu Miura, Shiro Horisawa, Takakazu Kawamata, Takaomi Taira. Successful treatment of focal hand dystonia after cervical whiplash injury by thalamotomy. 26-Aug-2022;13:387. Available from: https://surgicalneurologyint.com/surgicalint-articles/11824/
Abstract
Background: Posttraumatic focal hand dystonia after cervical whiplash injury is rare. Moreover, the treatment of peripheral posttraumatic dystonia is usually ineffective. Herein, we report a case of successful thalamotomy for a patient with focal hand dystonia after cervical whiplash injury.
Case Description: A 39-year-old woman was hit from behind by a car; subsequently, she felt strange in the right hand and was diagnosed with whiplash injury. A month later, she developed a persistent abnormal posture of the right hand. Brain imaging showed no lesions, and cervical magnetic resonance imaging showed stenosis but no spinal cord signal changes. Posttraumatic dystonia was diagnosed, for which the patient underwent left ventro-oral (Vo) thalamotomy. One year after the first surgery, the patient underwent left Vo and ventral intermediate nucleus (Vim) thalamotomy due to recurrence of dystonia. Nine years after the second surgery, the patient continues to be able to maintain her normal physical routine.
Conclusion: Vo-Vim thalamotomy may be a feasible and effective treatment for focal hand dystonia after cervical whiplash injury.
Keywords: Posttraumatic dystonia, Stereotactic thalamotomy, Ventral intermediate nucleus, Ventro-oral, Whiplash
INTRODUCTION
Trauma is thought to be a cause of secondary dystonia.[
CASE REPORT
The patient was a 39-year-old right-handed woman with an unremarkable medical history. She was hit from behind by a car while waiting at a traffic signal on her motorbike; subsequently, she had neck pain and felt restricted movement in the right hand. The patient was diagnosed with whiplash injury. One month later, she developed a persistent abnormal posture of the right hand. Electrophysiological examination showed no abnormal findings. Head computed tomography (CT) and brain magnetic resonance imaging (MRI) showed no lesions. Cervical MRI showed cervical canal stenosis but no spinal cord signal change. She was diagnosed with posttraumatic dystonia and referred to our hospital for surgical treatment.
On admission, her right thumb was adducted at the metacarpophalangeal (MP) joint and extended at the distal interphalangeal (DIP) joint. The second to fourth fingers were fixed in flexion at the DIP and proximal interphalangeal (PIP) joints. Her fifth finger was flexed at the DIP and PIP joints and extended at the MP joint [
First surgery
The patient underwent left Vo thalamotomy with the stereotactic target set at 1 mm above, 15 mm lateral to, and 2 mm posterior to the midpoint of the anterior commissure/ posterior commissure line. Surgery was performed under local anesthesia without any microelectrode recording. A monopolar radiofrequency probe (tip diameter, 1.0 mm; uninsulated length, 4.0 mm) was used. Macrostimulation (130 Hz, 100 μs pulse width, up to 15 mA) did not induce any adverse effects. Coagulation was performed at 70°C for 30 s at the tentative target, after which the electrode was withdrawn.
The extension and flexion of the right finger became smooth during the operation. There were no neurological deficits including paresthesia, dysphagia, sensory loss, or motor paresis after the surgery.
One day after the surgery, the patient extended and flexed the second to fourth fingers. Wrist movement got smooth. Seven days after the operation, the patient could write smoothly and was discharged. The patient reported recurrence of the right hand dystonia 14 months later; accordingly, revision surgery was planned.
Second surgery
The patient underwent left Vo and Vim thalamotomy; the stereotactic target coordinates, anesthesia, radiofrequency probe used, and coagulation procedure were all the same as those used for the first surgery. Macrostimulation (130 Hz, 100 μs pulse width, up to 15 mA) did not induce any adverse effects. Coagulation was performed at the tentative target. The electrode was withdrawn in 1 and 3 mm increments to increase lesion size, resulting in three contiguous lesions. As symptoms did not improve, the target was changed to 3 mm anterior and 3 mm posterior to the previous target. Three contiguous lesions anterior and two lesions posterior to the tentative target were made, resulting in a total of eight lesions [
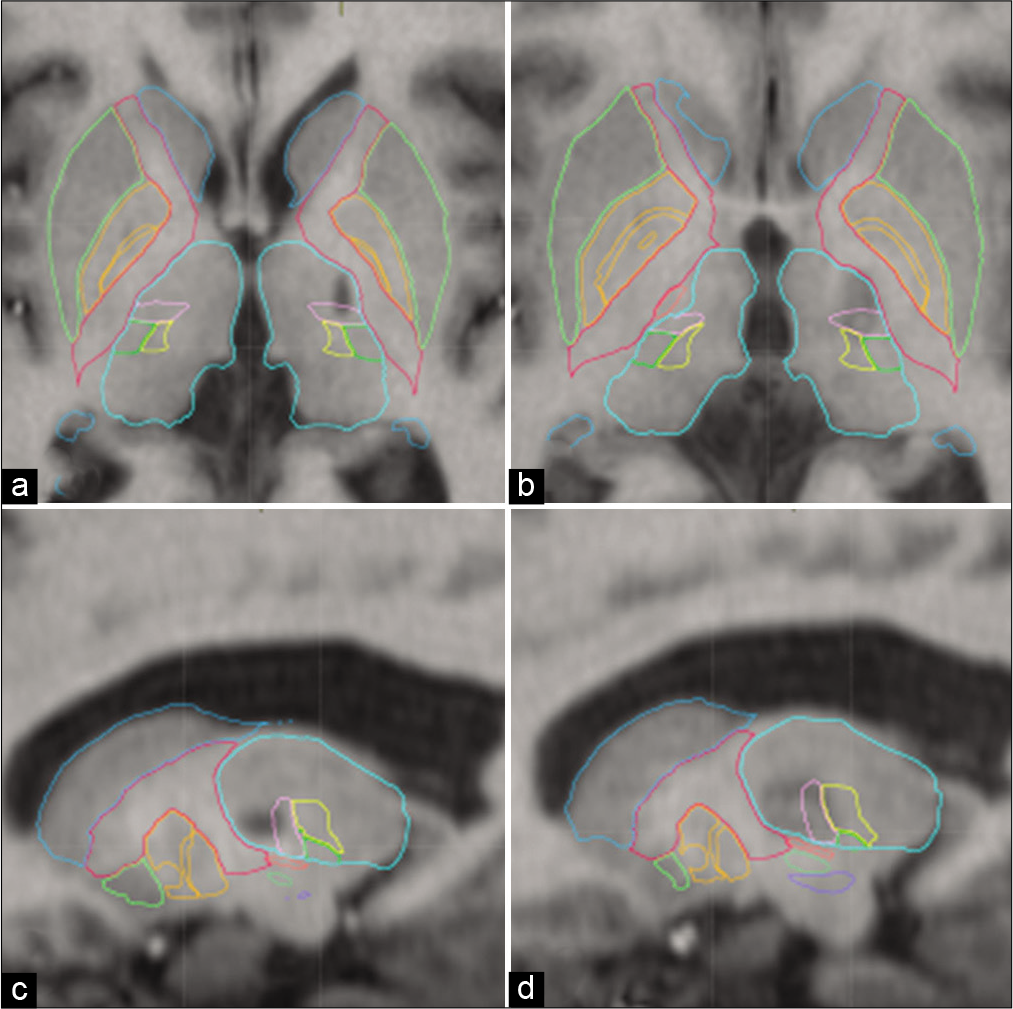
Figure 2:
Lesions revealed by T1-weighted MRI. A coagulation lesion can be seen on the ventro-oral (Vo) and ventral intermediate nucleus (Vim) border of the left thalamus before the second surgery (a and b). After the second surgery, coagulation lesions can be seen on both the Vo and Vim of the left thalamus (c and d).
There were no neurological deficits including paresthesia, dysphagia, sensory loss, or motor paresis after the second surgery. The patient was discharged 7 days after the second surgery. At the 8-year follow-up, although she reported occasionally experiencing awkwardness in her right hand, especially on cold days, the patient has maintained her normal physical routine.
DISCUSSION
Although trauma often precedes the onset of dystonia, its role in the development of dystonia has medical, psychological, and legal implications and is a controversial topic.[
The treatment of PPD, most commonly using botulinum toxin injections,[
CONCLUSION
Here we presented a patient with focal hand dystonia after cervical whiplash injury. Vo-Vim thalamotomy may be a feasible and effective treatment for peripheral posttraumatic dystonia.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Commentary
The authors of this case report describe very practical approach to a rarely-encountered but nevertheless very frustrating situation when the initial symptomatic improvement after an uneventful stereotactic lesioning procedure disappears over time. The decision they made – to repeat surgery, shift the target based on the patient’s response, and enlarge the area of thermocoagulation – was a good one, and the lasting symptomatic relief (over the 8 years of follow up) is indeed a confirmation of the correctness of their choice.
One may argue that in patients with post-traumatic dystonia, the surgical intervention should avoid further injury to the nervous system, and that preferred approach should be non-destructive, i.e., neuromodulation – deep brain stimulation, but the advantages of straightforward stereotactic thalamotomy (procedural simplicity, minimal follow up requirements, much lower cost) as illustrated in this case, definitely support judicial use of targeted lesioning in selected patients.
With relative rarity of dystonia due to whiplash, it would be unlikely to see a large clinical series covering its surgical treatment; therefore, a case report with a useful teaching point on management of symptomatic recurrence should serve as an illustration of clinical thinking and individually tailored treatment choice.
Konstantin Slavin, MD
University of Illinois at Chicago; Chicago, IL, USA
References
1. Cagnin A, Gasparoli E, Santelli L, Marcante A, Briani C. Posttraumatic dystonia and hemiplegic migraine: Different expressions of neuronal hyperexcitability?. Neurologist. 2012. 18: 36-8
2. Capelle HH, Grips E, Weigel R, Blahak C, Hansjörg B, Wohrle JC. Posttraumatic peripherally-induced dystonia and multifocal deep brain stimulation: Case report. Neurosurgery. 2006. 59: E702
3. Cavallieri F, Valzania F, Vercueil L, Moro E, Fraix V. A case of peripherally induced task-specific “lipstick dystonic tremor”. Tremor Other Hyperkinet Mov (N Y). 2019. 9: 689
4. Foley-Nolan D, Kinirons M, Coughlan RJ, O’Connor P. Post whiplash dystonia well controlled by transcutaneous electrical nervous stimulation (TENS): Case report. J Trauma. 1990. 30: 909-10
5. Frei K. Posttraumatic dystonia. J Neurol Sci. 2017. 379: 183-91
6. Hirato M, Miyagishima T, Takahashi A, Yoshimoto Y. Stereotactic selective thalamotomy for focal dystonia with aid of depth microrecording. World Neurosurg. 2018. 117: e349-61
7. Horisawa S, Goto S, Nakajima T, Ochiai T, Kawamata T, Taira T. Stereotactic thalamotomy for hairdresser’s dystonia: A case series. Stereotact Funct Neurosurg. 2016. 94: 201-6
8. Horisawa S, Ochiai T, Goto S, Nakajima T, Takeda N, Fukui A. Safety and long-term efficacy of ventro-oral thalamotomy for focal hand dystonia: A retrospective study of 171 patients. Neurology. 2019. 92: e371-7
9. Jankovic J. Peripherally induced movement disorders. Neurol Clin. 2009. 27: 821-32
10. Kim JP, Chang WS, Chang JW. The long-term surgical outcomes of secondary hemidystonia associated with post-traumatic brain injury. Acta Neurochir (Wien). 2012. 154: 823-30
11. Li HX, He L, Zhang CC, Eisinger R, Pan YX, Wang T. Deep brain stimulation in post-traumatic dystonia: A case series study. CNS Neurosci Ther. 2019. 25: 1262-9
12. Rojas-Medina LM, Esteban-Fernández L, RodríguezBerrocal V, Del Álamo de Pedro M, Ley Urzaiz L, BaillyBaillere IR. Deep brain stimulation in posttraumatic tremor: A series of cases and literature review. Stereotact Funct Neurosurg. 2016. 94: 379-86
13. Taira T, Hori T. Stereotactic ventrooralis thalamotomy for task-specific focal hand dystonia (writer’s cramp). Stereotact Funct Neurosurg. 2003. 80: 88-91
14. Tamburin S, Zanette G. Focal hand dystonia after cervical whiplash injury. J Neurol Neurosurg Psychiatry. 2003. 74: 134
15. Tarsy D. Comparison of acute-and delayed-onset posttraumatic cervical dystonia. Mov Disord. 1998. 13: 481-5
16. Tencer AF, Huber P, Mirza SK. A comparison of biomechanical mechanisms of whiplash injury from rear impacts. Annu Proc Assoc Adv Automot Med. 2003. 47: 383-98
17. van Rooijen DE, Geraedts EJ, Marinus J, Jankovic J, van Hilten JJ. Peripheral trauma and movement disorders: A systematic review of reported cases. J Neurol Neurosurg Psychiatry. 2011. 82: 892-8
18. Vasileiadis GI, Sakellariou VI, Papagelopoulos PJ, Zoubos AB. Posttraumatic focal dystonia of the shoulder. Orthopedics. 2012. 35: e977-80