- Department of Neurosurgery, Peoples’ Friendship University of Russia, Moscow, Russian Federation,
- Department of Neurosurgery, International Center for Neurological Restoration, Havanna, Cuba, Mexico,
- Department of Neurosurgery, Hospital Juárez de México, Mexico-City, Mexico,
- Charité – Universitätsmedizin Berlin, corporate member of Freie Universität Berlin, Humboldt-Universität zu Berlin, and Berlin Institute of Health, Berlin, Germany,
- Centre for Surgery Zurich, Klinik Hirslanden, Zurich, Switzerland.
Correspondence Address:
Ibrahim E. Efe, Department of Neurosurgery, Charité, Berlin, Germany.
DOI:10.25259/SNI_1229_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Manuel De Jesus Encarnacion-Ramirez1, Amaya Alvarez Aquino2, Rossi Evelyn Barrientos Castillo1, Gustavo Melo-Guzmán3, Durdica López-Vujnovic3, Agustin Blas3, Rubén Acosta-Garcés3, Miguel Bernés-Rodríguez3, Rafael Mendizabal Guerra3, Arturo Ayala-Arcipreste3, Renat Nurmukhametov1, Ibrahim E. Efe4,5. Surgical management of a penetrating drill bit injury to the skull base. 11-Feb-2022;13:49
How to cite this URL: Manuel De Jesus Encarnacion-Ramirez1, Amaya Alvarez Aquino2, Rossi Evelyn Barrientos Castillo1, Gustavo Melo-Guzmán3, Durdica López-Vujnovic3, Agustin Blas3, Rubén Acosta-Garcés3, Miguel Bernés-Rodríguez3, Rafael Mendizabal Guerra3, Arturo Ayala-Arcipreste3, Renat Nurmukhametov1, Ibrahim E. Efe4,5. Surgical management of a penetrating drill bit injury to the skull base. 11-Feb-2022;13:49. Available from: https://surgicalneurologyint.com/surgicalint-articles/11382/
Abstract
Background: Low-energy penetrating brain injuries are rarely encountered in neurosurgical practice. Immediate surgical management remains the primary treatment strategy to control potential bleeding and prevents infectious complications.
Case Description: A 28-year-old man presented with an orbital injury with left-sided chemosis, amaurosis, and ophthalmoplegia following an assault. Cranial CT revealed an industrial drill bit causing a penetrating injury to the skull base. The tip of the object reached the petrous apex. CT angiography showed no signs of cerebrovascular damage. The drill bit was visualized through a frontotemporal craniotomy. It was then carefully removed under direct microscopic vision. Postoperative ceftriaxone was administered. The patient was discharged in good condition on postoperative day 6. His vision impairment remained.
Conclusion: Timely access to neuroimaging diagnostics and microneurosurgical facilities allows for good outcomes in the surgical treatment of low-velocity penetrating brain injuries.
Keywords: Drill bit injury, Head trauma, Penetrating injury, Skull base, Traumatic brain injury
INTRODUCTION
Low-velocity penetrating injuries to the brain are a rare neurosurgical emergency. The most common causes include work-related accidents and suicide attempts. Reports on penetrating brain injuries as a result of assault are very scarce. These injuries demand immediate management to control potential hemorrhage and gross contamination. The literature suggests that neurosurgical removal under direct vision remains the safest treatment strategy.[
CASE DESCRIPTION
We here describe the microneurosurgical removal of a penetrating industrial drill bit from the skull base with the help of a frontotemporal craniotomy. A 28-year-old man presented to the emergency department following an assault resulting in an orbital injury and loss of consciousness for 20 min. He had orbital apex syndrome with left-sided amaurosis, ophthalmoplegia, ptosis, and trigeminal hypoesthesia of branches V1 and V2. His Glasgow coma score was 15 with no motor deficits. Cranial CT with bone reconstruction revealed an industrial drill bit of 10 cm penetrating the orbit, breaking through its posterior wall and reaching the middle fossa floor. The drill bit was in close proximity of the cavernous and petrous segments of the internal carotid artery. However, preoperative CT angiography showed no sign of vascular injury [
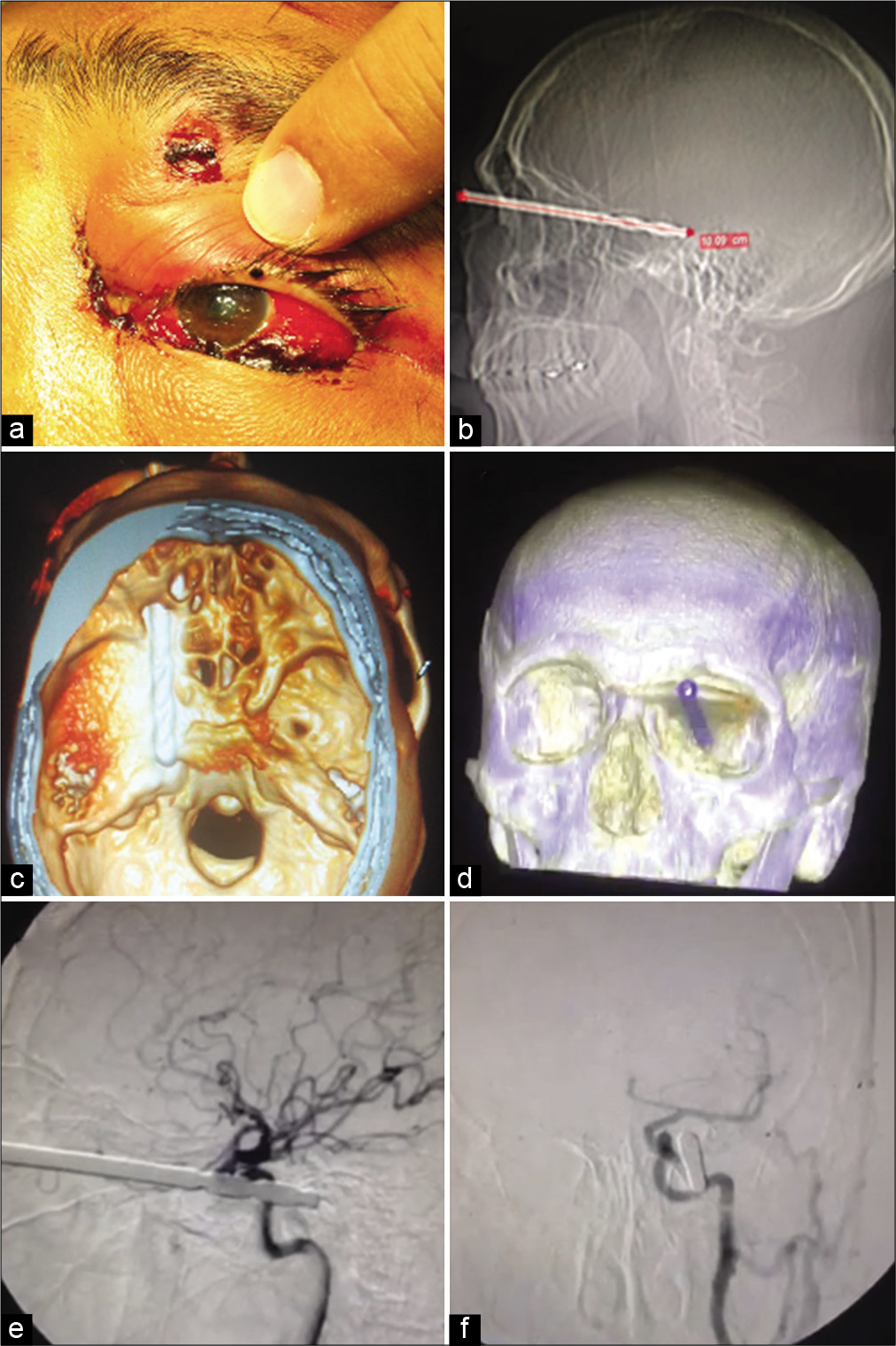
Figure 1:
The patient presented with a left-sided traumatic hemorrhagic chemosis (a), areflectic pupils, and palpebral edema with a 3 mm wide wound caused by a penetrating metallic object. Sagittal skull X-ray (b) showed a radiopaque foreign body of 10 cm length entering the orbital apex reaching the middle fossa floor. Three-dimensional reconstructions of the patient’s CT scans (c and d) revealed a drill bit crossing the orbital cone, passing by the left paraclinoid and parasellar regions reaching the petrous apex. Left internal carotid artery angiography (e and f) showed no evidence of vascular injury.
Surgical approach
We first exposed the carotid bifurcation to allow for distal control at the cervical level in case of an arterial injury during removal of the drill bit. The carotid artery was visualized through a 5 cm incision from the anterior edge of the sternocleidomastoid muscle to the angle of the mandible. Bleeding was controlled using monopolar electrocoagulation. The external carotid artery is identified through its first branch, the superior thyroid artery whereas the internal carotid artery has no cervical branches [
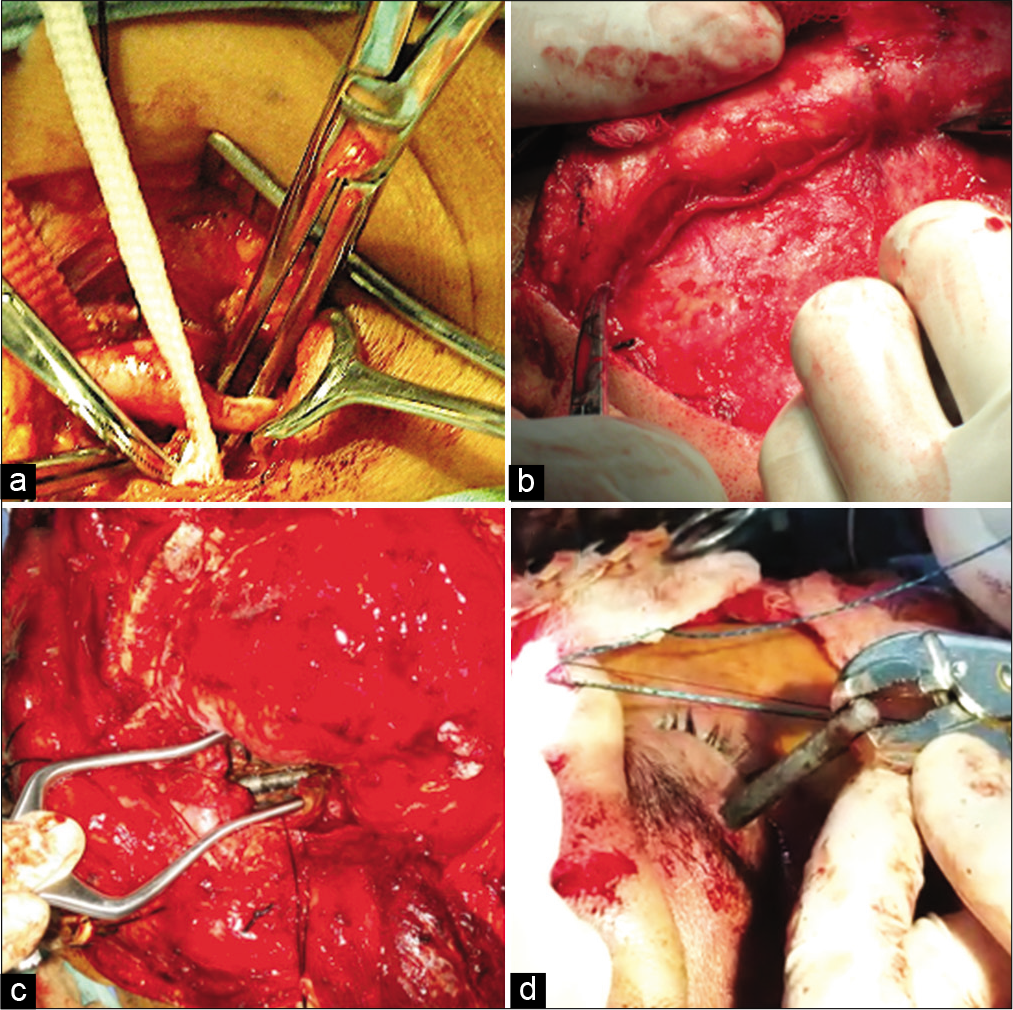
Figure 2:
The cervical segment of the internal carotid artery (a) was dissected in case a distal control was needed during the surgery. It can be appreciated in front of the metal clamp. The carotid bifurcation is seen distal to the internal carotid artery. The superficial temporal artery (b) was dissected to be used as a graft vessel in case an extracranial-to-intracranial bypass was needed. The drill bit was identified inside the intraconal space of the orbit (c). The drill bit was extracted through its transpalpebral penetration site (d).
We performed a Dandy type incision involving the temporal and the entire frontal region. We then carefully dissected the superficial temporal artery to be used for an extracranialto-intracranial bypass in case of an intraoperative vascular injury. The temporal muscle was dissected using the Oikawa technique to preserve the muscular vasculature and prevent temporal muscle atrophy. The interfascial dissection of the temporal muscle from the root of zygoma to the outer edge of the orbital crest further avoided injury to the frontotemporal branch of the facial nerve.
We used an orbitozygomatic craniotomy following four burr holes in the McCarthy keyhole, the root of zygoma, posterior to the superior temporal line, and in the anterior parasagittal region of the frontal bone. An orbital osteotomy involving the lateral wall and the orbital roof was performed. A periorbital dissection along the conal fat exposed the object which was then followed to the orbital apex where it penetrated through the posterior wall of the orbit. The dura mater was opened in a C-shaped fashion to locate the basal cisterns of the skull base, the optic nerve, the supraclinoid carotid, and the ipsilateral third nerve. The lateral wall of the cavernous sinus and the drill bit was visualized. The drill bit was then slowly and gradually removed under microscopic supervision using a strong clamp. The dura mater was then closed and the bone flap was placed back.
Outcome
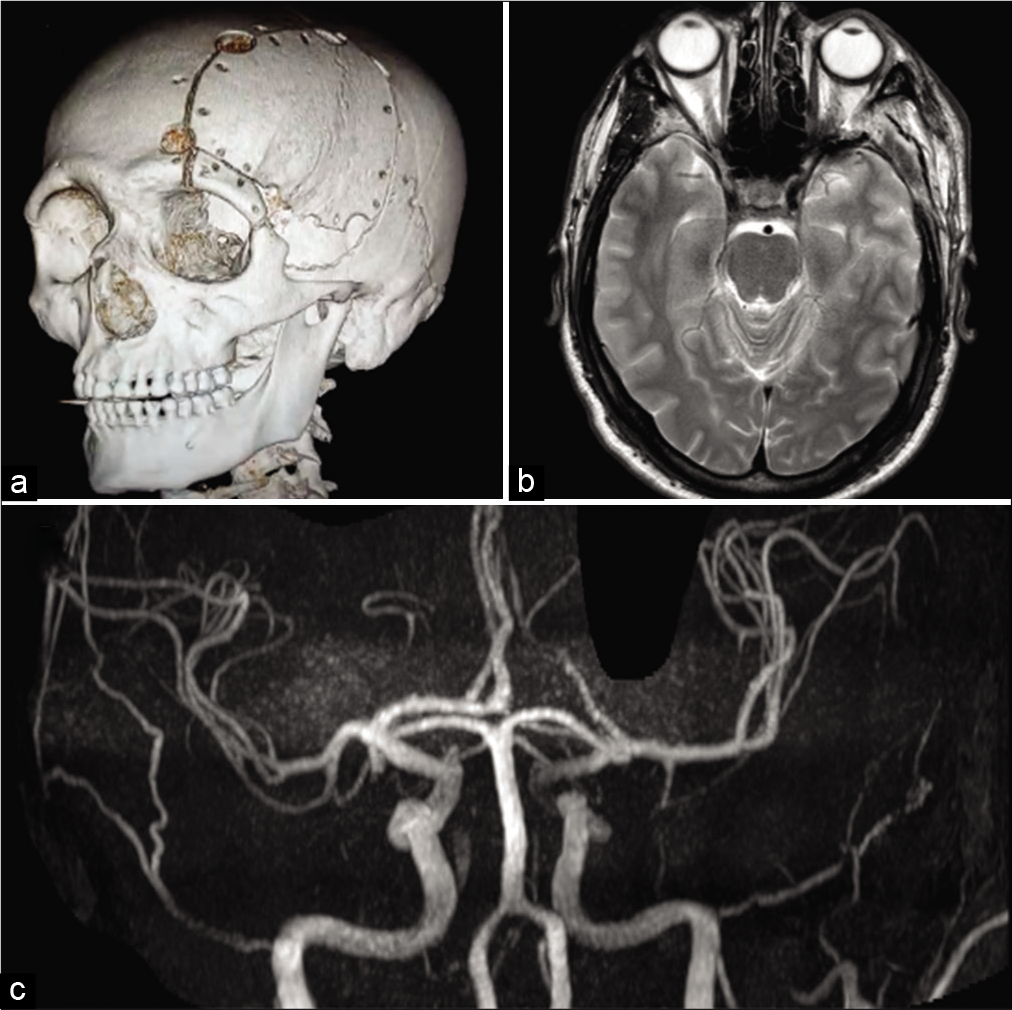
The patient was hospitalized for 5 days for antibiotic medication with ceftriaxone and was discharged at postoperative day 6. His palpebral edema progressively reduced whereas his visual impairment persisted. His postoperative CT and MRI scans showed no evidence of purulent collections or damage of the cerebral parenchyma [
DISCUSSION
Extent of injury depends mainly on the kinetic energy generated by the penetrating object. Low-velocity penetrating brain injuries are much less common than injuries suffered from high-velocity projectiles. They typically confer better outcomes due to the lower kinetic energy and hence little anatomical disruption.[
Decision-making and safe surgical removal warrants a range of neuroimaging modalities. The cranial CT can rule out intracranial bone fragments and hematomas. It further allows for a 3D reconstruction to visualize the drill bit trajectory. Neuronavigation can further help localize the object intraoperatively.[
Follow-up angiograms are highly recommended to detect secondary pseudoaneurysms and intracranial hemorrhage.[
Penetrating brain injuries pose a high risk of local wound infections, meningitis, encephalitis, or cerebral abscess. Besides careful washing of the surgical field to remove contaminated bone and tissue fragments, antibiotic medication should be started. Most common pathogens include staphylococcus aureus and Gram-negative organisms.[
CONCLUSION
Despite being an extremely rare emergency, low-energy penetrating injuries to the brain can be surgically treated with good outcomes. Timely access to adequate imaging diagnostics and a microneurosurgical facility are crucial for safe removal.
Submission declaration
No copyright material was used in this manuscript. This work has never been published before and is currently not being considered for publication in any other journal. If accepted, it will not be published elsewhere in English or in any other language. All authors agreed to the submission of this manuscript.
Protection of patients’ rights to privacy statement
No identifying information can be found anywhere in our submission.
Human rights statement
All procedures described in this manuscript were in accordance with the ethical standards published in the Helsinki Declaration of 1975, as revised in 2000.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Awori J, Wilkinson DA, Gemmete JJ, Thompson BG, Chaudhary N, Pandey AS. Penetrating head injury by a nail gun: Case report, review of the literature, and management considerations. J Stroke Cerebrovasc Dis. 2017. 26: e143-9
2. Bayston R, de Louvois J, Brown E, Johnston R, Lees P, Pople I. Use of antibiotics in penetrating craniocerebral injuries. Lancet. 2000. 355: 1813-7
3. Benzel EC, Day WT, Kesterson L, Willis BK, Kessler CW, Modling D. Civilian craniocerebral gunshot wounds. Neurosurgery. 1991. 29: 67-72
4. Blankenship BA, Baxter AB, McKahn GM. Delayed cerebral artery pseudoaneurysm after nail gun injury. Am J Roentgenol. 1999. 172: 541-2
5. Enam S, Kazim S, Tahir M, Waheed S, Shamim M. Management of penetrating brain injury. J Emerg Trauma Shock. 2011. 4: 395-402
6. Ferraz VR, Aguiar GB, Vitorino-Araujo JL, Badke GL, Veiga JC. Management of a low-energy penetrating brain injury caused by a nail. Case Rep Neurol Med. 2016. 2016: 4371367
7. Freeman BJC, Ainscow DA. Nail gun injury: An update. Injury. 1994. 25: 110-1
8. Litvack ZN, Hunt MA, Weinstein JS, West GA. Self-inflicted nail-gun injury with 12 cranial penetrations and associated cerebral trauma. Case report and review of the literature. J Neurosurg. 2006. 104: 828-34
9. Luo W, Liu H, Hao S, Zhang Y, Li J, Liu B. Penetrating brain injury caused by nail guns: Two case reports and a review of the literature. Brain Inj. 2012. 26: 1756-62
10. . Part 2: Prognosis in penetrating brain injury. J Trauma. 2001. 51: S44-86
11. Woodall MN, Alleyne CH. Nail-gun head trauma: A comprehensive review of the literature. J Trauma Acute Care Surg. 2012. 73: 993-6
12. Zhu RC, Yoshida MC, Kopp M, Lin N. Treatment of a self-inflicted intracranial nail gun injury. BMJ Case Rep. 2021. 14: e237122