- Department of Neurosurgery, University of Occupational and Environmental Health, Kitakyusyu, Fukuoka, Japan.
Correspondence Address:
Kohei Suzuki, Department of Neurosurgery, University of Occupational and Environmental Health, Kitakyusyu, Fukuoka, Japan.
DOI:10.25259/SNI_765_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Taichi Shimabukuro, Kohei Suzuki, Yoshiteru Nakano, Junkoh Yamamoto. Surgical management of primary Ewing’s sarcoma of the petroclival bone extend into the sphenoid sinus: A case report and review of literatures. 06-Oct-2021;12:500
How to cite this URL: Taichi Shimabukuro, Kohei Suzuki, Yoshiteru Nakano, Junkoh Yamamoto. Surgical management of primary Ewing’s sarcoma of the petroclival bone extend into the sphenoid sinus: A case report and review of literatures. 06-Oct-2021;12:500. Available from: https://surgicalneurologyint.com/surgicalint-articles/11160/
Abstract
Background: Ewing’s sarcoma (ES) is a malignancy that arises from bones or soft tissue, characterized by primitive small and round blue cells. Primary ES typically occurs in the long bones, vertebrae, or pelvis, and is extremely rare in the skull base.
Case Description: A 14-year-old girl presented with posterior cervical pain and dysfunction of multiple cranial nerves (CNs). Radiological investigation revealed a solid mass of the petroclival bone extending into the sphenoid sinus. The patient underwent endoscopic transsphenoidal surgery for diagnosis of the pathology, and partial resection was safely achieved. Histopathological, genetic, and radiological examinations confirmed the diagnosis of primary ES. Subsequently, the patient underwent adjuvant chemotherapy and radiotherapy following which the clinical symptoms resolved. Complete response was achieved after multimodal treatment. Twenty months after treatment, the patient remains in remission without recurrence or metastatic disease. Primary ES of the petroclival bone has been reported in only three cases in the literature. As seen in the present case, dysfunction of multiple CNs is the most common manifestation of petroclival ES. Diagnosis should be confirmed by histopathological and genetic examinations considering the nonspecific clinical symptoms and radiological features.
Conclusion: Multimodal treatment, including surgery, chemotherapy, and radiotherapy, can result in favorable outcomes. Clinicians should consider safe resection during surgical management to prevent complications that can delay postoperative multimodal treatment.
Keywords: Endoscopic transsphenoidal surgery, Ewing’s sarcoma, Garcin syndrome, Petroclival, Sinonasal, Skull base
INTRODUCTION
Ewing’s sarcoma (ES) is a malignancy that arises from bones or soft tissue, characterized by primitive small and round blue cells.[
CASE REPORT
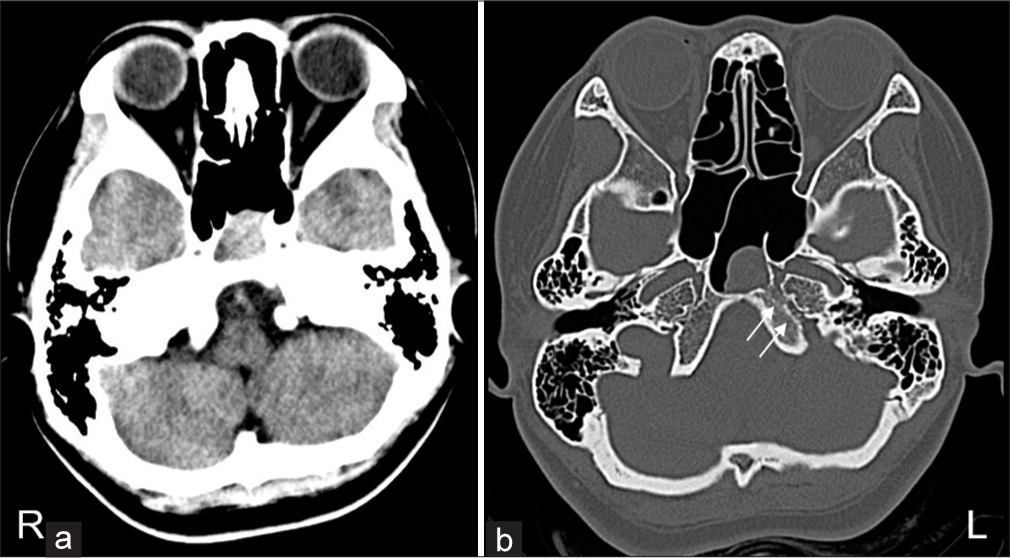
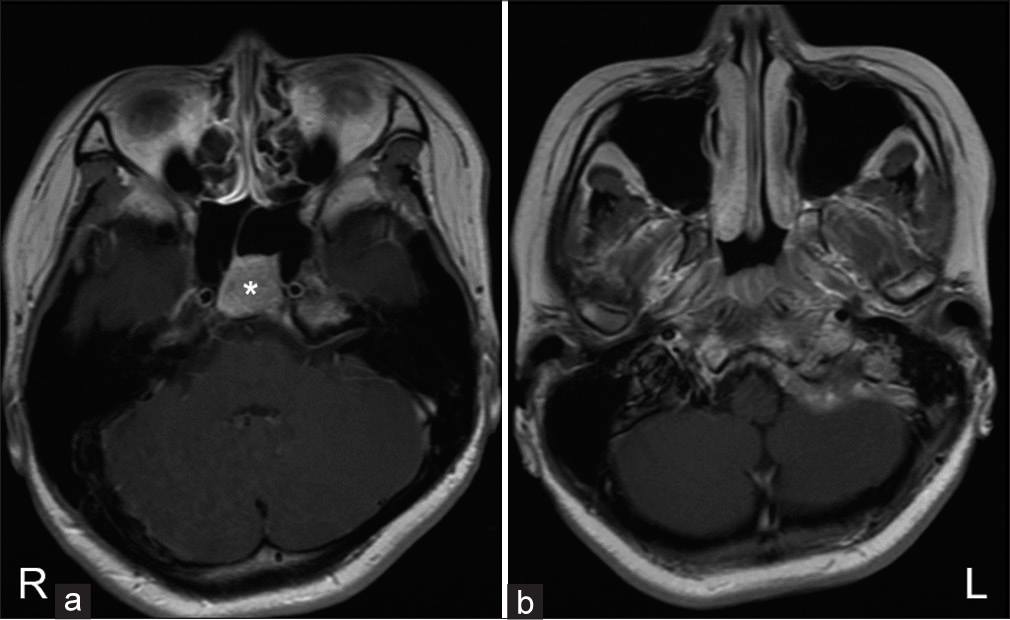
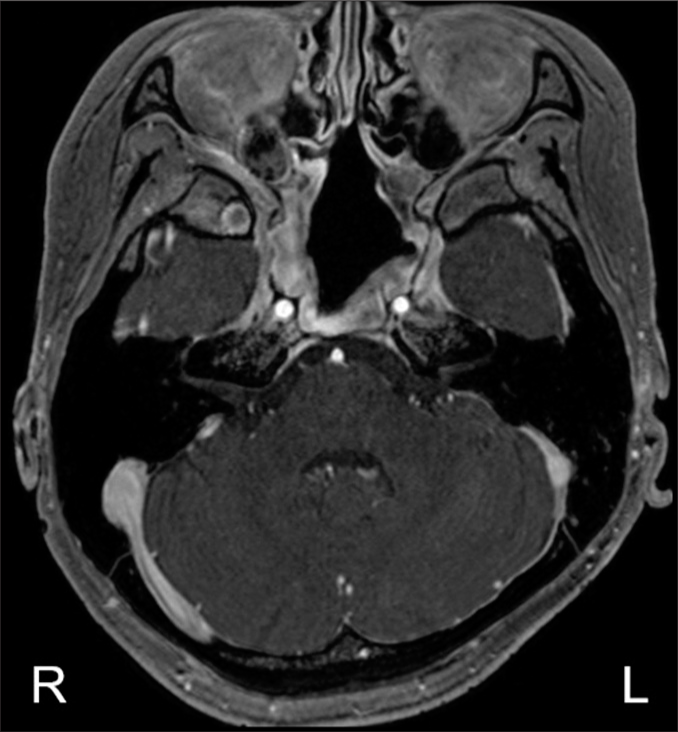
A 14-year-old girl who presented with the left posterior cervical pain and dysphasia was diagnosed with polyneuropathy due to reactive herpes virus infection by otolaryngologists. She was treated with antiviral drugs and adrenal corticosteroids; however, the symptoms worsened rapidly. Moreover, the patient developed hoarseness of voice due to vocal cord palsy 2 weeks after the initial manifestations. Additional investigations were performed considering the uncommon clinical course, and a skull base tumor was identified. The patient was referred to our department a month after the initial manifestations. Physical examination revealed left anterior and posterior cervical pain and multiple left cranial nerve (CN) palsies (glossopharyngeal, vagus, and accessory nerves). Serological examination did not reveal any obvious abnormalities. Computed tomography (CT) revealed enlargement of the left petroclival synchondrosis with osteoclastic changes and a soft-tissue mass within the adjacent sphenoid sinus [
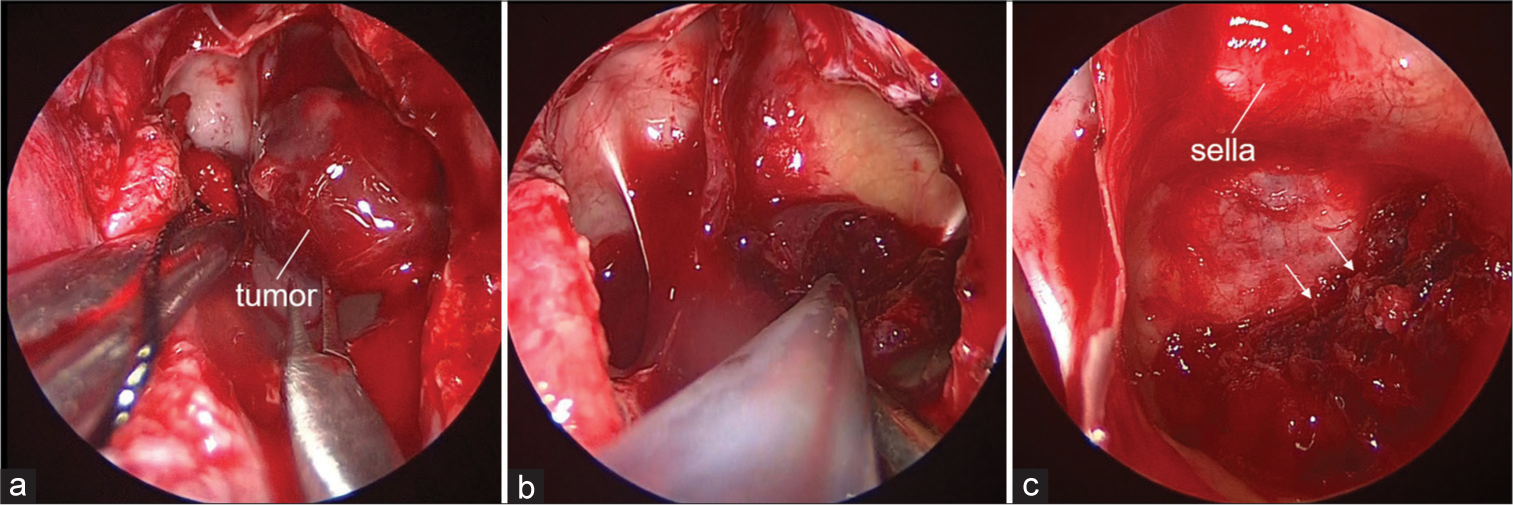
Due to the rapid progression of clinical symptoms, the patient underwent endoscopic transsphenoidal surgery for diagnosis of the pathology. Intraoperatively, the tumor was found to extend into the sphenoid sinus and underlie the edematous mucosa of the sinus [
Figure 3:
Intraoperative findings. The tumor exposed by the transsphenoidal approach underlying the edematous sphenoid sinus mucosa (a). The tumor was relatively fibrous and was resected using ultrasound aspirator (b). Residual tumor connected to the petroclival lesion through the destructive clivus (allows) (c).
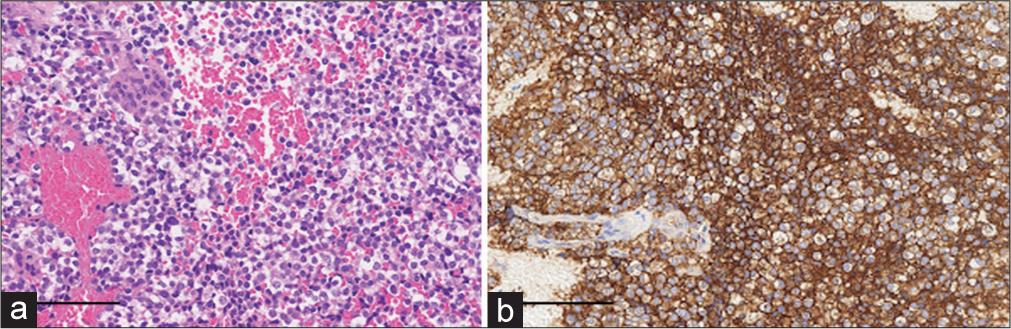
Histopathological examination revealed a lesion composed of round cells with clear cytoplasm and uniformly round nuclei [
Subsequently, the patient underwent adjuvant multidrug chemotherapy and radiotherapy. Five cycles of adjuvant chemotherapy using vincristine (2 mg/m2), doxorubicin (37.5 mg/m2), and cyclophosphamide (1200 mg/m2), alternating with etoposide (100 mg/m2) and ifosfamide (1800 mg/m2) combined with G-CSF, were performed every 2–3 weeks along with intensity-modulated radiation therapy (60 Gy/30 fractions). In addition, two cycles of chemotherapy using vincristine and cyclophosphamide, alternating with etoposide and ifosfamide, were performed at 2-week intervals. The patient experienced anemia, neutropenic fever, and thrombocytopenia. Complete response was achieved 9 months after adjuvant chemotherapy. At the 22-month post-surgical follow-up, the patient had recovered well with no clinical or radiological evidence of recurrence or metastatic disease [
DISCUSSION
Primary ESs of skull base involvement are extremely rare, and to date, only three cases of primary ES of the petroclival bone have been reported [
In cases of primary ES of the cranium, initial diagnosis can be difficult due to nonspecific clinical symptoms and radiological features. Therefore, the diagnosis should be confirmed by histopathological and genetic examinations. ES is characterized by primitive small round cells with high nuclear to cytoplasmic rate arranged in a sheet pattern.[
Regarding surgical management, previous reports have recommended that tumor resection should be as radical as possible.[
CONCLUSION
Primary ES of the petroclival bone is extremely rare and can commonly extend into the surrounding critical structures. Multimodal treatment can result in favorable outcomes, and improvement in CN palsy can be observed several months after the treatment with regular follow-up. Therefore, to avoid delay in the induction of postoperative treatment, safe resection of the tumor without any complications rather than radical resection should be considered in cases of primary skull base ES associated with multiple CN palsies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
References
1. Balasubramaniam S, Nadkarni T, Menon R, Goel A, Rajashekaran P. Primary Ewing’s sarcoma of the petroclival bone. J Clin Neurosci. 2008. 15: 712-4
2. Bernstein M, Kovar H, Paulussen M, Randall RL, Schuck A, Teot LA. Ewing’s sarcoma family of tumors: Current management. Oncologist. 2006. 11: 503-19
3. Bridge RS, Rajaram V, Dehner LP, Pfeifer JD, Perry A. Molecular diagnosis of Ewing sarcoma/primitive neuroectodermal tumor in routinely processed tissue: A comparison of two FISH strategies and RT-PCR in malignant round cell tumors. Mod Pathol. 2006. 19: 1-8
4. Gurney JG, Davis S, Severson RK, Fang JY, Ross JA, Robison LL. Trends in cancer incidence among children in the U.S.. Cancer. 1996. 78: 532-41
5. Klein EA, Anzil AP, Mezzacappa P, Borderon M, Ho V. Sinonasal primitive neuroectodermal tumor arising in a long-term survivor of heritable unilateral retinoblastoma. Cancer. 1992. 70: 423-31
6. Krishnamani K, Kumar TN, Gandhi LV, Raghunadharao D, Sadashivudu G, Megha U. Primary Ewing’s sarcoma of the cranium: Case series and review of literature. J Cancer Res Ther. 2014. 10: 377-80
7. Schartz D, Divakar P, Tafe L, Paydarfar J. Primary Ewing’s sarcoma of the petroclival bone: A case report and literature review. Surg Neurol Int. 2020. 11: 6
8. Thakar S, Furtado S, Ghosal N, Dilip J, Mahadevan A, Hegde A. Skull-base Ewing sarcoma with multifocal extracranial metastases. J Cancer Res Ther. 2012. 8: 636-8
9. Veselis CA, Awan O, Thomas A, Ling S, Jonnalagadda P, Aneja A. Bone Tumors occurring in the soft tissues: A review of the clinical, imaging, and histopathologic findings. Curr Probl Diagn Radiol. 2021. 50: 419-29
10. Yeshvanth SK, Ninan K, Bhandary SK, Lakshinarayana KP, Shetty JK, Makannavar JH. Rare case of extraskeletal Ewings sarcoma of the sinonasal tract. J Cancer Res Ther. 2012. 8: 142-4