- Department of Neurosurgery, University of Helsinki and Helsinki University Hospital, Helsinki, Finland,
- Department of Neurosurgery, Heinrich-Heine University Medical Center, Düsseldorf, Germany.
Correspondence Address:
Sajjad Muhammad
Department of Neurosurgery, University of Helsinki and Helsinki University Hospital, Helsinki, Finland,
DOI:10.25259/SNI_294_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sajjad Muhammad, Ahmad Hafez, Atte Karppinen, Mika Niemelä. Surgical treatment of a rare rosette-forming glioneuronal tumor in the pineal region. 18-Apr-2020;11:68
How to cite this URL: Sajjad Muhammad, Ahmad Hafez, Atte Karppinen, Mika Niemelä. Surgical treatment of a rare rosette-forming glioneuronal tumor in the pineal region. 18-Apr-2020;11:68. Available from: https://surgicalneurologyint.com/surgicalint-articles/9969/
Abstract
Background: Rosette-forming glioneuronal tumors (RGNTs) in the pineal region are rare. RGNTs have been described in the fourth ventricle, but rarely reported in other brain regions. Here, we report the radiological findings, surgical treatment, and short-term outcome of an RGNT found in the pineal region.
Case Description: We present a case of a 22-year-old medical student with a 4-month history of headaches and diplopia. A previous magnetic resonance imaging scan revealed a mass in the pineal region, with heterogeneous contrast enhancement and hydrocephalus. Three months prior, an endoscopic biopsy and third ventriculocisternostomy were performed elsewhere; the diagnosis was neurocytoma Grade I, and radiotherapy was planned. The patient presented at our hospital for a second opinion, and we suggested surgical treatment. A near-total resection was performed in sitting position using a supracerebellar infratentorial microsurgical approach. The tumor was very soft and not well vascularized. Diplopia was initially worsened after the tumor was removed and relieved completely after 2 weeks. An 8-week follow-up examination revealed that the patient was free of symptoms. Histological analysis confirmed it was an RGNT.
Conclusion: Maximal safe resection in pineal region RGNTs is a feasible and recommended treatment option.
Keywords: Operative nuances, Pineal region, Rosette-forming glioneuronal tumor
INTRODUCTION
Rosette-forming glioneuronal tumors (RGNTs) are an unusual variant of mixed neuronal-glial tumors. RGNTs are typically found in the fourth ventricle, with limited extension to the surrounding structures (cerebellar vermis, midbrain, and cerebral aqueduct). They were initially classified as novel “rosette-forming glioneuronal tumors of the fourth ventricle” according to the 2007 WHO classification of central nervous tumors.[
CASE HISTORY
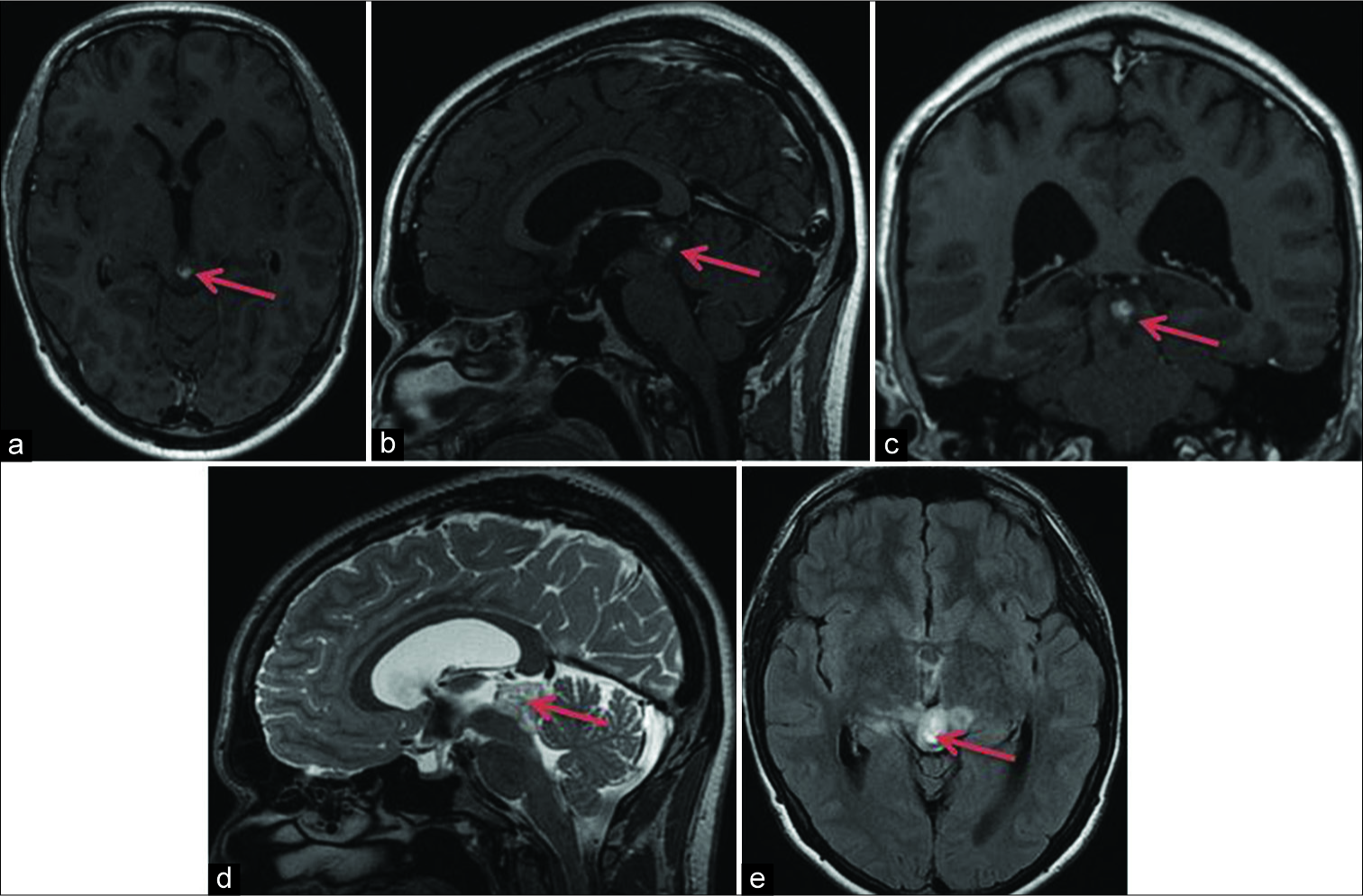
A 22-year-old medical student presented with a 4-month history of headache and diplopia. A previous magnetic resonance imaging (MRI) scan revealed a contrast- enhancing lesion in the pineal region. An endoscopic biopsy and third ventriculocisternostomy were performed elsewhere; the diagnosis was neurocytoma Grade I. Radiotherapy was planned elsewhere. The patient presented to our hospital for a second opinion. After oncological consultation, we suggested surgical resection of the tumor. On examination, the patient was alert and oriented. Visual field was intact, and pupil size was normal and reactive to light. The patient’s hearing and facial nerve function were normal. A new MRI scan revealed a contrast-enhancing space-occupying lesion of approximately 2 cm in size in the pineal region [
Surgery of pineal region RGNT
Operative findings
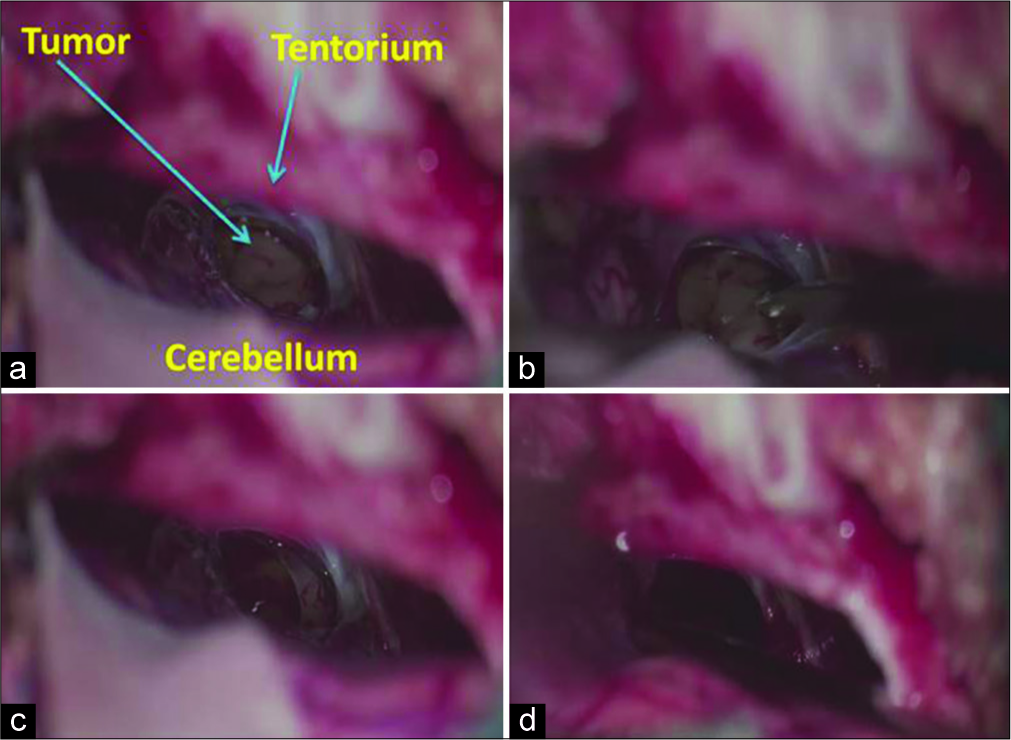
Surgery was performed with the patient in sitting position. A supracerebellar infratentorial approach was used, with an OPMI PENTERO 900 microscope (Carl Zeiss, Germany). The dura was opened in a Y-shaped fashion, preserving the main veins in the tentorial region. The tumor was easily recognized; it was soft, cystic, and pale yellow in color [
Postoperative outcome
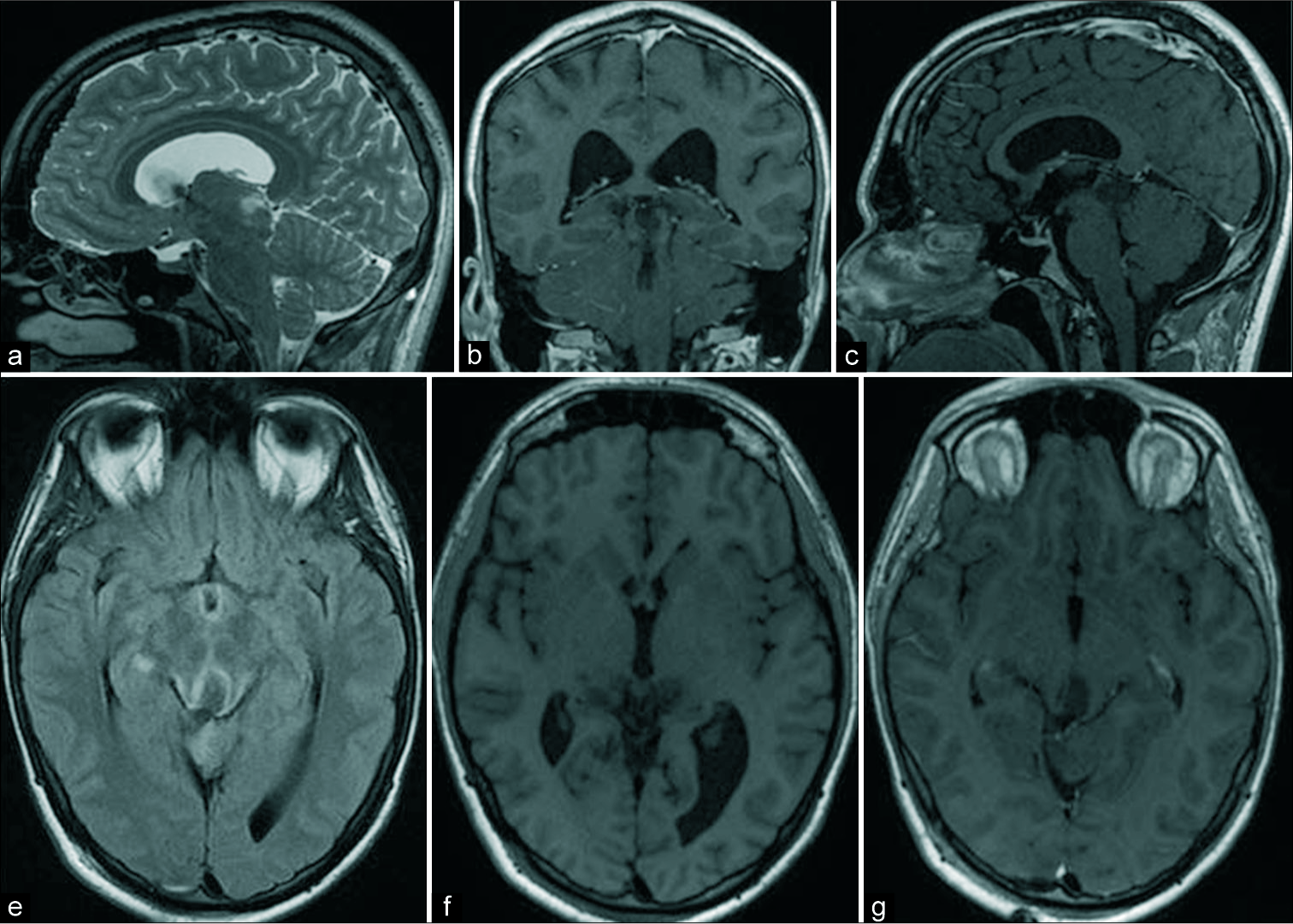
Diplopia was initially worse but completely relieved 2 weeks after the surgery, without any new focal neurological deficit. No other complications occurred. The patient was discharged from the hospital 4 days after the surgery. An 8-week follow-up examination revealed that the patient was without symptoms. Histological analysis showed an RGNT. Postoperative MRI scans showed a small remnant in posterior part of thalamus and aqueduct [
DISCUSSION
An RGNT in the pineal region is a rare affliction. It mainly affects young adults – predominantly females – with a peak incidence among people in their thirties.[
Due to limited experience with therapeutic treatments such as stereotactic radiosurgery or chemotherapy, surgical resection aimed at achieving gross total resection remains the preferred treatment of RGNTs. RGNTs are Grade I benign tumors, but aggressive progression and ventricular dissemination have been previously described.[
CONCLUSION
Maximal safe resection of RGNTs in the pineal region is a feasible and recommended treatment option.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the research committee of University of Helsinki and with the 1964 Declaration of Helsinki and its amendments or comparable ethical standards.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
We are thankful to the Ehrnrooth Foundation for providing funding to SM for a clinical vascular and skull base fellowship at the Department of Neurosurgery at the University of Helsinki.
Conflicts of interest
There are no conflicts of interest.
References
1. Allinson KS, O’Donovan DG, Jena R, Cross JJ, Santarius TS. Rosette-forming glioneuronal tumor with dissemination throughout the ventricular system: A case report. Clin Neuropathol. 2015. 34: 64-9
2. Anyanwu CT, Robinson TM, Huang JH. Rosette-forming glioneuronal tumor: An update. Clin Transl Oncol. 2019. 2019: 1-8
3. Bidinotto LT, Scapulatempo-Neto C, Mackay A, de Almeida GC, Scheithauer BW, Berardinelli GN. Molecular profiling of a rare rosette-forming glioneuronal tumor arising in the spinal cord. PLoS One. 2015. 10: e0137690-
4. Cachia D, Prado MP, Theeler B, Hamilton J, McCutcheon I, Fuller GN. Synchronous rosette-forming glioneuronal tumor and diffuse astrocytoma with molecular characterization: A case report. Clin Neuropathol. 2014. 33: 407-11
5. Chiba K, Aihara Y, Eguchi S, Tanaka M, Komori T, Okada Y. Rosette-forming glioneuronal tumor of the fourth ventricle with neurocytoma component. Childs Nerv Syst. 2014. 30: 351-6
6. García Cabezas S, Serrano Blanch R, Sanchez-Sanchez R, Palacios Eito A. Rosette-forming glioneuronal tumour (RGNT) of the fourth ventricle: A highly aggressive case. Brain Tumor Pathol. 2015. 32: 124-30
7. Gessi M, Lambert SR, Lauriola L, Waha A, Collins VP, Pietsch T. Absence of KIAA1549-BRAF fusion in rosette-forming glioneuronal tumors of the fourth ventricle (RGNT). J Neurooncol. 2012. 110: 21-5
8. Komori T, Scheithauer BW, Hirose T. A rosette-forming glioneuronal tumor of the fourth ventricle: Infratentorial form of dysembryoplastic neuroepithelial tumor?. Am J Surg Pathol. 2002. 26: 582-91
9. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007. 114: 97-109
10. Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK. The 2016 World Health Organization classification of tumors of the central nervous system: A summary. Acta Neuropathol. 2016. 131: 803-20
11. Medhi G, Prasad C, Saini J, Pendharkar H, Bhat MD, Pandey P. Imaging features of rosette-forming glioneuronal tumours (RGNTs): A series of seven cases. Eur Radiol. 2016. 26: 262-70
12. Wang Y, Xiong J, Chu SG, Liu Y, Cheng HX, Wang YF. Rosette-forming glioneuronal tumor: Report of an unusual case with intraventricular dissemination. Acta Neuropathol. 2009. 118: 813-9
13. Xiong J, Liu Y, Chu SG, Chen H, Chen HX, Mao Y. Rosette-forming glioneuronal tumor of the septum pellucidum with extension to the supratentorial ventricles: Rare case with genetic analysis. Neuropathology. 2012. 32: 301-5
14. Yang C, Fang J, Li G, Li S, Ha T, Wang J. Histopathological, molecular, clinical and radiological characterization of rosette-forming glioneuronal tumor in the central nervous system. Oncotarget. 2017. 8: 109175-90