- Department of Neurosurgery, Saiseikai Shiga Hospital, Ritto, Japan.
- Department of Neurosurgery, Kyoto Prefectural University of Medicine, Kyoto, Japan.
DOI:10.25259/SNI_332_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Takuma Aoki1, Daisuke Umebayashi2, Kazunori Tatsuzawa2, Naoya Hashimoto2. Symptomatic Chiari type 1 malformation associated with acromegaly: A case report. 14-Jun-2021;12:283
How to cite this URL: Takuma Aoki1, Daisuke Umebayashi2, Kazunori Tatsuzawa2, Naoya Hashimoto2. Symptomatic Chiari type 1 malformation associated with acromegaly: A case report. 14-Jun-2021;12:283. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10884
Abstract
Background: Here, we report a patient who presented with both symptomatic acromegaly and symptomatic Chiari I malformation (CM1) with a C2-T5 syrinx.
Case Description: A 63-year-old female presented with bilateral arm dysesthesias and back pain. For approximately the past 30 years, she had chronic signs of acromegaly (i.e. an enlarged forehead, jaw, and nose, and enlarged hands and feet). When the cervical magnetic resonance showed a CM1 (tonsillar herniation) with C2-T5 syringomyelia, she underwent foramen magnum decompression and C1 posterior arch resection. Postoperatively, she was asymptomatic. The added finding of a growth hormone (GH)-producing pituitary lesion was treated medically with endocrine therapy, as she had incidentally required surgery/chemotherapy for a newly diagnosed colon cancer.
Conclusion: Symptomatic CM1, syrinx, and acromegaly may occur together. Appropriately treatment may include a suboccipital decompression, and C1 arch resection surgery, followed by either surgical or medical treatment for the GH-producing pituitary adenoma.
Keywords: Acromegaly, Chiari malformation, Pituitary adenoma, Syringomyelia
INTRODUCTION
A patient acutely presented with a Chiari I malformation (CM1), syrinx from C2-T5, and a pituitary adenoma (i.e. growth hormone [GH]-producing lesion resulting acromegaly). The former was managed with a suboccipital craniectomy and C1 laminectomy/fusion, while the accompanying pituitary lesion was managed medically/endocrinologically, due to the patient’s newly discovered colon carcinoma warranting surgery, radiation, and chemotherapy.
CASE PRESENTATION
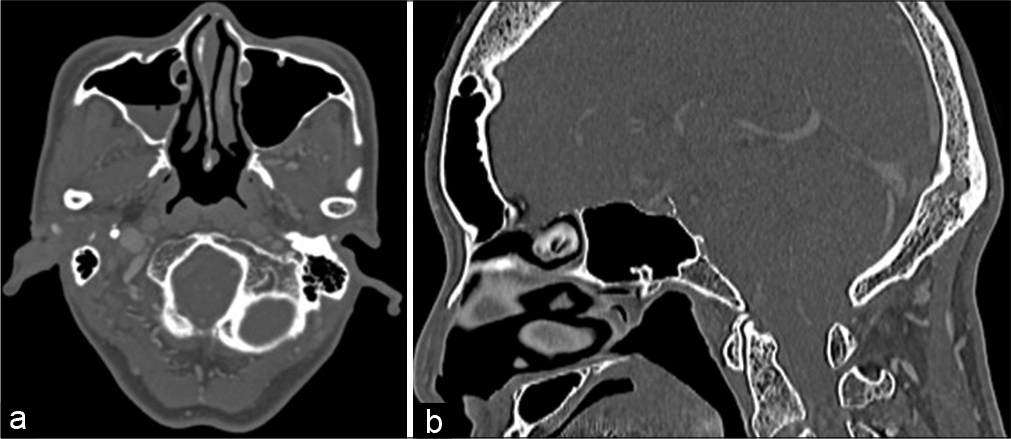
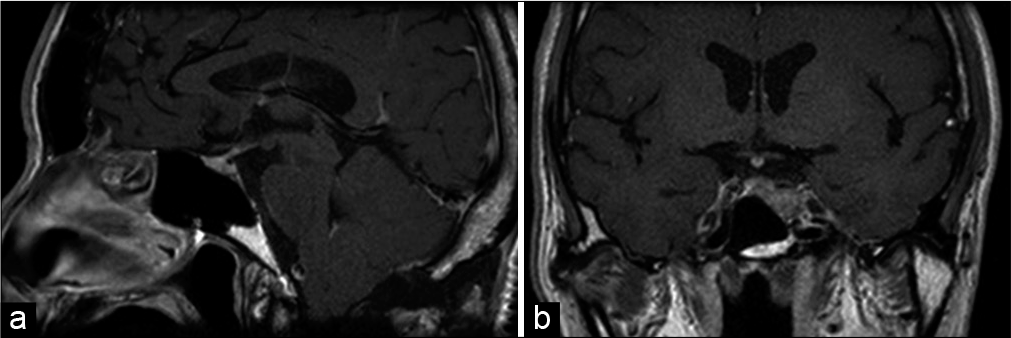
A 63-year-old female presented with 30 years duration of acromegaly (i.e. a large forehead, jaw, nose, hands, and feet), newly presented with bilateral arm dysesthesias, and neck pain. On neurological examination, she exhibited no focal deficits. The cervical magnetic resonance (MR) showed a CM1 (i.e. 7 mm herniation of the cerebellar tonsils of below the foramen magnum), a C2-T5 syrinx, while the brain MR documented a pituitary adenoma [
Endocrine evaluation
The preoperative endocrine examination revealed that GH and insulin-like growth factor-1 (IGF-1) levels were elevated at 13.8–369 ng/ml, respectively. Further, the GH level was not suppressed after the oral glucose tolerance testing.
Surgery and postoperative course
The patient underwent a suboccipital/foramen magnum decompression (FMD), with C1 posterior arch resection. Postoperatively, her forearm dysesthesias improved. Due to the need to treat newly diagnosed colon cancer, the patient’s GH-producing pituitary lesion was managed medically (i.e. with a long-acting somatostatin analog therapy). The subsequent endocrine examination after somatostatin analog therapy revealed that her GH and IGF-1 levels declined to 3.27–100 ng/ml, respectively.
DISCUSSION
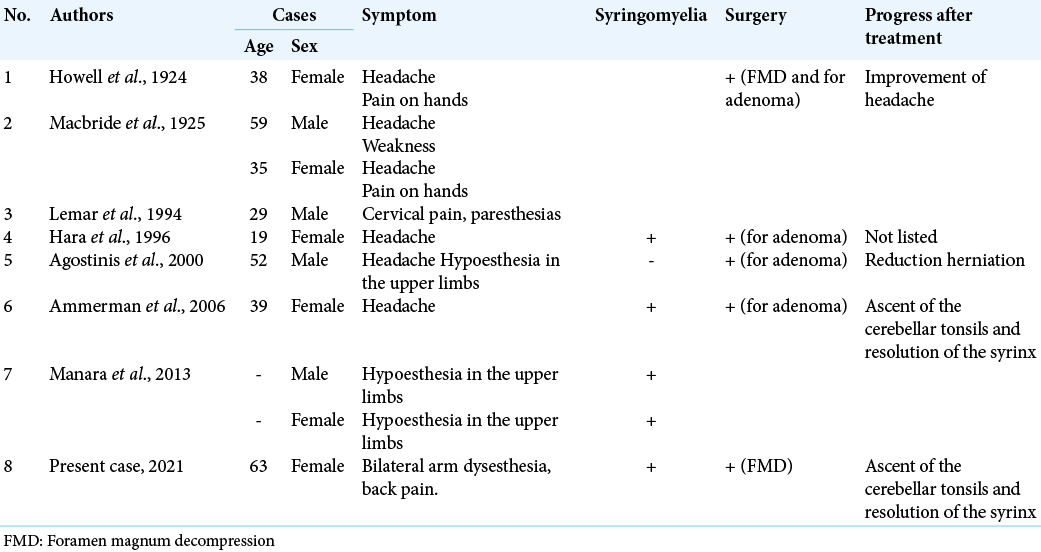
In this case, the patient had a CM1, an accompanying C2-T5 syrinx, and a GH-producing pituitary adenoma. The authors found nine similar cases in of the literature; notably, these combined pathologies further contributed to posterior fossa bony hypertrophy and increased narrowing of the foramen magnum [
CONCLUSION
Here, we presented a patient with a symptomatic CM1, syringomyelia, and a GH-producing pituitary adenoma (i.e. acromegaly). The former was effectively managed with a suboccipital/FMD, and C1 laminectomy, while the latter was treated with an endocrine therapy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank Enago (www.enago.jp) for the English language review.
References
1. Agostinis C, Caverni L, Montini M, Pagani G, Bonaldi G. “Spontaneous” reduction of tonsillar herniation in acromegaly: A case report. Surg Neurol. 2000. 53: 396-9
2. Ammerman JM, Goel R, Polin RS. Resolution of Chiari malformation after treatment of acromegaly. Case illustration. J Neurosurg. 2006. 104: 980
3. Gupta A, Vitali AM, Rothstein R, Cochrane DD. Resolution of syringomyelia and Chiari malformation after growth hormone therapy. Childs Nerv Syst. 2008. 24: 1345-8
4. Hara M, Ichikawa K, Minemura K, Kobayashi H, Suzuki N, Sakurai A. Acromegaly associated with Chiari-I malformation and polycystic ovary syndrome. Intern Med. 1996. 35: 803-7
5. Howell CM. Case of acromegaly and syringomyelia. Proc R Soc Med. 1924. 17: 54
6. Lemar HJ, Perloff JJ, Merenich JA. Symptomatic Chiari-I malformation in a patient with acromegaly. South Med J. 1994. 87: 284-5
7. Macbride HJ. Syringomyelia in association with acromegaly. J Neurol Psychopathol. 1925. 6: 114-22
8. Manara R, Bommarito G, Rizzati S, Briani C, Puppa AD, Citton V. Herniation of cerebellar tonsils in acromegaly: Prevalence, pathogenesis and clinical impact. Pituitary. 2013. 16: 122-30