- Department of Neurosurgery, Acute Services, Belfast Health and Social Care Trust, Royal Hospital, Northern Ireland, United Kingdom,
- National Centre for Neurosurgery, Beaumont Hospital, Beaumont Road, Dublin, Ireland.
DOI:10.25259/SNI_342_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Philip Thomas, Michael Amoo, Jack Horan, Mohammed Ben Husien, Derek Cawley, Jabir Nagaria, Ciaran Bolger. Technical outcome of atlantoaxial transarticular screw fixation without supplementary posterior construct for rheumatoid arthritis. 11-Jul-2020;11:188
How to cite this URL: Philip Thomas, Michael Amoo, Jack Horan, Mohammed Ben Husien, Derek Cawley, Jabir Nagaria, Ciaran Bolger. Technical outcome of atlantoaxial transarticular screw fixation without supplementary posterior construct for rheumatoid arthritis. 11-Jul-2020;11:188. Available from: https://surgicalneurologyint.com/surgicalint-articles/10130/
Abstract
Background: transarticular screw (TAS) fixation without a supplementary posterior construct, even in rheumatoid arthritis (RA) patients, provides sufficient stability with acceptable clinical results. Here, we present our experience with 15 RA patients who underwent atlantoaxial (AA) TAS fixation without utilizing a supplementary posterior fusion.
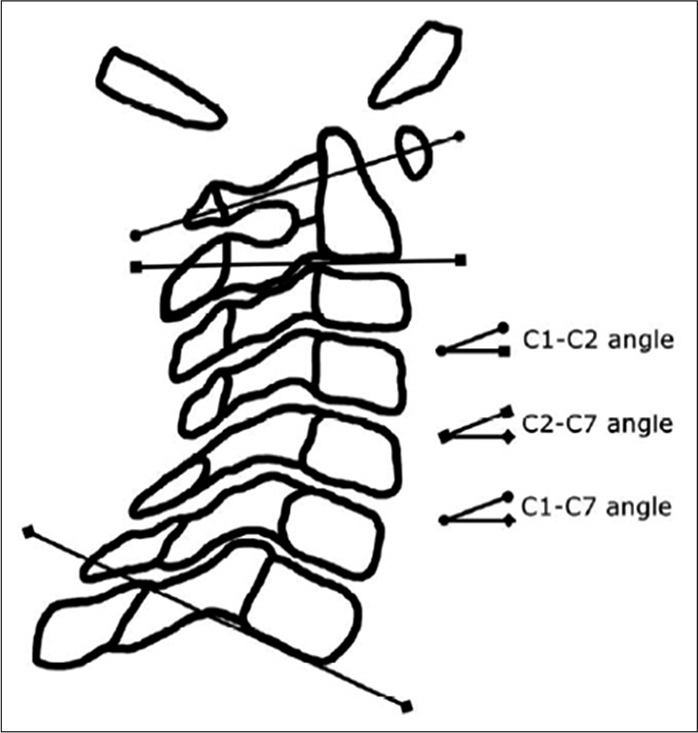
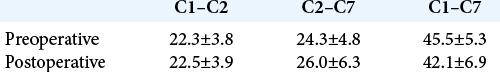
Methods: To treat AA instability, all 15 RA patients underwent C1–C2 TAS fixation without a supplementary posterior construct. Patients were followed for at least 24 months. Pre- and postoperative sagittal measures of C1– C2, C2–C7, and C1–C7 angles, atlanto-dens interval (ADI), posterior atlanto-dens interval (PADI), and adjacent segment (i.e., C2–C3) anterior disc height (ADH) were retrospectively recorded from lateral X-ray imaging. The presence or absence of superior migration of the odontoid (SMO), cervical subaxial subluxation, C1–C2 bony fusion, screw pull-out, and screw breakage were also noted.
Results: There was little difference between the pre- and postoperative studies regarding angles measured. Following TAS fixation, the mean ADI shortened, and mean PADI lengthened. There was no difference in the mean measures of C2–C3 ADH. There was no evidence of SMO pre- or postoperatively. Two patients developed anterior subluxation at C5–C6; one of the two also developed anterior subluxation at C2–C3. All patients subsequently showed C1–C2 bony fusion without screw pull-out or breakage.
Conclusion: In RA patients who have undergone C1–C2 TAS fixation, eliminating a supplementary posterior fusion resulted in adequate stability.
Keywords: Atlantoaxial, C1–C2, Rheumatoid arthritis, Transarticular screw fixation
INTRODUCTION
The instability of the atlantoaxial (AA) joint can result from aplasia or hypoplasia of the odontoid process, laxity of the transverse ligament, and assimilation of the atlas. AA can be associated with various conditions including Down’s syndrome, Klippel-Feil syndrome, osteogenesis imperfecta, neurofibromatosis, and rheumatoid arthritis (RA).[
Many spinal surgeons feel the current gold standard for posterior AA arthrodesis which is transarticular screw (TAS) fixation classically, achieved by the placement of a TAS screw from C2 to the anterior surface of C1 (across the facets, bilaterally).[
MATERIALS AND METHODS
We retrospectively evaluated the radiographs of 15 consecutive patients (13 females and 2 males), averaging 52 years of age (33–78 years) who underwent bilateral C1– C2 TAS fixation for the treatment of RA-associated AA instability.
Surgical technique
Preoperative planning for screw placement utilized CT-based StealthStation® image guidance (Medtronic Sofamor Danek, Memphis, TN). Parallel caudal stab incisions allowed for delivery of all instruments percutaneously to the posterior arch of C2; we used cannulated 3.5 mm diameter titanium screws (UCSS, Medtronic Sofamor Danek, Memphis, TN). The screw trajectory was confirmed intraoperatively under StealthStation® image guidance and fluoroscopy. Before operative closure, the C1–C2 facet joints were curetted and packed with morselized autologous iliac crest bone graft; no supplementary posterior construct was performed.
Follow-up
Patients were followed an average of 26 months (range 24– 39 months). Pre- and postoperative sagittal cervical X-rays measured; C1–C2, C2–C7, and C1–C7 angles [
RESULTS
Compared to the preoperative mean measures, there were no remarkable differences noted in the postoperative fixation, subaxial, and C-spine angles (i.e., the C1–C2, C2–C7, and C1–C7 angles, respectively) [
DISCUSSION
Satisfactory clinical outcomes are reported utilizing C1–C2 TAS fixation alone with RA.[
CONCLUSION
Technically satisfactory outcomes of AA segment arthrodesis can be achieved in RA patients using the TAS fixation technique without a supplementary posterior construct.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bahadur R, Goyal T, Dhatt SS, Tripathy SK. Transarticular screw fixation for atlantoaxial instability-modified Magerl’s technique in 38 patients. J Orthop Surg Res. 2010. 5: 87-
2. Crockard HA, Stevens JM. Craniovertebral junction anomalies in inherited disorders: Part of the syndrome or caused by the disorder?. Eur J Pediatr. 1995. 154: 504-12
3. Dreyer SJ, Boden SD. Natural history of rheumatoid arthritis of the cervical spine. Clin Orthop Relat Res. 1999. 366: 98-106
4. Haid RW, Subach BR, McLaughlin MR, Rodts GE, Wahlig JB. C1-C2 transarticular screw fixation for atlantoaxial instability: A 6-year experience. Neurosurgery. 2001. 49: 65-8
5. Magerl F, Seemann P, Kehr P, Weidner A.editors. Stable posterior fusion of the atlas and axis by trans-articular screw fixation. Cervical Spine. Vienna: Springer-Verlag; 1987. 1: 322-7
6. Mukai Y, Hosono N, Sakaura H, Fujii R, Iwasaki M, Fuchiya T. Sagittal alignment of the subaxial cervical spine after C1-C2 transarticular screw fixation in rheumatoid arthritis. J Spinal Disord Tech. 2007. 20: 436-41
7. Naderi S, Crawford NR, Song GS, Sonntag VK, Dickman CA. Biomechanical comparison of C1-C2 posterior fixations. Cable, graft, and screw combinations. Spine (Phila Pa 1976). 1998. 23: 1946-55
8. Nagaria J, Kelleher MO, McEvoy L, Edwards R, Kamel MH, Bolger C. C1-C2 transarticular screw fixation for atlantoaxial instability due to rheumatoid arthritis: A seven-year analysis of outcome. Spine (Phila Pa 1976). 2009. 34: 2880-5
9. Wang C, Yan M, Zhou H, Wang S, Dang G. Atlantoaxial transarticular screw fixation with morselized autograft and without additional internal fixation: Technical description and report of 57 cases. Spine (Phila Pa 1976). 2007. 32: 643-6
10. Yoshimoto H, Ito M, Abumi K, Kotani Y, Shono Y, Takada T. A retrospective radiographic analysis of subaxial sagittal alignment after posterior C1-C2 fusion. Spine (Phila Pa 1976). 2004. 29: 175-81