- Department of Neurosurgery, University of Puerto Rico, San Juan, United States.
Correspondence Address:
Orlando De Jesus, Department of Neurosurgery, University of Puerto Rico, San Juan, United States.
DOI:10.25259/SNI_64_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Orlando De Jesus, Ricardo J. Fernández-de Thomas, Caleb Feliciano. Tension pneumoventricle in a patient with a ventriculoperitoneal shunt and an ethmoidal meningoencephalocele. 13-May-2022;13:202
How to cite this URL: Orlando De Jesus, Ricardo J. Fernández-de Thomas, Caleb Feliciano. Tension pneumoventricle in a patient with a ventriculoperitoneal shunt and an ethmoidal meningoencephalocele. 13-May-2022;13:202. Available from: https://surgicalneurologyint.com/surgicalint-articles/11589/
Abstract
Background: Tension pneumoventricle is a rare, life-threatening complication. It has been rarely described in patients with ventriculoperitoneal (VP) shunts.
Case Description: A 28-year-old male patient with a VP shunt became progressively lethargic after falling from his wheelchair. Skull X-rays and head CT scan showed abundant air inside the ventricles. He was taken to the operating room, and the shunt was revised without improvement. Two days later, a frontal external ventricular drain was placed to remove the air. In the investigation toward the etiology of the pneumoventricle, a review of previous head CT scans and brain MRIs showed that the patient had a small left frontonasal meningoencephalocele extending into the ethmoid, which had been unnoticed. He underwent repair of the defect with adequate sealing of the frontal skull base.
Conclusion: In a shunted patient with moderate or severe symptoms from a tension pneumoventricle, external ventricular drainage is required to remove the air as the shunt is inadequate.
Keywords: Ethmoid, Meningoencephalocele, Pneumoventricle, Tension, Ventriculoperitoneal shunt
BACKGROUND
Intraventricular pneumocephalus, also known as pneumoventricle, is usually asymptomatic and does not need treatment if present in small amounts. However, tension pneumoventricle is a rare, life-threatening complication that can cause a decline in the neurological status.[
Tension pneumoventricle has been rarely described after placement of ventriculoperitoneal (VP) shunts.[
CASE DESCRIPTION
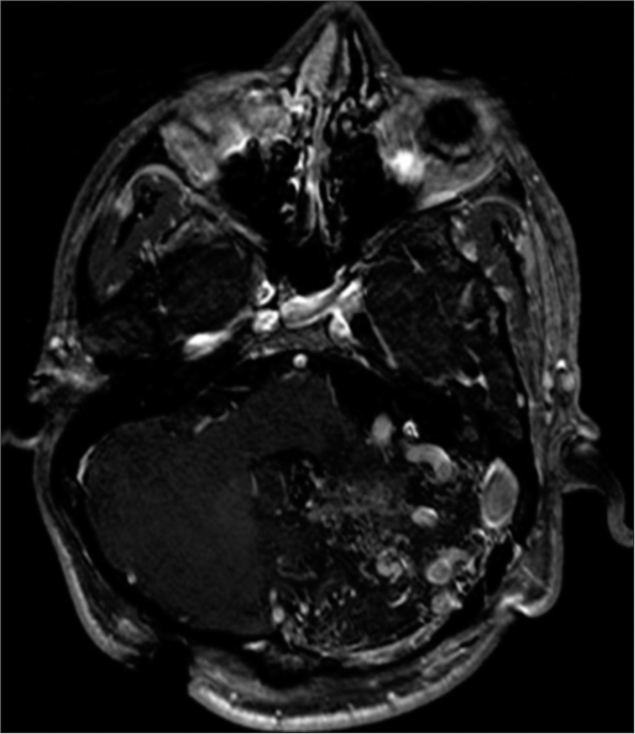
A 28-year-old male patient with a VP shunt suffered a fall from his wheelchair, for which he became progressively lethargic during the following 2 days. On evaluation, his neurological examination showed a Glasgow Coma Scale of 12. Eight years prior, he was diagnosed with a left cerebellar arteriovenous malformation during workup for headaches [
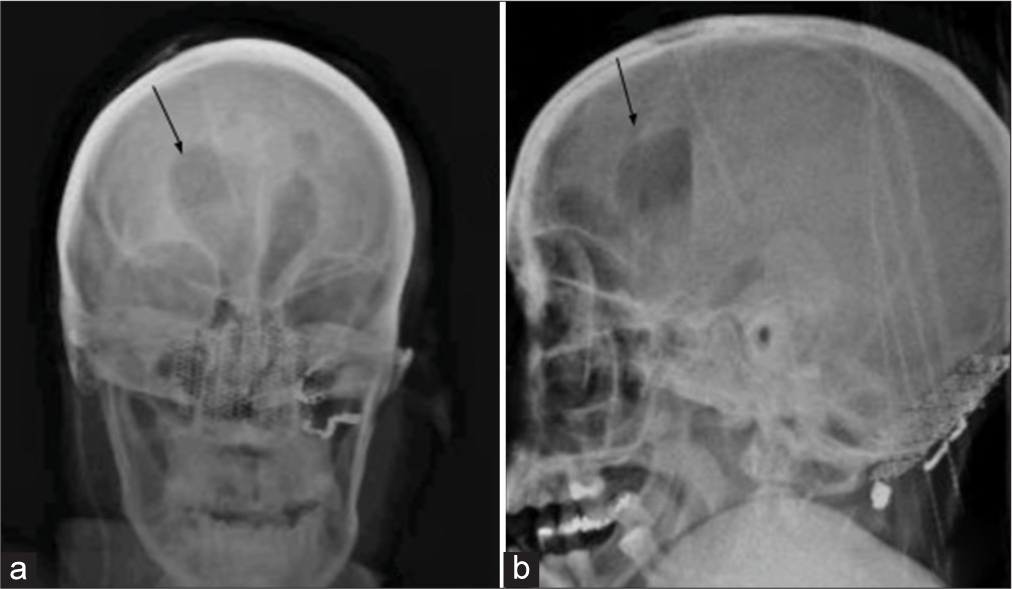
As the patient had a VP shunt, it was believed that the acute lethargic presentation was due to malfunctioning of the VP shunt or a traumatic brain injury secondary to the fall. Manual palpation of the shunt valve showed good pumping and refill. A radiological workup for the shunt malfunction was ordered. The skull X-rays showed abundant air inside the ventricles, and we thought that it could be the source of his symptoms [
During the surgery, it was found that the ventricular catheter was patent, and the valve had good distal flow, although a substantial amount of air inside the valve chamber. Air bubbles were observed draining together with a clear CSF when the valve was disconnected from the ventricular catheter. A new valve was placed, and the patient was admitted to the intensive care unit. No improvement was observed during the following 2 days, and a repeated head CT scan still showed a significant amount of pneumoventricle. He was returned to the operating room, and a frontal EVD was placed to remove the air trapped inside the ventricles. After 1 day, the EVD was kept closed to monitor the intracranial pressure. A subsequent head CT scan 6 days later showed resolution of the pneumoventricle and the EVD was removed when the second CSF culture was negative. No active evidence of a CSF leak was observed during the hospitalization.
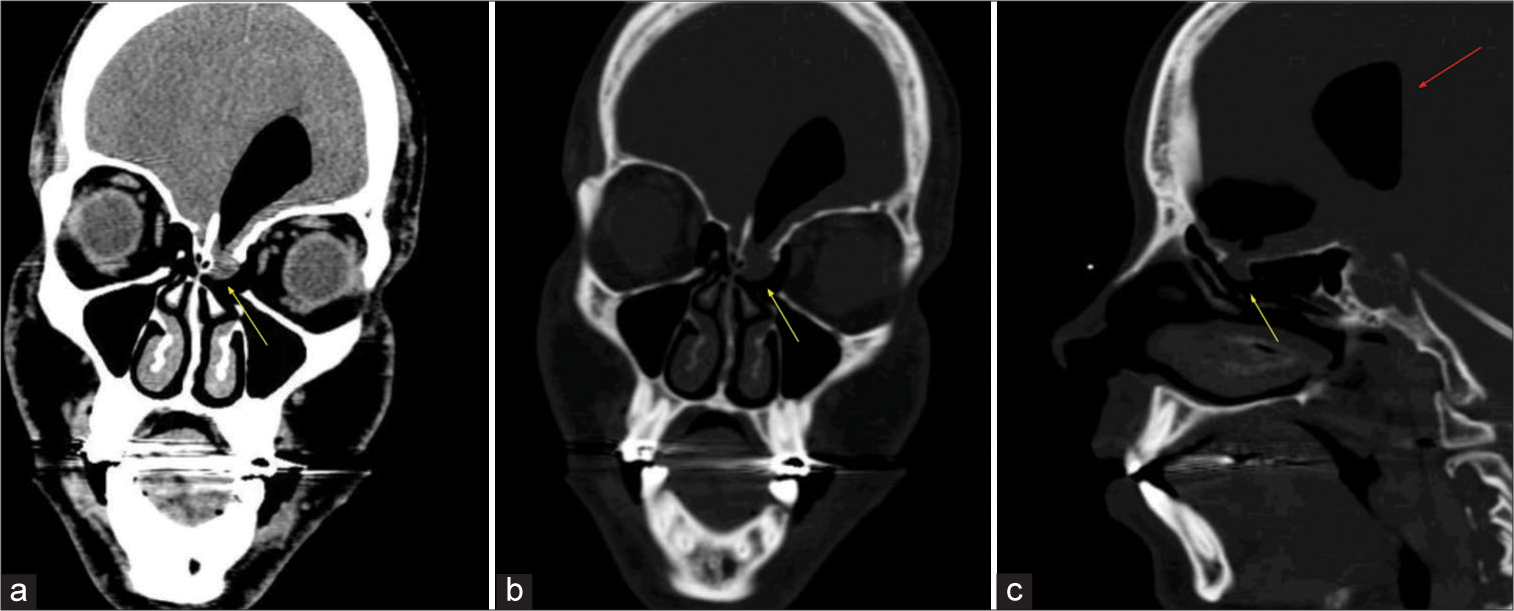
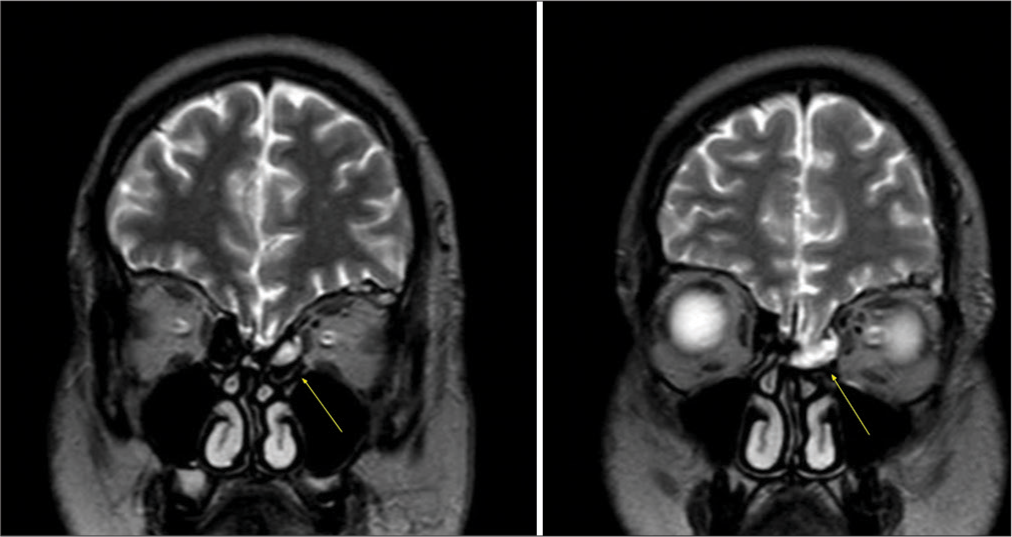
In our investigation toward the etiology of the pneumoventricle, a review of previous head CT scans and MRIs showed that the patient had a small left frontonasal meningoencephalocele extending into the ethmoid which had been previously unnoticed [
The otolaryngology department was consulted to repair the meningoencephalocele and frontal skull base defect. The patient underwent endoscopic endonasal removal of the meningoencephalocele with a reconstruction of the frontal skull base defect using an underlay cartilage patch placed at the defect and a vascularized nasoseptal mucosal graft placed in an overlay fashion. No postoperative lumbar drainage was used. The patient did not present any CSF leak postoperatively, and the head CT scan showed small-sized ventricles with no pneumoventricle. Six months after the resection of the meningoencephalocele and reconstruction of the skull base defect, he continues asymptomatic without evidence of a CSF leak.
DISCUSSION
In this case, the patient’s deterioration was initially thought to be secondary to the malfunction of the VP shunt. However, the valve pumped well and refilled quickly. At surgery, the shunt system was found to work adequately, although the air inside the valve chamber. We believe that the fall he sustained from the wheelchair caused the rupture of the arachnoid membrane of the meningoencephalocele occupying the frontal skull base defect. Due to the negative pressure produced by the shunt, air was forced into the brain and ventricles, causing the patient’s symptomatic presentation of tension pneumoventricle without evident rhinorrhea.
Cartwright and Eisenberg were the first to report on a tension pneumoventricle caused by the rupture of a basal encephalocele.[
CONCLUSION
Tension pneumoventricle is a rare but potentially life-threatening complication. In patients with moderate or severe symptoms, external ventricular drainage is required to remove the air. A skull base defect or meningoencephalocele can produce a tension pneumoventricle. Patients with VP shunts can also develop tension pneumoventricle. In these patients, the VP shunt may be incapable of removing air in large volumes to improve symptoms.
Declaration of the patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Almubarak AO, Fakhroo F, Alhuthayl MR, Kanaan I, Aldahash H. Tension pneumoventricle secondary to cutaneous-ventricular fistula: Case report and literature review. World Neurosurg. 2020. 142: 155-8
2. Ani CC, Ismaila BO. Tension pneumoventricle: A report of two cases. Niger J Clin Pract. 2016. 19: 559-62
3. Armocida D, Pesce A, Frati A, Miscusi M, Paglia F, Raco A. Pneumoventricle of unknown origin: A personal experience and literature review of a clinical enigma. World Neurosurg. 2019. 122: 661-4
4. Cartwright MJ, Eisenberg MB. Tension pneumocephalus associated with rupture of a middle fossa encephalocele. Case report. J Neurosurg. 1992. 76: 292-5
5. Chhiber SS, Nizami FA, Kirmani AR, Wani MA, Bhat AR, Zargar J. Delayed posttraumatic intraventricular tension pneumocephalus: Case report. Neurosurg Q. 2011. 21: 128-32
6. Ferrante L, Santoro A, Mastronardi L, Acqui M. Tension pneumocephalus after CSF shunting procedures. Br J Neurosurg. 1988. 2: 269-72
7. Garg N, Devi I, Dua R, Arivazhagan A. Tension pneumoventricle following exposure of shunt chamber. Br J Neurosurg. 2008. 22: 121-2
8. Gönül E, Yetişer S, Sirin S, Coşar A, Tasar M, Birkent H. Intraventricular traumatic tension pneumocephalus: A case report. Kulak Burun Bogaz Ihtis Derg. 2007. 17: 231-4
9. Lefranc M, Peltier J, Demuynkc F, Bugnicourt JM, Desenclos C, Fichten A. Tension pneumocephalus and rhinorrhea revealing spontaneous cerebrospinal fluid fistula of the anterior cranial base. Neurochirurgie. 2009. 55: 340-4
10. Lin YH, Lin HL, Cho DY. Tension pneumoventricle after endoscopic transsphenoidal surgery for rathke cleft cyst. World Neurosurg. 2020. 135: 228-32
11. Martinez-Perez R, Gómez E, Rayo N. Spontaneous tension pneumocephalus: A rare complication of shunting. World Neurosurg. 2017. 100: 710.e11-3
12. Mineo JF, Phong DH, Seizeur R, Mériot P, Besson G. Delayed isolated tension intraventricular pneumocephalus after ventriculoperitoneal shunt. Neurochirurgie. 2004. 50: 96-100
13. Mylonas C. Delayed pneumocephalus in patients with CSF shunts. Br J Neurosurg. 1991. 5: 67-72
14. Ohkawa T, Nakao N, Uematsu Y, Itakura T. Temporal lobe encephalocele in the lateral recess of the sphenoid sinus presenting with intraventricular tension pneumocephalus. Skull Base. 2010. 20: 481-6
15. Perrin RG, Bernstein M. Tension pneumoventricle after placement of a ventriculoperitoneal shunt: A novel treatment strategy. Case report. J Neurosurg. 2005. 102: 386-8
16. Ruiz-Juretschke F, Mateo-Sierra O, Iza-Vallejo B, Carrillo-Yagüe R. Intraventricular tension pneumocephalus after transsphenoidal surgery: A case report and literature review. Neurocirugia (Astur). 2007. 18: 134-7
17. Salem-Memou S, Vallee B, Jacquesson T, Jouanneau E, Berhouma M. Pathogenesis of delayed tension intraventricular pneumocephalus in shunted patient: possible role of nocturnal positive pressure ventilation. World Neurosurg. 2016. 85: 20.e17-20
18. Sasani M, Ozer FA, Oktenoglu T, Tokatli I, Sarioglu AC. Delayed and isolated intraventricular tension pneumocephalus after shunting for normal pressure hydrocephalus. Neurol India. 2007. 55: 81-2
19. Satapathy GC, Dash HH. Tension pneumocephalus after neurosurgery in the supine position. Br J Anaesth. 2000. 84: 115-7
20. Shaikh N, Chanda A, Hassan J, Al-Kubaisi A, Momin U, Alyafai A. Tension pneumoventricle: Reversible cause for aphasia. Qatar Med J. 2021. 2021: 15
21. Tsai JC, Cheng KY, Tsai ST, Tsai MJ. Tension pneumoventricle and cerebrospinal fluid rhinorrhea. QJM. 2017. 110: 39-40
22. Tuğcu B, Tanriverdi O, Günaldi O, Baydin S, Postalci LS, Akdemir H. Delayed intraventricular tension pneumocephalus due to scalp-ventricle fistula: A very rare complication of shunt surgery. Turk Neurosurg. 2009. 19: 276-80
23. Ugarriza LF, Cabezudo JM, Lorenzana LM, Porras LF, GarcíaYagüe LM. Delayed pneumocephalus in shunted patients. Report of three cases and review of the literature. Br J Neurosurg. 2001. 15: 161-7
24. Verhaeghe A, De Muynck S, Casselman JW, Vantomme N. Delayed intraventricular pneumocephalus following shunting for normal-pressure hydrocephalus. World Neurosurg. 2018. 116: 174-7