- Department of Neurosurgery, Airlangga University, – Dr. Soetomo General Academic Hospital, Surabaya, West Java, Indonesia.
- Department of Neurosurgery, Universitas Airlangga – Dr. Soetomo General Academic Hospital, Surabaya, West Java, Indonesia.
Correspondence Address:
Muhammad Faris, Department of Neurosurgery, Universitas Airlangga –Dr. Soetomo General Academic Hospital, Surabaya, West Java, Indonesia.
DOI:10.25259/SNI_708_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Galih Indra Permana1, Muhammad Faris2, Eko Agus Subagio2, Abdul Hafid Bajamal1. The effects of the coronavirus disease 2019 pandemic on neurospine surgery practice in the referral center hospital developing country. 20-Dec-2021;12:620
How to cite this URL: Galih Indra Permana1, Muhammad Faris2, Eko Agus Subagio2, Abdul Hafid Bajamal1. The effects of the coronavirus disease 2019 pandemic on neurospine surgery practice in the referral center hospital developing country. 20-Dec-2021;12:620. Available from: https://surgicalneurologyint.com/surgicalint-articles/11298/
Abstract
Background: The coronavirus disease 2019 (COVID-19) pandemic represents a once in a century challenge to human health care with over 4.5 million cases and over 300,000 deaths thus far. Surgical practice has been significantly impacted with all specialties writing guidelines for how to manage during this crisis. This study reported the effect of the COVID-19 pandemic on the neurosurgical practice, especially neurospine, in the outpatient visit, emergency department, and the surgical procedure.
Methods: This study is the comparative retrospective about neurospine practice in the outpatient visit, emergency department, and the surgical procedure among before and during COVID-19 pandemic. We recorded data from January to December 2019 (before COVID-19 pandemic) and compared with the same period in the 2020 (during a COVID-19 pandemic).
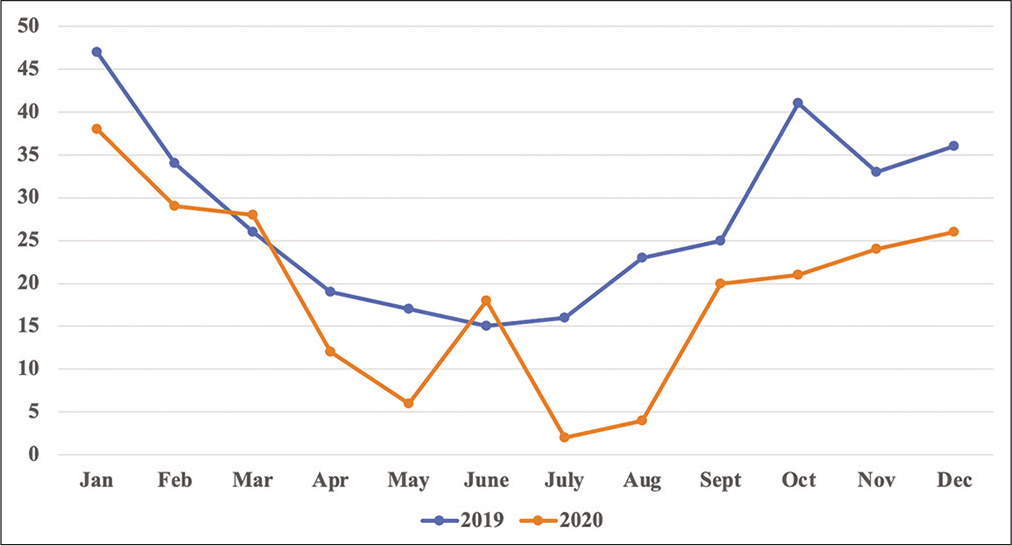
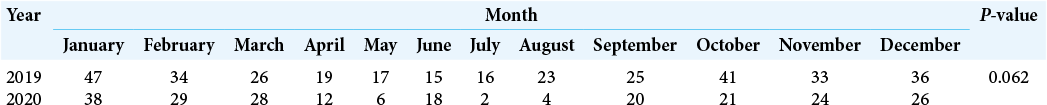
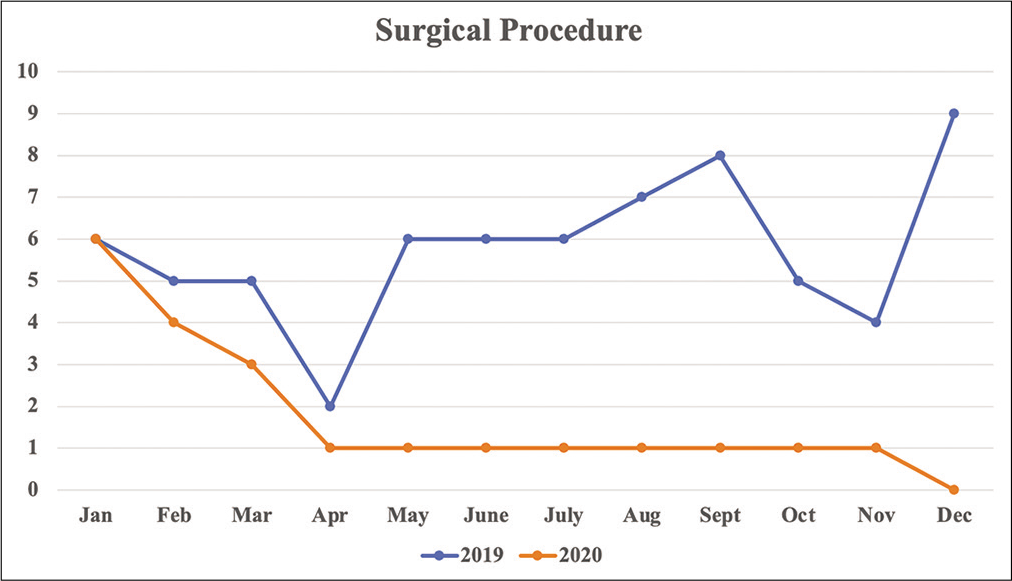
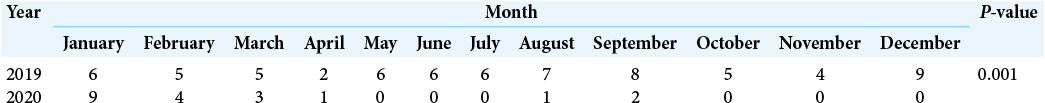
Results: A total of the outpatient visits, the average number per month was 28 ± 10.5 visits per month before the pandemic. The average number outpatient visit per month during the pandemic was 19 ± 11.1 visits per month, with the lowest in July 2020. The result of the average monthly neurospine surgical procedure before the pandemic was 5 ± 1.9 operations per month. Compared during the pandemic, there was decreased in the neurospine surgical procedure with the average number was 2 ± 2.7 operations per month. The decreased number significantly happens in the surgical procedure and emergency department patient (P P > 0.05).
Conclusion: The COVID-19 pandemic changed all scopes of medical practice and training. Considering the limitation in the available resources, the number of educational cases may decrease in subspecialized disciplines such as neurospine neurosurgery. The COVID-19 pandemic affects in the neurospine and neurosurgery treatment policy in the referral tertiary hospital.
Keywords: Coronavirus disease 2019, Developing country, Neurospine practice, Pandemic, Referral hospital
INTRODUCTION
A new type of virus that attacks the respiratory tract began in Wuhan, China, in late 2019 has spread across the world since then. The virus has caused an outbreak of viral pneumonia. The causative virus has been temporarily named as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the relevant infected disease has been named as coronavirus disease 2019 (COVID-19) by the World Health Organization.[
Dr. Soetomo General Academic Hospital is a tertiary referral hospital and a COVID-19 referral center in Surabaya, East Java, Indonesia. A lot of COVID-19 cases from the East Java region referred to this hospital to be treated. The neurosurgery department serves the health field of neurotrauma, neurovascular, neuro-oncology, neuropediatric, neurofunctional, and neurospine surgery. Many countries reported decreased in hospital treatment and outpatient since the COVID-19 pandemic.[
MATERIALS AND METHODS
This study used a retrospective case control with analytical observational. The sample method used a total population of the neurospine division from neurosurgery department that came to the clinic, emergency department, and inpatient care at the time from January to December 2019 and January to December 2020.
Group’s comparison was analyzed using the Kruskal–Wallis nonparametric comparative test. Statistical analysis was performed using the IBM SPSS Statistics for Mac version 26. The difference in the group of outpatient visit, emergency department visit, and surgery procedure was statistically calculated and considered significant if P < 0.05. This method was to compare the number of neurospine division patient before and after COVID-19 pandemic.
RESULTS
We collected the data from our hospital, Dr. Soetomo General Academic Hospital, as a tertiary referral hospital in Surabaya, East Java, Indonesia. The data were analyzed from the clinic, emergency department, and surgery of neurospine cases. This study compared the data from before pandemic COVID-19 (January–December 2019) and during pandemic COVID-19 (January–December 2020) in Indonesia. The result from before the pandemic showed the number patient in the outpatient visited, the average number per month was 28 ± 10.5 visits per month, with the lowest outpatient visit in June 2019 with 15 visits. The average number outpatient visit per month during the pandemic was 19 ± 11.1 visits per month, with the lowest in July 2020. The number of monthly neurospine outpatient visit is shown in [
During the pandemic period from January to December 2020, there was a decrease number of neurospine outpatient visit compared to the same period before pandemic in 2019, except in the June where the number of neurospine outpatient visit more than in the same month in the 2019 or before the pandemic. The comparable number of monthly neurospine outpatient visit before the pandemic and during the pandemic in the same period is shown in [
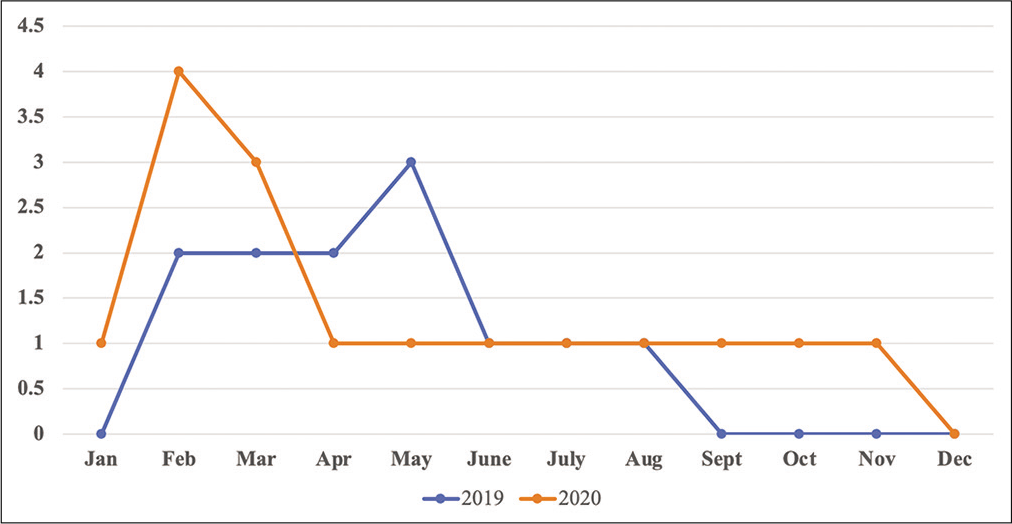
The number of the surgical procedure for the neurospine patient also decreased during the pandemic period in 2020 compared to the same period before the pandemic in 2019. The result of the average monthly neurospine surgical procedure before the pandemic was 5 ± 1.9 operations per month. Compared during the pandemic, there was decreased in the neurospine surgical procedure with the average number was 2 ± 2.7 operations per month. There was no neurospine surgical procedure in the May, June, July, October, November, and December during the pandemic period. The number of the monthly neurospine surgical procedure before and during the pandemic is shown in [
The decreased number also found in the emergency department visit of the neurospine patients during the pandemic period. Based on the data, [
Based on the result of the nonparametric Kruskal–Wallis comparative test for the number of neurospine outpatient visit during January–December in the pandemic period and before pandemic in the same month is not significant (P >0.05) differences in the number of neurospine outpatient visit. The comparable number of the surgical procedure before and during the pandemic is significantly different (P <0.05), which is higher neurospine surgical procedure before pandemic. The number of neurospine emergency patient significantly difference (P < 0.05) in the number between before pandemic and during the pandemic. Neurospine emergency patient decreased in the number during the pandemic compared to the before pandemic.
DISCUSSION
This study showed the decreased number of the neurospine outpatient visit during COVID-19 pandemic in the 2020 compared to the same period before COVID-19 pandemic in 2019. There was decreased in the number, but statistically no significant difference (P > 0.05). In June 2020, the number of neurospine outpatient visit is higher than before the pandemic. In the first 3 months, January–March 2020, the number of patients is still same as before pandemic. Because in our country, the increased cases of COVID-19 start in April 2020. There was no policy about public mobility restriction and hospital regulation about pandemic situation in the first 3 months during the pandemic. The decreased neurospine patient visit decreased in the rest of the month, which the lowest outpatient visit in July 2020. This month is the highest case of COVID-19, there was accumulation of COVID-19 cases in the hospital. All the resources were used to treat COVID-19 patients and there was a restriction policy in the outpatient visit.
Based on the statistical data, the number of neurospine surgical procedure and emergency department significantly decreased (P < 0.05) during the pandemic compare to the before the pandemic. In the first 3 months, the number of the neurospine surgical procedure is still same as before the pandemic. The rest of the month decreased significantly compared to before the pandemic. There was no neurospine surgical procedure in the May, June, July, October, November, and December. Some of the COVID-19 problem is human resources and ICU room usage. The ICU room usage decreased because used for COVID-19 patient and the medical personnel help treating COVID-19 patients. Some of the elective surgery was canceled and only emergency or urgent surgery performed. The number of emergency patient significantly decreased during the pandemic, even though before the pandemic, the neurospine emergency department visit is low. During the pandemic, there was only one patient in the January 2020 and there was no patient in the rest of the month. This decreased number can be caused by restriction policy of mobility and almost all the cases in the emergency department were COVID-19 cases. As one of the tertiary referral hospitals, almost all of the cases were referred to the Surabaya, include COVID-19. When our hospital unable to accept another case, all the cases from another hospital, especially neurospine, were delayed to refer.
In the 2nd week of June 2020, the Indonesia had performed a polymerase chain reaction swab test for COVID-19 on 514,287 specimens from 322,933 people. There were 38,277 confirmed cases of COVID-19, with 2134 cases of death. The death rate was eight people per 1 million populations. The new cases increased from 300 cases per day on average in April and May to 500 cases per day in June 2020. East Java Province was the region with the highest COVID-19 cases in Indonesia, and the cases were distributed unevenly in 38 cities and towns.[
Meybodi et al.[
There are two important things to be held in our practice, as others: (1) urgent or emergent cases should be managed anyway and (2) maximum protection of patients and staff is of great importance. Decision-making about testing asymptomatic patients should be customized based on many factors related to the patients, society, medical centers, and the type of surgery. In our country with restricted resources, testing all the patients may not be cost effective; therefore, performing the diagnostic test for the symptomatic patients and with the high risk is the standard.[
Postponing elective surgeries are not only a reasonable strategy and it seems to be the only rational path for neurosurgeons until the end of the pandemic. The data from our US respondents indicated that even within the short 2 weeks of the principal study, the date of the response was a positive predictor of both the hospitals’ response and neurosurgeons’ opinion toward more stringent shutdowns.[
CONCLUSION
The number of neurospine patient in the clinic, emergency department, and surgical operation procedure decreased during the pandemic compared to the before pandemic in the same period. The COVID-19 pandemic changed all scopes of medical practice and training. Considering the limitation in the available resources, the number of educational cases may decrease in subspecialized disciplines such as neurospine neurosurgery. The COVID-19 pandemic affects in the neurospine and neurosurgery treatment policy in the referral tertiary hospital.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Al-Jabir A, Kerwan A, Nicola M, Alsafi Z, Khan M, Sohrabi C. Impact of the Coronavirus (COVID-19) pandemic on surgical practice-Part 2 (surgical prioritisation). Int J Surg. 2020. 79: 233-48
2. Burks JD, Luther EM, Govindarajan V, Shah AH, Levi AD, Komotar RJ. Early changes to neurosurgery resident training during the COVID-19 pandemic at a large U.S. academic medical center. World Neurosurg. 2020. 144: e926-33
3. de Simone B, Chouillard E, Sartelli M, Biffl WL, di Saverio S, Moore EE. The management of surgical patients in the emergency setting during COVID-19 pandemic: The WSES position paper. World J Emerg Surg. 2021. 16: 14
4. Díaz-Bello S, Hernández-Hernández A, Guinto-Nishimura GY, Mondragón-Soto MG, Lem-Carrillo M, González-Aguilar A. Reconversion of neurosurgical practice in times of the SARS-CoV-2 pandemic: A narrative review of the literature and guideline implementation in a Mexican neurosurgical referral center. Neurosurg Focus. 2020. 49: E4
5. Jean WC, Ironside NT, Sack KD, Felbaum DR, Syed HR. The impact of COVID-19 on neurosurgeons and the strategy for triaging non-emergent operations: A global neurosurgery study. Acta Neurochir (Wien). 2020. 162: 1229-40
6. Kibbe MR. Surgery and COVID-19. JAMA. 2020. 324: 1151-2
7. Meredith JW, High KP, Freischlag JA. Preserving elective surgeries in the COVID-19 pandemic and the future. JAMA. 2020. 324: 1725-6
8. Meybodi KT, Habibi Z, Nejat F. The effects of COVID-19 pandemic on pediatric neurosurgery practice and training in a developing country. Child’s Nerv Syst. 2021. 37: 1313-7
9. Setyono H, Alifianto U, Wijanarko F, Ramadhana GA, Putra GS, Putra MD. The impact of the pandemic on neurosurgical services: A study from a coronavirus disease 2019 referral hospital in Surakarta. Surg Neurol Int. 2021. 12: 128
10. Suryaningtyas W, Wahyuhadi J, Turchan A, Subagio EA, Parenrengi MA, Apriawan T. Neurosurgery at the epicenter of the COVID-19 pandemic in Indonesia: Experience from a Surabaya academic tertiary hospital. Neurosurg Focus. 2020. 49: E5