- Department of Neurosurgery, Allegheny General Hospital, Pittsburgh,
- Department of Surgery, Penn State Health Milton S. Hershey Medical Center, Hershey, Pennsylvania, United States.
DOI:10.25259/SNI_29_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Gordon Mao, Michael Joseph Gigliotti, Derrick Dupre. The use of hospital consumer assessment of healthcare services and the Press Ganey medical practice surveys in guiding surgical patient care practices. 18-Jul-2020;11:192
How to cite this URL: Gordon Mao, Michael Joseph Gigliotti, Derrick Dupre. The use of hospital consumer assessment of healthcare services and the Press Ganey medical practice surveys in guiding surgical patient care practices. 18-Jul-2020;11:192. Available from: https://surgicalneurologyint.com/surgicalint-articles/10136/
Abstract
Background: Patient satisfaction questionaries have become popular in the past decade after the institution of the Patient Care and Affordable Care Act of 2010. This study evaluated whether the Hospital Consumer Assessment of Healthcare Services (H-CAHPS) and Press Ganey scores improved after institutional changes to the rounding system.
Methods: In the summer of 2017, utilizing H-CAHPS and Press Ganey scores, we asked whether switching from mid-level rounding providers to resident physicians improved patient care. Pre- and post-intervention groups, each lasting four quarters, were divided into care provided by mid-level personnel versus residents. For these periods, H-CAHPS respondent data were compared by a Chi-squared test (P t-test (P
Results: Significant improvement was noted in patients answering “Definitely yes” in recommending our institution in both H-CAHPS and Press Ganey satisfaction surveys. Significant improvement regarding the speed of discharge, instructions for post-hospital care, and the overall rating of care given was observed in the Press Ganey responses alone.
Conclusion: Significant improvement in satisfaction was noted in the Press Ganey responses regarding the discharge process and speed of discharge. The quality of this last encounter likely contributed to+ the significant improvement observed in both the H-CAPHS and Press Ganey Scores for an overall hospital stay and the percentage of those definitely recommending our institution.
Keywords: Hospital Consumer Assessment of Healthcare Services, Neurosurgery, Outcomes, Press Ganey
INTRODUCTION
Beginning in 2010 with the Patient Care and Affordable Care Act, the Centers of Medicare and Medicaid Services (CMS) identified “patient experience of care” as one of the five domains in an Accountable Care Organization (ACO).[
Two commonly used surveys, including the Hospital Consumer Assessment of Healthcare Services (H-CAHPS) and the Press Ganey Medical Practice Survey, are useful to quantify abstract and complex concepts.[
MATERIALS AND METHODS
Providers utilized for patient care
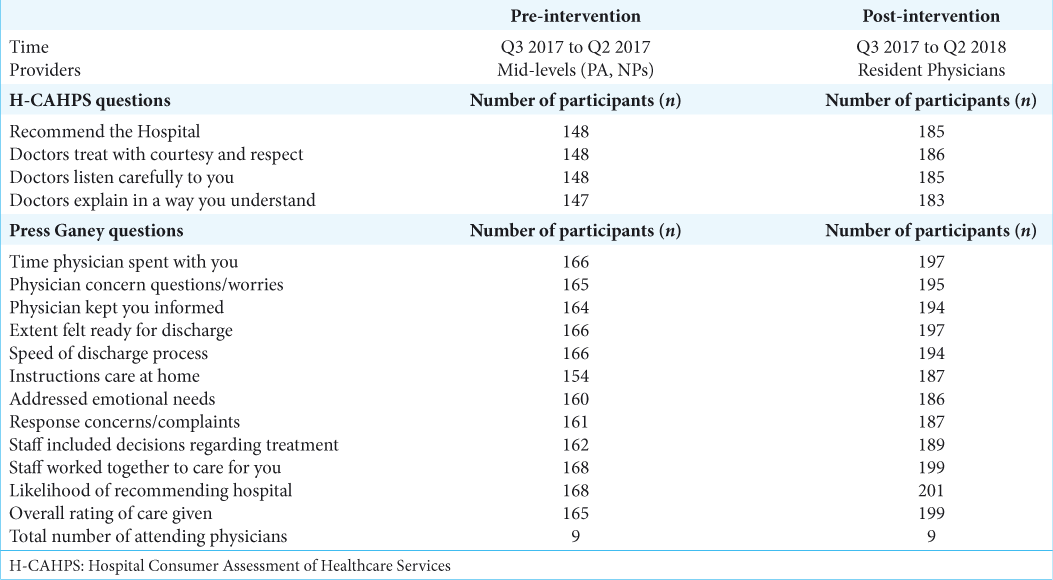
Our department quality initiative was to study the impact of resident rounding on floor patients and participation in the discharge process. Previously, mid-level providers (nurse practitioners and physicians assistants) handled a majority of the floor duties and discharges. The study period lasted from 2016 to 2018, covering a pre- and post-intervention period of 1 year [
Hospital consumer assessment of healthcare services versus Press Ganey questionnaire
H-CAHPS and Press Ganey scores were reviewed beginning in the third quarter of 2016 through the second quarter of 2018. Five questions were taken from the H-CAHPS survey and were divided into pre-intervention and post-intervention groups. Twelve questions were taken from Press Ganey surveys and also divided into pre- and post-intervention groups. Responses were divided into “Definitely Yes” versus “All Other Responses” to allow for statistical analysis [
Control group and exclusion criteria
Average H-CAHPS and Press Ganey scores from the same nine attending physicians were utilized as a control throughout all quarters measured. Case type and associated patient satisfaction scores were excluded from the analysis.
Statistical analysis
H-CAHPS scores were analyzed categorically and were reported as counts and percentages. Statistical analysis was performed using MedCalc version 13.1.0 (MedCalc Statistical Software BVBA, Ostend, Belgium) and charts were created utilizing Microsoft Excel 2010 (Microsoft Corporation, Redmond, Washington). A threshold level of P < 0.05 was considered statistically significant.
Press Ganey responses were analyzed categorically and presented as means with concurrent standard deviations. A threshold value of P < 0.05 was considered statistically significant. Ninety-five percentage CI was reported for the question results deemed statically significant.
RESULTS
Hospital consumer assessment of healthcare services
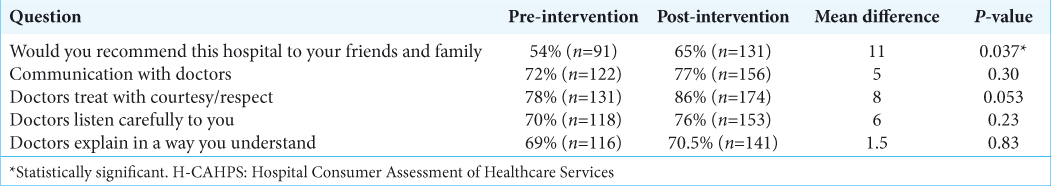
For the survey question “Recommend the hospital,” the proportion of survey participants that responded “Definitely yes” in the post-intervention period was statistically significant when compared to the pre-intervention period (P = 0.037). However, no statistical significance was observed in the following response categories: “Communication with doctors,” “Doctors treat with courtesy/respect,” “Doctors listen carefully to you,” and “Doctors explain in a way you understand.” Complete H-CAHPS data with corresponding P-values are included in [
Press Ganey medical practice survey
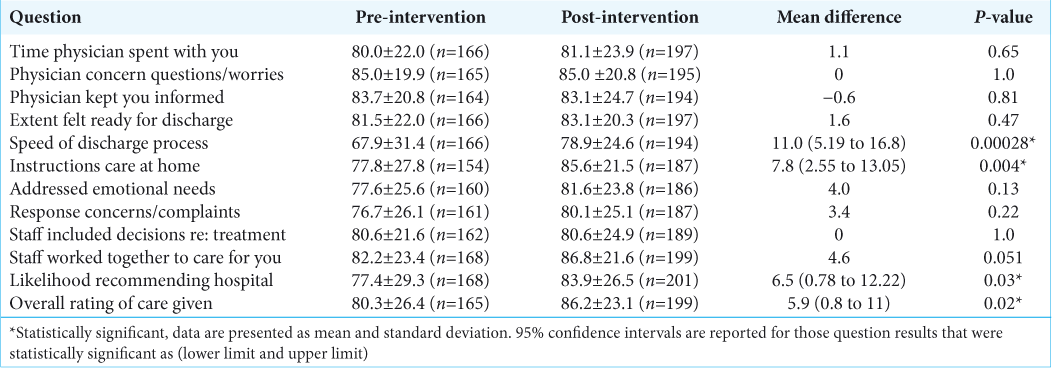
Twelve categories of the Press Ganey medical practice survey were analyzed. For questions “Likelihood of recommending the hospital” and “Overall rating of care given,” responses of “Definitely yes” versus “All other responses” were significant in the post-intervention group (P = 0.03 and P = 0.02, respectively). Patients responding with “Definitely yes” in the “Speed of discharge process” and “Instructions for care at home” were also significantly improved (P = 0.00028 and P = 0.004, respectively). The patient response to “Staff worked together to care for you,” approached significance (0.051). Complete Press Ganey questionnaire data are included in [
DISCUSSION
After the passage of the Patient Care and Affordable Care Act of 2010, the Joint Commission for the Accreditation of Healthcare Organizations mandated that health systems measure quality outcome indicators.[
The patient satisfaction significantly improved in five H-CAHPS and Press Ganey domains when placing an increased emphasis on a physician-centered care model. Furthermore, the H-CAHPS question “Doctors treat you with courtesy” approached significance, and so there may be a higher perceived level of respect and less opportunity for miscommunication when patients are seen by physicians as opposed to physician extenders.
Approximately 98,000 deaths occur annually in U.S. hospitals as a direct result of medical errors.[
A dissatisfied patient is less likely to remain loyal to a specific healthcare facility, be compliant with treatment, or participate in self-health maintenance.[
However, the linkage between neurosurgical procedures, outcome, and patient satisfaction may be problematic. Many extraneous factors play a role in patient response and satisfaction rates, as previous studies have pointed out that age, ethnicity, culture, personality, family support, and other factors have a significant influence on intended outcomes.[
CONCLUSION
Here, using both Hospital Consumer Assessment of Healthcare Services (H-CAHPS) and the Press Ganey Medical Practice Surveys, we documented that direct resident contact with patients throughout their hospital stay improved patient satisfaction. This supports the notion that changing healthcare delivery in neurosurgical residency programs, with an emphasis on resident physician input inpatient care, can be a factor in improving patient satisfaction outcomes.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Davis BA, Kiesel CK, Mcfarland J, Collard A, Coston K, Keeton A. Evaluating instruments for quality: Testing convergent validity of the consumer emergency care satisfaction scale. J Nurs Care Qual. 2005. 20: 364-8
2. Etier BE, Orr SP, Antonetti J, Thomas SB, Theiss SM. Factors impacting Press Ganey patient satisfaction scores in orthopedic surgery spine clinic. Spine J. 2016. 16: 1285-9
3. Glickman SW, Boulding W, Manary M, Staelin R, Roe MT, Wolosin RJ. Patient satisfaction and its relationship with clinical quality and inpatient mortality in acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2010. 3: 188-95
4. Petrullo KA, Lamar S, Nwankwo-Otti O, Alexander-Mills K, Viola D. The patient satisfaction survey: What does it mean to your bottom line?. J Hosp Adm. 2012. 2: 1-8
5. Press I, Fullam F. Patient satisfaction in pay for performance programs. Qual Manag Health Care. 2011. 20: 110-5
6. Rogers F, Horst M, To T, Rogers A, Edavettal M, Wu D. Factors associated with patient satisfaction scores for physician care in trauma patients. J Trauma Acute Care Surg. 2013. 75: 110-5
7. Santuzzi NR, Brodnik MS, Rinehart-Thompson L, Klatt M. Patient satisfaction. Qual Manag Health Care. 2009. 18: 3-18
8. Schmocker RK, Holden SE, Vang X, Lumpkin ST, Stafford LM, Leverson GE. The number of inpatient consultations is negatively correlated with patient satisfaction in patients with prolonged hospital stays. Am J Surg. 2016. 212: 282-8