- Department of Neurosurgery, Yokohama City University, Yokohama, Japan.
- Department of Orthopedics, Yokohama City University, Yokohama, Japan.
- Department of Pathology, Yokohama City University, Yokohama, Japan.
Correspondence Address:
Yohei Miyake, Department of Neurosurgery, Yokohama City University, Yokohama, Japan.
DOI:10.25259/SNI_113_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Chihiro Oka1, Yohei Miyake1, Kensuke Tateishi1, Yusuke Kawabata2, Hiromichi Iwashita3, Tetsuya Yamamoto1. Thigh leiomyosarcoma-derived brain metastasis with intracerebral hematoma: A case report and literature review. 03-Mar-2023;14:80
How to cite this URL: Chihiro Oka1, Yohei Miyake1, Kensuke Tateishi1, Yusuke Kawabata2, Hiromichi Iwashita3, Tetsuya Yamamoto1. Thigh leiomyosarcoma-derived brain metastasis with intracerebral hematoma: A case report and literature review. 03-Mar-2023;14:80. Available from: https://surgicalneurologyint.com/surgicalint-articles/12178/
Abstract
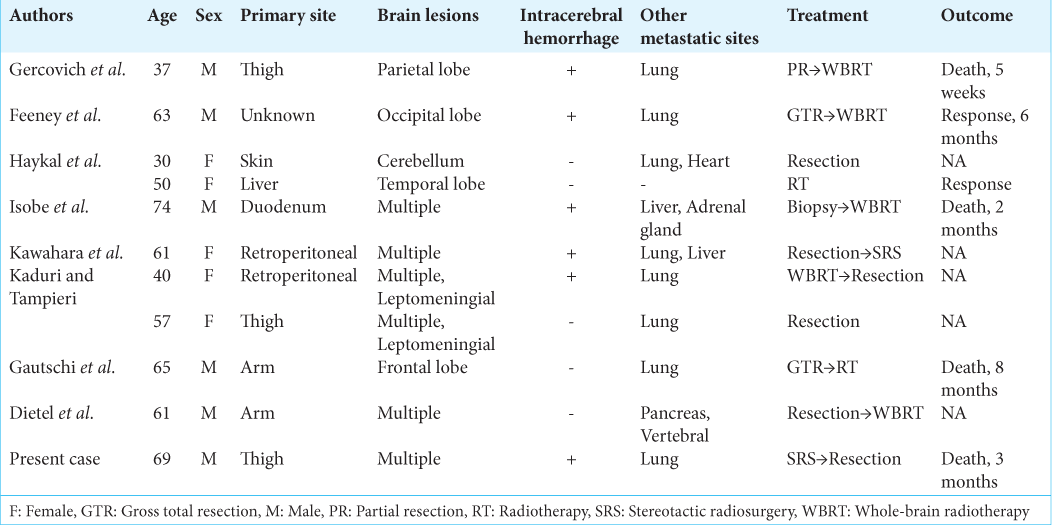
Background: Brain metastases with hematoma are clinically important as they indicate the potential for rapid neurological deterioration. Non-uterine leiomyosarcoma-derived brain metastases are particularly rare, and their clinical features, including the bleeding rate, are unclear. Herein, we present a rare case of thigh leiomyosarcoma-derived brain metastasis with intratumoral hematoma and review previous case reports.
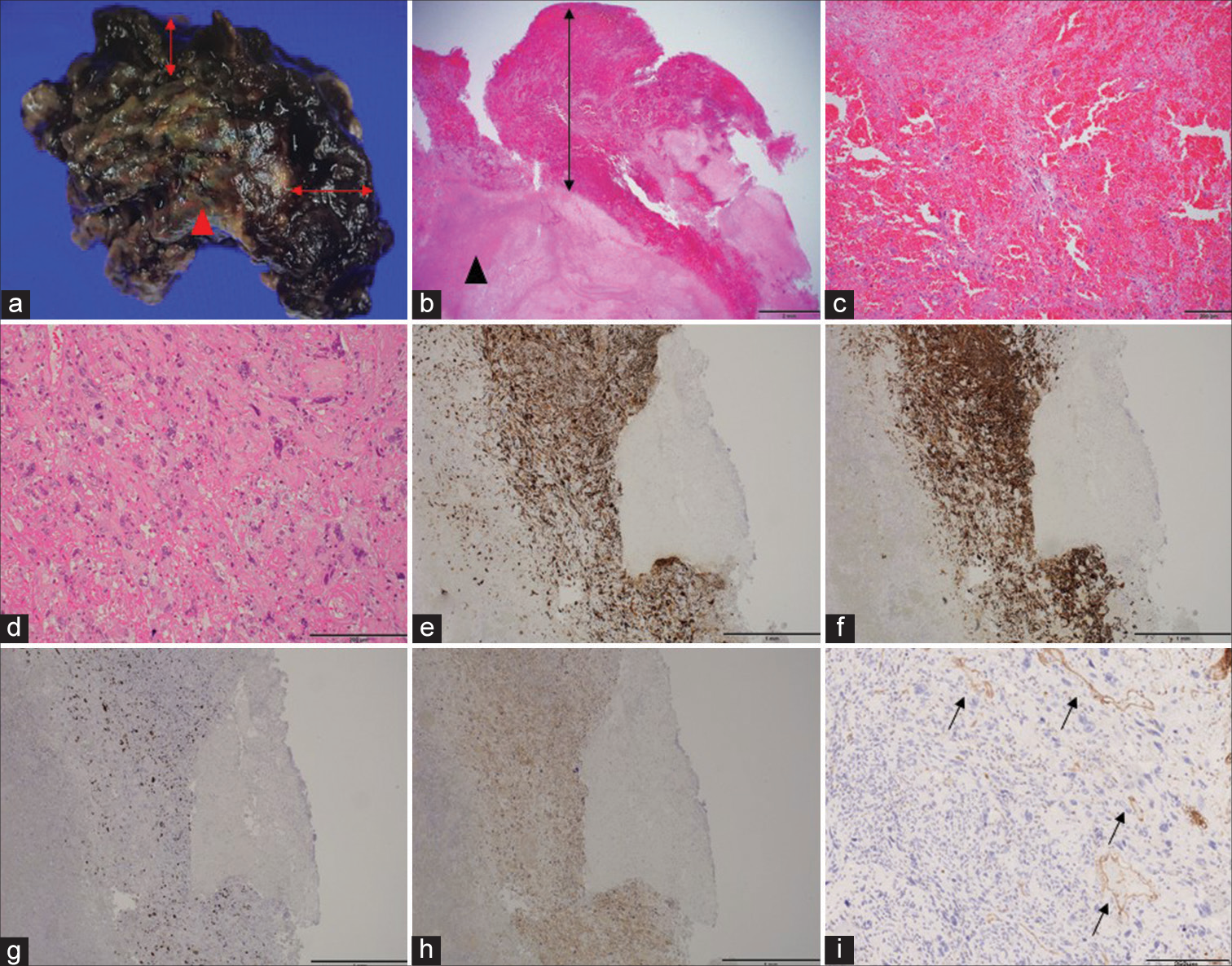
Case Description: A 68-year-old man with a right thigh leiomyosarcoma presented with multiple brain metastases. The patient received stereotactic radiotherapy; however, he reported sudden right-sided hemiparesis. We found a right frontal irradiated lesion with intratumoral hemorrhage and performed gross total tumor resection. Histopathological examination showed highly atypical cells with prominent necrosis and hemorrhage. Abnormal thin-walled vessels were prominent within the brain tumor, and vascular endothelial growth factor was diffusely expressed immunohistopathologically. To date, 11 cases of brain metastasis from non-uterine leiomyosarcoma, including the present case, have been reported. Of note, six patients had hemorrhage. Three out of six patients presented with hemorrhage before therapeutic intervention, three cases were from residual sites after surgery or radiation.
Conclusion: More than half the patients with non-uterine leiomyosarcoma-derived brain metastases presented with intracerebral hemorrhage. Furthermore, these patients are at risk of developing rapid neurological deterioration due to intracerebral hemorrhage.
Keywords: Brain metastasis, Hemorrhage, Non-uterine leiomyosarcoma
INTRODUCTION
Brain metastases occasionally present with intratumoral bleeding, especially in renal cell carcinoma and malignant melanoma.[
CASE REPORT
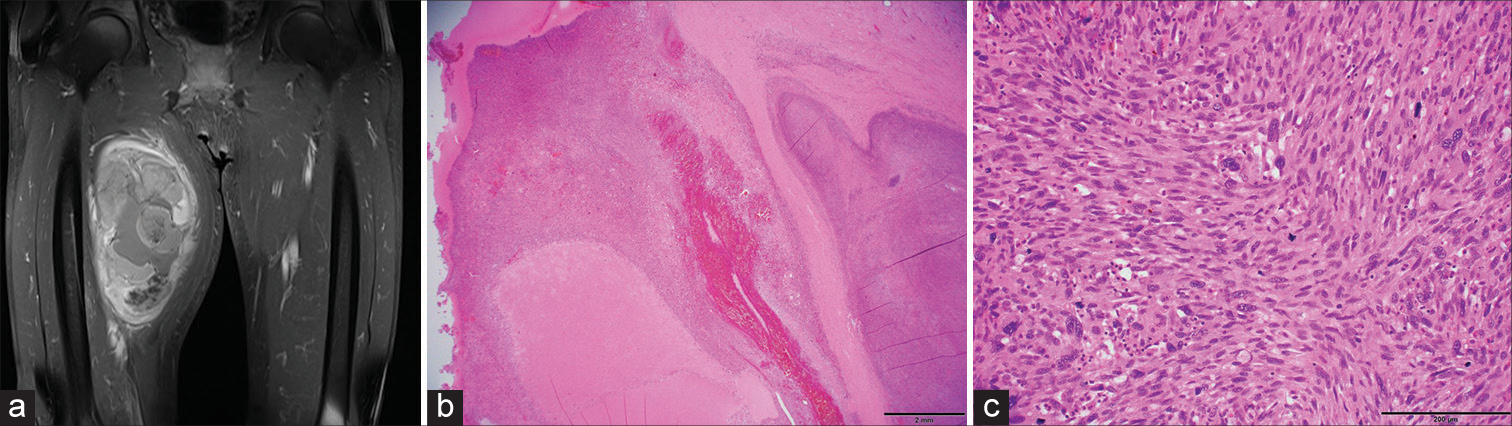
A 68-year-old man presented with swelling on the right thigh. Magnetic resonance imaging (MRI) revealed a contrast-enhanced tumor with a hemorrhagic and unclear border [
Figure 1:
Clinicopathological features of the thigh leiomyosarcoma. Gadolinium-enhanced T1-weighted magnetic resonance imaging demonstrating a heterogeneously enhanced tumor in the right thigh (a), hematoxylin and eosin staining indicate dense tumor cell proliferation with necrosis and hemorrhage (b), and tumors showing spindle cells with highly pleomorphic nuclei (c).
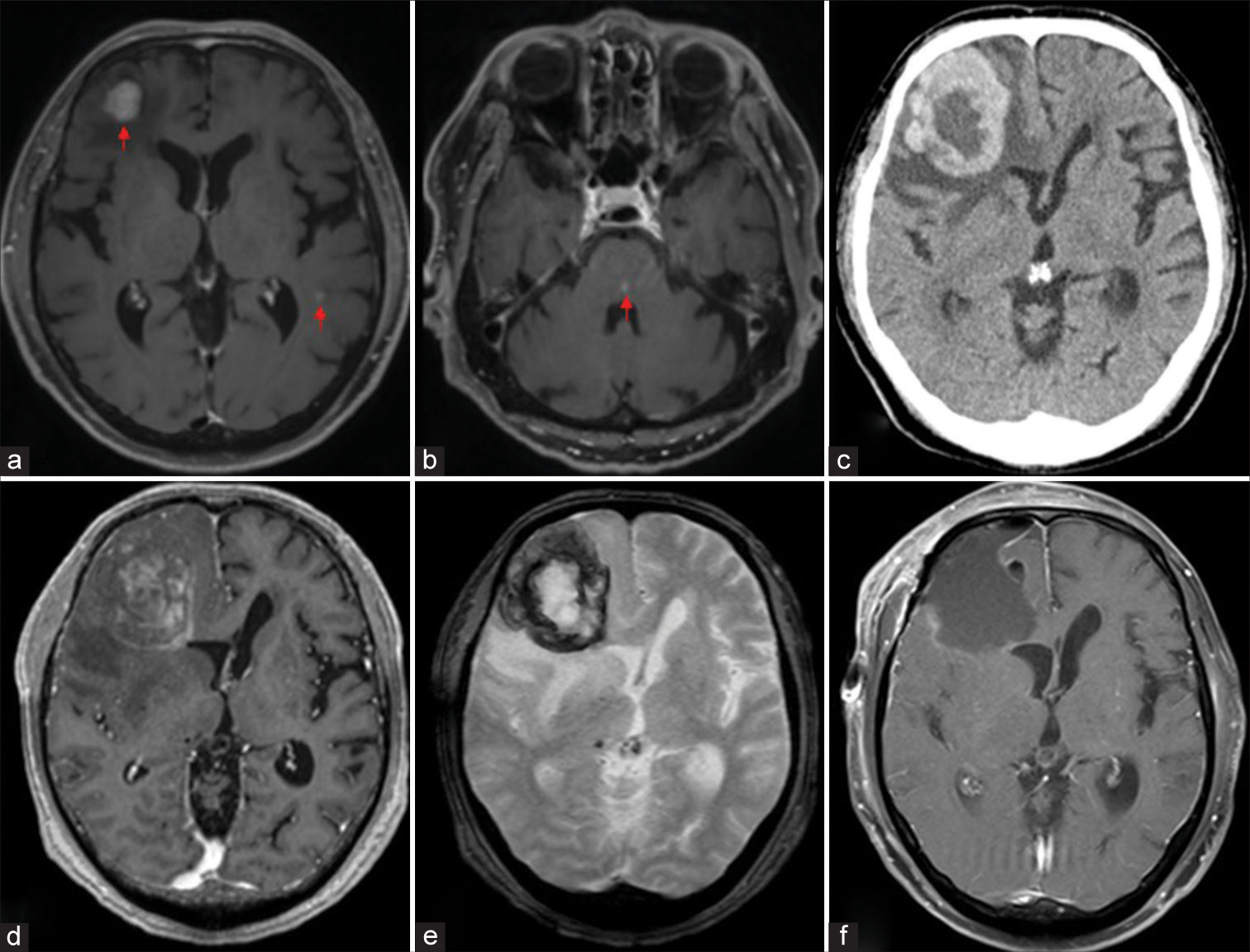
Figure 2:
Radiographic features of the metastatic brain tumor derived from leiomyosarcoma of the thigh. Gadolinium-enhanced T1-weighted magnetic resonance imaging (MRI) demonstrating multiple brain tumors (a and b, arrows). Computed tomography and MRI showing the right frontal tumor with a surrounding hematoma (c-e). MRI indicating total resection of the tumor (f).
Figure 3:
Pathological characteristics of the metastatic brain tumor derived from leiomyosarcoma of the thigh. Macroscopic view showing the tumor (arrowhead) and the surrounding hematoma (arrows) (a). Hematoxylin and eosin staining indicates diffuse growth of atypical cells with necrosis (arrowhead) and hemorrhage (arrows) (b). Hemorrhage comprising tumor cells (c). Tumor cells showing spindle and epithelioid features with highly pleomorphic nuclei (d). Immunostaining for desmin (e), caldesmon (f), Ki-67 (g), vascular endothelial growth factor (h), and CD31 (i). Thin-walled vessels are prominent within the tumor (i, arrows).
DISCUSSION
Leiomyosarcoma is a soft-tissue sarcoma that occurs in the uterus, gastrointestinal tract, blood vessels, and extremities.[
Notably, six (54.5%) patients demonstrated co-occurrence of brain metastases with hemorrhagic components.[
Although the underlying mechanisms of hemorrhage within brain tumors are unclear, abnormal tumor vessels, such as thin-walled, poorly formed, or dilated vessels, may contribute to intratumoral hemorrhage.[
In our patient, the small lesions disappeared after stereotactic radiotherapy, except for a 2 cm lesion in the right frontal lobe. Similarly, whole-brain irradiation controlled the small lesions, but the most significant lesion, measuring 2 cm, grew and required resection.[
CONCLUSION
We reported a rare case of thigh leiomyosarcoma-derived brain metastasis. The majority of non-uterine leiomyosarcoma-derived brain metastases present with intracerebral hemorrhage even after treatment. These findings suggest that non-uterine leiomyosarcoma-derived brain metastases may pose a risk of rapid neurological deterioration due to intracerebral hemorrhage and require early therapeutic intervention.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Amant F, Coosemans A, Debiec-Rychter M, Timmerman D, Vergote I. Clinical management of uterine sarcomas. Lancet Oncol. 2009. 10: 1188-98
2. Dietel E, Nestler U, Nenning H, Eisenloffel C, Stassart R, Meixensberger J. A late systemic and brain metastasis from subcutaneous leiomyosarcoma of the right forearm: A case report and review of the literature. J Med Case Rep. 2021. 15: 14
3. Donato J, Campigotto F, Uhlmann EJ, Coletti E, Neuberg D, Weber GM. Intracranial hemorrhage in patients with brain metastases treated with therapeutic enoxaparin: A matched cohort study. Blood. 2015. 126: 494-9
4. Espat NJ, Bilsky M, Lewis JJ, Leung D, Brennan MF. Soft tissue sarcoma brain metastases. Prevalence in a cohort of 3829 patients. Cancer. 2002. 94: 2706-11
5. Feeney JJ, Popek EJ, Bergman WC. Leiomyosarcoma metastatic to the brain: Case report and literature review. Neurosurgery. 1985. 16: 398-401
6. Gautschi OP, Hottinger AF, Lobrinus JA, Schaller K, Bijlenga P. Isolated cerebral metastasis of a triceps muscle leiomyosarcoma: A case report. Br J Neurosurg. 2014. 28: 400-2
7. George S, Serrano C, Hensley ML, Ray-Coquard I. Soft tissue and uterine leiomyosarcoma. J Clin Oncol. 2018. 36: 144-50
8. Gercovich FG, Luna MA, Gottlieb JA. Increased incidence of cerebral metastases in sarcoma patients with prolonged survival from chemotherapy. Report of cases of leiomysarcoma and chondrosarcoma. Cancer. 1975. 36: 1843-51
9. Haykal HA, Wang AM, Zamani A. Leiomyosarcoma metastatic to the brain: CT features and review. AJNR Am J Neuroradiol. 1985. 8: 911-2
10. Isobe N, Oki S, Sumida M, Kanou Y, Nabika S, Watanabe Y. Metastatic leiomyosarcoma of the brain manifesting as multiple hemorrhages. Case report. Neurol Med Chir (Tokyo). 2005. 45: 44-8
11. Jung S, Moon KS, Jung TY, Kim IY, Lee YH, Rhu HH. Possible pathophysiological role of vascular endothelial growth factor (VEGF) and matrix metalloproteinases (MMPs) in metastatic brain tumor-associated intracerebral hemorrhage. J Neurooncol. 2006. 76: 257-63
12. Kaduri S, Tampieri D. Leiomyosarcoma leptomeningeal brain metastases. Neuroradiol J. 2012. 25: 587-92
13. Kawahara I, Fujimoto T, Ono T, Takahata H, Toda K, Tsutsumi K. Multiple cerebral metastasis of a retroperitoneal leiomyosarcoma. Brain Nerve. 2012. 64: 565-9
14. Kawasaki K, Hamamoto Y, Fukada J, Adachi M, Sasaki H, Takaishi H. Fatal hemorrhage in a patient with advanced soft tissue sarcoma following radiation and pazopanib treatment: A case report. Oncol Lett. 2016. 11: 2408-10
15. Lee V, Jairam V, Yu JB, Park HS. Nationwide patterns of hemorrhagic stroke among patients hospitalized with brain metastases: Influence of primary cancer diagnosis and anticoagulation. Sci Rep. 2020. 10: 10084
16. Ostrowski RP, He Z, Pucko EB, Matyja E. Hemorrhage in brain tumor-an unresolved issue. Brain Hemorrhages. 2022. 3: 98-102
17. Pakos EE, Goussia AC, Tsekeris PG, Papachristou DJ, Stefanou D, Agnantis NJ. Expression of vascular endothelial growth factor and its receptor, KDR/Flk-1, in soft tissue sarcomas. Anticancer Res. 2005. 25: 3591-6