- Department of Neurosurgery, UT Houston, Houston, Texas, United States.
- UT Health Houston, McGovern Medical School, UT Houston, Houston, Texas, United States.
Correspondence Address:
Laura A. Zima, Department of Neurosurgery, UT Houston, Houston, Texas, United States.
DOI:10.25259/SNI_512_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Laura A. Zima1, Subhiksha Srinivasan2, Brad Budde1, Ryan Kitagawa1. Thirty-two nails injected into the head: An operative report and review of the literature. 26-Aug-2022;13:377
How to cite this URL: Laura A. Zima1, Subhiksha Srinivasan2, Brad Budde1, Ryan Kitagawa1. Thirty-two nails injected into the head: An operative report and review of the literature. 26-Aug-2022;13:377. Available from: https://surgicalneurologyint.com/surgicalint-articles/11834/
Abstract
Background: Self-inflicted nail gun injuries are a rare phenomenon that can result in traumatic damage. The velocity of the nail is generally fast enough to penetrate the skull. However, the extent of damage depends on the exact angle and structures of the brain encountered by the nails.
Case Description: A 55-year-old male presented with 32 nails in the head and was found down. Initially, the patient presented with localization but had to be intubated soon after due to declining condition. This report describes the operative technique for safe removal of all nails, separated into six categories based on location and structures of the brain encountered. A review of literature revealed potential complications such as hemorrhage and infections and how to protect against these undesired effects.
Conclusion: Self-inflicted nail gun head injuries are an uncommon form of traumatic head injury. Some important tools that helped prevent our patient from developing major complications included stereotactic navigation, antibiotic prophylaxis, and angiography to carefully monitor for vascular injuries.
Keywords: Neurotrauma, Penetrating trauma, Sinus injury
INTRODUCTION
We describe a unique case of 32 independent nails to the head. The surgical technique to remove the nail depends on the penetration depth, trajectory, and surrounding structures. We review the operative set up and technique in detail for six different types of nail injuries encountered and review the relevant literature. All nails, including two through the superior sagittal sinus, were safely removed.
Nail gun injuries are associated with several important potential complications. One is the formation of a traumatic pseudoaneurysm. A 50% mortality rate in the event of a rupture has been reported, therefore, performing arteriograms a week or two after injury are helpful, especially in patients with a subarachnoid hemorrhage or hematoma.[
CASE REPORT
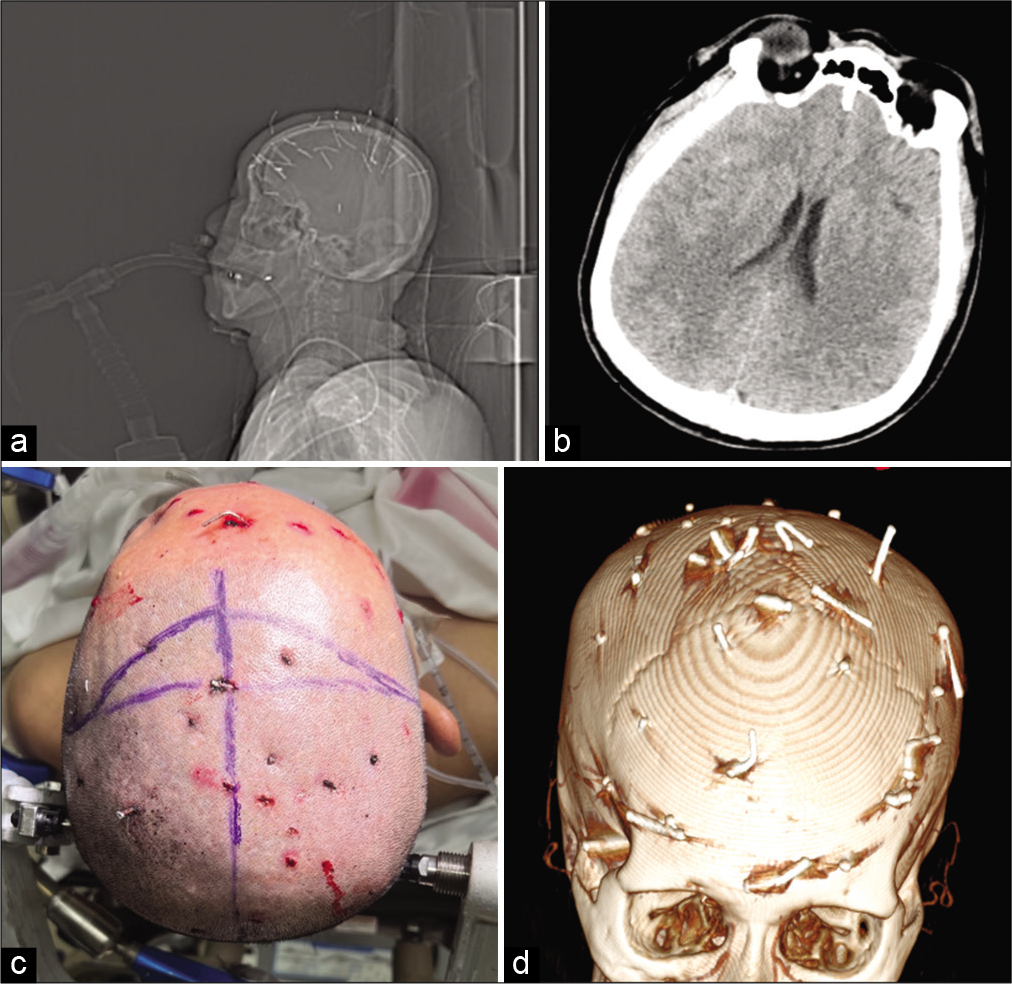
The patient is a 55-year-old male who presented after being found down with nail injuries including multiple shots to the head. The patient was reportedly localizing on the scene but subsequently deteriorated and was intubated. Representative images on arrival are shown in
Operative technique
The patient was placed in the supine position in a Mayfield head holder with care to avoid placement of the pins into any of the fractures. Stereotactic image guidance was used to locate each nail and evaluate the trajectory and ultrasound was used to evaluate for intracerebral hemorrhage (ICH). A microscope was present for removal of the nails through the superior sagittal sinus. A bicoronal incision that was bisected posteriorly was used to access to all of the nails from a single operative approach.
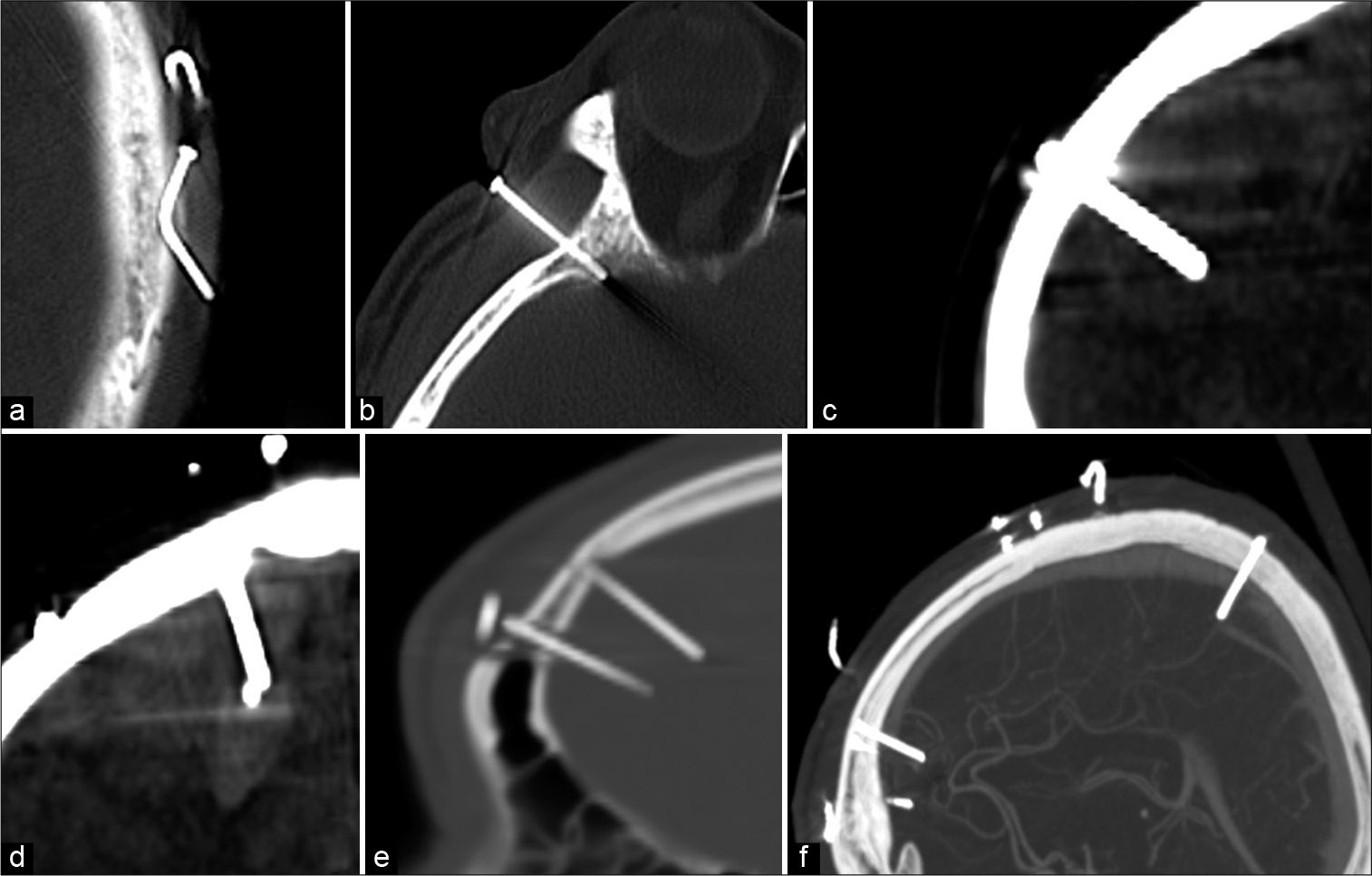
Representative images of each nail type are shown in
Figure 2:
Seven types of nails described, under skin but not involving other structures not pictured. (a) Into bone but does not violate dura, (b) into brain but uncomplicated, (c) into surface vessel, (d) into brain with underlying hematoma, (e) through air sinus (frontal sinus), and (f) through blood sinus.
Type 1: Nail under the skin but not penetrating the skull
This group is the most simple for removal, but this type is also the most likely to be left behind at the conclusion of the surgery. In our case, the skin was opened in its entirety first and any nails were removed directly. The overlying skin defect was closed with suture, and at the case conclusion, we obtain fluoroscopic imaging to ensure that none of these nails were left behind. This type of nail removal may also be performed at the bedside under local anesthesia if open surgical intervention is not otherwise needed.
Type 2: Nail penetrating the skull but not violating the dura
The next group of nails was those that went into the bone but did not violate the dura. This type of nail was confirmed with both preoperative imaging and image guidance before extraction. They were then removed and the holes were sealed using bone wax and the entrance wound sutured in case there were microperforations of the dura that could lead to cerebrospinal fluid (CSF) leakage. This type of nail could be removed at the bedside as well.
Type 3: Dural penetration without underlying hematoma
Multiple nails penetrated the dura and pia without underlying hematoma on preoperative imaging. A single burr hole followed by a 2–3 cm circular craniectomy was performed around the nail. Excessive nail movement was avoided and the bone flap was elevated in the nail trajectory as determined by image guidance. Any surface vascular hemorrhage was controlled followed by ultrasonography to ensure no ICH. The dura is opened followed by pial hemostasis. In this case, all of the nails were sequentially removed and a final ultrasound was performed at all sites to ensure no delayed hematoma before craniectomy reconstruction.
Type 4: Dural penetrating with underlying hematoma
The same procedure was performed for the nail removal as was done when there was no underlying hematoma initially. One nail was associated with an underlying subdural hematoma which was able to be evacuated through the small craniectomy. Another nail was associated with a <3 cm ICH visualized with ultrasound. The craniectomy was expanded and the hemorrhage was evacuated with ultrasound guidance through the original cortical violation of the nail.
Type 5: Penetration through an air sinus
The next type of nail that was encountered was through both the inner and outer tables of the frontal sinus. The craniectomy was performed superior to the frontal sinus and the dura was dissected away from the posterior table. The nail was removed and hemostasis was obtained. The ultrasound confirmed no underlying hematoma. The anterior table was sealed using bone wax and the posterior table was isolated from the dural violation with vascularized pericranial graft. A complete cranialization of the frontal sinus was not needed given the small defect.
Type 6: Penetration through the superior sagittal sinus
These lesions have the most risk for hemorrhage and complications. Although the anterior sinus injuries are less dangerous given the ability to ligate the sinus if needed, the treatment is the same. A craniectomy with exposure of the sinus anterior and posterior to the nail is performed. The dura ipsilateral to the nail exit site is opened and the exit of the nail from the sinus is visualized with the operative microscope. The nail and bone flap are removed and the internal and external sinus defects are packed with foam-based hemostatic products and Cottonoid patties. This technique was effective in our case, but ligation or reconstruction of the sinus may be necessary in unique cases.
Ultrasound and fluoroscopy were performed before cranial reconstruction with titanium mesh to ensure no retained nails or operative hematomas. The patient had a postoperative venogram which demonstrated patent superior sagittal sinus. The patient was discharged home with the right hemiparesis.
DISCUSSION
Treatment of self-inflicted nail gun injuries to the head varies based on the penetration level and structures affected. In most cases, the speed of a nail dislodged from a nail gun allows penetration of the skull.[
Our case represents a unique situation in which 32 separate nails were encountered which fit into six different categories: under skin but not involving other structures, into bone but does not violate dura, into brain but uncomplicated, into brain with underlying hematoma, through air sinus (frontal sinus), and through blood sinus. While the previous case reports have described management of self-inflicted nail gun head injuries, this report separates the nails encountered into categories based on location of the nail penetration.
In general, subcutaneous nail gun injuries not involving other structures can easily be removed at bedside in a sterile manner using local anesthesia.[
Occasionally, the nail may penetrate an air sinus. A previous case by Patchana et al. describes a nail extending through the maxillary sinus into the skull base and right frontal lobe.[
Although this case did not involve large vessel arterial injury, the previous literature has described a case of penetration of the basilar artery. Englot et al. presented a 51-year-old male with a nail gun head injury who presented with a subarachnoid hemorrhage and occlusion of the basilar artery.[
Another possible area of injury involves the venous sinuses. Nail gun injury to the superior sagittal sinus requires careful management required to prevent life-threatening bleeding.[
Common complications of nail gun head injuries include meningitis, CSF leak, and cerebral abscesses.[
CONCLUSION
We describe a unique case of 32 independent nails to the head. We describe the operative technique for the removal of six broad categories of nails; under skin but not involving other structures, into bone but does not violate dura, into brain but uncomplicated, into brain with underlying hematoma, through air sinus (frontal sinus), and through blood sinus. Key points include use of stereotactic navigation to evaluate each nail, ultrasound to evaluate for intraparenchymal hemorrhage intraoperatively, and fluoroscopy to assure all nails are removed.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Arici L, Akgün B, Kaplan M, Yılmaz I. Penetrating head trauma with four nails: An extremely rare case. Ulus Travma Acil Cerrahi Derg. 2012. 18: 265-7
2. Bayston R, de Louvois J, Brown EM, Johnston RA, Lees P, Pople IK. Use of antibiotics in penetrating craniocerebral injuries. “Infection in neurosurgery” working party of British society for antimicrobial chemotherapy. Lancet. 2000. 355: 1813-7
3. Carnevale JA, Morrison JF, Choi DB, Klinge PM, Cosgrove GR, Oyelese AA. Self-inflicted nail-gun injury with cranial penetration and use of intraoperative computed tomography. Surg Neurol Int. 2016. 7: S259-62
4. Englot DJ, Laurans MS, Abbed K, Bulsara KR. Removal of nail penetrating the basilar artery. Neurosurg Rev. 2010. 33: 501-4
5. Ferraz VR, Aguiar GB, Vitorino-Araujo JL, Badke GL, Veiga JC. Management of a low-energy penetrating brain injury caused by a nail. Case Rep Neurol Med. 2016. 2016: 4371367
6. Isaacs AM, Yuh SJ, Hurlbert RJ, Mitha AP. Penetrating intracranial nail-gun injury to the middle cerebral artery: A successful primary repair. Surg Neurol Int. 2015. 6: 152
7. Min SH, Kweon C-young, Shin W. Penetrating brain injury caused by a nail gun. Nerve. 2017. 3: 81-4
8. Patchana T, Taka TM, Ghanchi H, Wiginton J, Wacker M. Case report: Projectile into right frontal lobe from a nail gun. Cureus. 2020. 12: e9460
9. Selvanathan S, Goldschlager T, McMillen J, Campbell S. Penetrating craniocerebral injuries from nail-gun use. J Clin Neurosci. 2007. 14: 678-83
10. Sim SK, Theophilus SC, Noor Azman AR. Multiple nail gun penetrating head injury: A case report. IIUM Med J Malaysia. 2013. 12: 514
11. Testerman GM, Dacks LM. Multiple self-inflicted nail gun head injury. South Med J. 2007. 100: 608-10
12. Wang AS, Zeng MH, Wang F. Successful treatment of a nail gun injury in right parietal region and superior sagittal sinus. J Craniofac Surg. 2021. 32: 1297-301
13. Ye CN, Lin MC, Huang CL. Double penetration wound: A nail gun injury involving the head and heart. Radiol Case Rep. 2020. 15: 334-8
14. Yuh SJ, Alaqeel A. Ten self-inflicted intracranial penetrating nail gun injuries. Neurosciences (Riyadh). 2015. 20: 267-70
15. Zhu RC, Yoshida MC, Kopp M, Lin N. Treatment of a self-inflicted intracranial nail gun injury. BMJ Case Rep. 2021. 14: e237122