- Department of Neurological Surgery, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, United States.
- Department of Neurosurgery, Tulane Medical Center, New Orleans, Louisiana, United States.
Correspondence Address:
Hussam Abou-Al-Shaar, Department of Neurological Surgery, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, United States.
DOI:10.25259/SNI_535_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Justin Beiriger1, Hussam Abou-Al-Shaar1, Hansen Deng1, Mansour Mathkour2, David O. Okonkwo1. Thoracic intramedullary neurosarcoidosis with thoracic disc herniation: Diagnostic importance of intramedullary contrast enhancement. 06-Jul-2021;12:331
How to cite this URL: Justin Beiriger1, Hussam Abou-Al-Shaar1, Hansen Deng1, Mansour Mathkour2, David O. Okonkwo1. Thoracic intramedullary neurosarcoidosis with thoracic disc herniation: Diagnostic importance of intramedullary contrast enhancement. 06-Jul-2021;12:331. Available from: https://surgicalneurologyint.com/surgicalint-articles/10947/
Abstract
Background: Thoracic intramedullary neurosarcoidosis is an uncommon but serious manifestation of spinal cord disease. Its concomitant occurrence with thoracic disc herniation can mislead the physician into attributing neurologic and radiographic findings in the spinal cord to disc pathology rather than inflammatory disorder. Here, we present such a rare case of concomitant thoracic disc and spinal neurosarcoidosis.
Case Description: A 37-year-old male presented with progressive right lower extremity weakness and numbness. Magnetic resonance imaging (MRI) of the thoracic spinal cord revealed a T6-T7 paracentral disc eccentric to the right with T2 signal change extending from T2 to T10 level. This prompted acquiring a contrasted MRI that also depicted intramedullary enhancement around the T6-T7 disc bulge. Computed tomography scan of the chest showed mediastinal lymphadenopathy concerning for sarcoidosis. Lymph node biopsy confirmed the diagnosis of sarcoidosis, and high-dose steroid treatment was initiated. The patient had significant symptomatic improvement with steroids with full neurological recovery and improvement of his symptoms.
Conclusion: While stenosis from thoracic disc disease could potentially suggest a mechanical etiology for the patient’s symptoms, attention must be paid to the imaging findings as well as the degree and extent of cord signal change and intramedullary contrast enhancement. Appropriate and timely diagnosis is essential to avoid unnecessary invasive procedures.
Keywords: Cord edema, Intramedullary, Neurosarcoidosis, T2 signal change, Thoracic disc, mimickers
INTRODUCTION
Sarcoidosis is a well-described inflammatory granulomatous disease that affects multiple organ systems. Involvement of the central nervous system is present in approximately 25% of cases; however, it remains subclinical in the majority of patients.[
Spinal neurosarcoidosis is particularly difficult to diagnosis due to its rarity and nonspecific clinical presentation, which can be indistinguishable from other etiologies. Radiographic findings can frequently be nondiagnostic. However, the classic pattern that suggests a diagnosis of spinal neurosarcoidosis is T2 hyperintensity and contrast enhancement within the central spinal cord.[
CASE REPORT
Clinical presentation
A 37-year-old otherwise healthy African-American male presented with 3 months of progressive right lower extremity weakness and numbness. The patient noticed that he had been walking with a limp and was unable to urinate or ejaculate despite preserved erection. On neurological examination, he had decreased strength in the right hip flexion (4/5), knee extension (4/5), foot dorsiflexion (3/5), extensor hallucis longus (2/5), and plantar flexion (2/5). He also reported decreased sensation in the right lower extremity in nondermatomal distribution.
Imaging
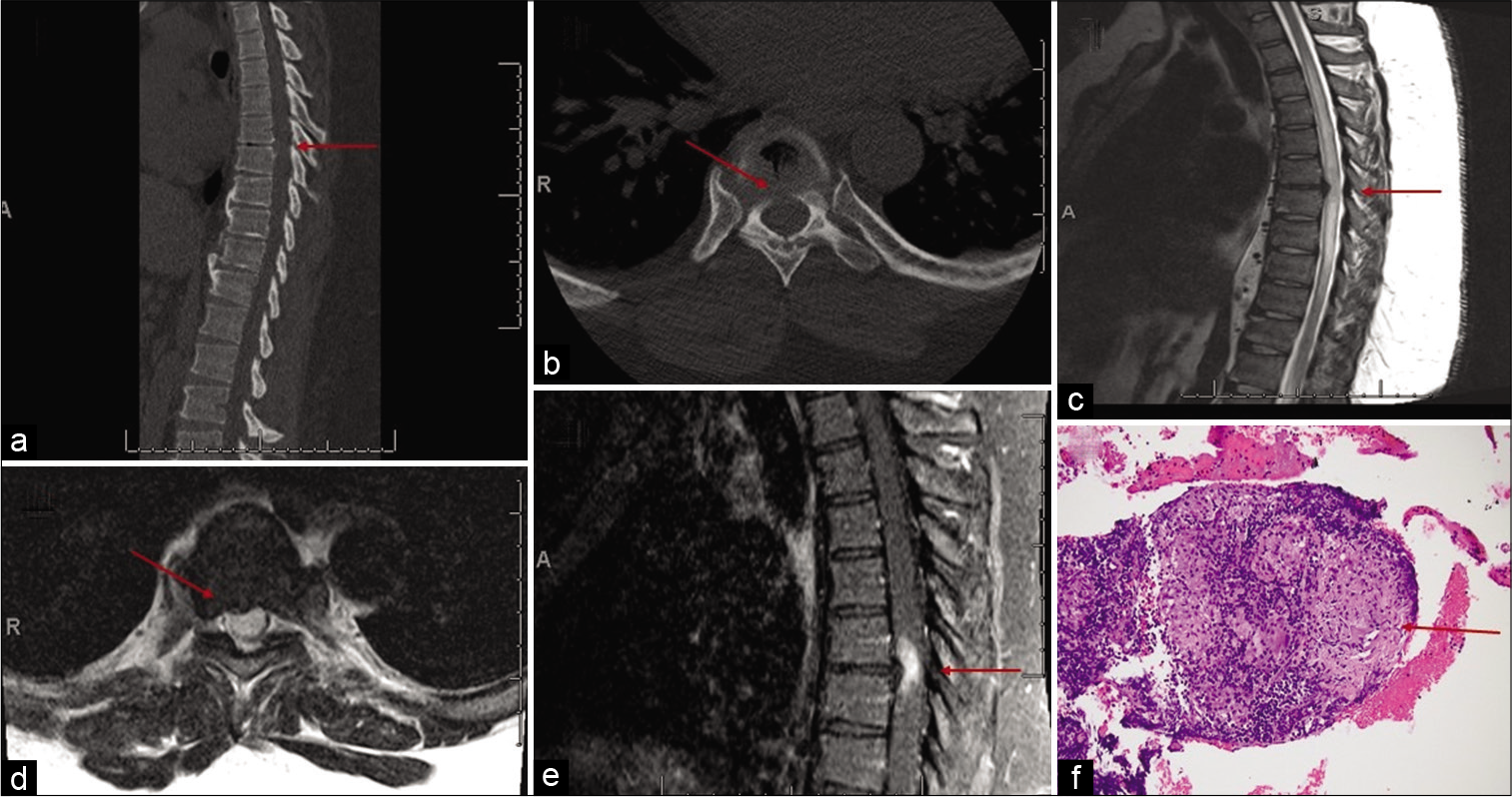
Computed tomography (CT) imaging of the spine revealed a calcified T6-T7 paracentral disc eccentric to the right [
Figure 1:
Sagittal (a) and axial (b) computed tomography scan of the thoracic spine showing a calcified T6-T7 paracentral disc eccentric to the right. Sagittal (c) and axial (d) T2-weighted magnetic resonance imaging (MRI) demonstrating the T6-T7 paracentral disc with T2 signal change extending from the T2 to T10 levels. Sagittal T1-weighted MRI with gadolinium (e) demonstrating enhancement around the T6-T7 disc bulge. Histopathological examination demonstrated noncaseating granulomas consistent with the diagnosis of sarcoidosis (f).
Histopathologic findings
The patient was started on high-dose dexamethasone. The patient noticed significant improvement in his strength over the subsequent 3 days. Given the extent of T2 signal change and contrast enhancement in the spinal cord and response to steroids, the suspicion for another primary etiology was investigated. CT chest revealed diffuse mediastinal lymphadenopathy. Angiotensin-converting enzyme level was within normal limits. He underwent an ultrasound-guided endobronchial biopsy of the enlarged lymph nodes. Histopathological examination demonstrated noncaseating granulomas consistent with a diagnosis of sarcoidosis [
Treatment and follow-up
The patient received 3 days of high-dose methylprednisolone therapy followed by prednisone (40 mg twice a day) at the time of discharge along with methotrexate and infliximab infusion. His right lower extremity returned to nearly full strength, with only mild weakness in the right extensor halluces longus and plantar flexion (4+/5) at his last follow-up visit.
DISCUSSION
Neurosarcoidosis can occur anywhere along the neuroaxis but most commonly affects the meninges of the skull base. The occurrence of spinal neurosarcoidosis is uncommon, with the cervical spine being the most common location followed by the thoracic spine.[
Spinal neurosarcoidosis is associated with a spectrum of clinical manifestations that could be nonspecific. Common presentations include cranial nerve palsy (31–55%), chronic aseptic meningitis (16–37%), spinal cord disease/myelitis, cerebral parenchymal disease (21%), neuroendocrine involvement (6–9%), hydrocephalus (9–10%), cerebral infarction (6%), and peripheral nervous system symptoms such as polyneuropathy (17%).[
Diagnostic workup of neurosarcoidosis involves imaging, serum and cerebrospinal fluid (CSF) analysis, and biopsy of enlarged lymph nodes. Imaging findings in spinal neurosarcoidosis can also be found in other conditions. Contrast enhancement on MR imaging provides evidence of breakdown of the blood–brain barrier, which has been reported as a highly sensitive marker of neuroinflammation.[
A thorough diagnostic workup is critical to providing the appropriate treatment therapy in this patient. Furthermore, establishment of a diagnosis of spinal neurosarcoidosis prevented this patient from undergoing an unnecessary surgery for his T6-7 paracentral disc. This is important as neurological surgical procedures are not without risk; the overall morbidity following surgery to correct a thoracic disc herniation is reported as high as 29% (medical 21%, surgical site 11%, CSF related 8%, and neurologic complications 5%).[
Timely and appropriate treatment of neurosarcoidosis is essential to achieve reversal of symptoms and to prevent progression of disease. Specific treatment of spinal neurosarcoidosis is not well described in the literature and is adapted from general management of multiorgan sarcoidosis. The goal is to treat the underlying inflammatory process and to reverse the symptomatic effects of the neuroinflammation. Initial therapy often starts with oral steroids, or an intravenous equivalent may be used for severe disease.[
CONCLUSION
We present a rare case of concomitant compressive thoracic disc and spinal neurosarcoidosis in a patient presenting with leg weakness. While a thoracic disc on spinal imaging may potentially suggest a mechanical etiology for the patient’s symptoms, careful attention must be paid to radiographic characteristics, specifically the extent of spinal cord signal change and intramedullary enhancement. This report highlights the importance of a complete diagnostic workup to identify the underlying etiology and provide the appropriate therapeutic intervention. Due to its variable presentation, spinal neurosarcoidosis should remain a differential diagnosis in patients presenting with progressive weakness.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Absinta M, Cortese IC, Vuolo L, Nair G, de Alwis MP, Ohayon J. Leptomeningeal gadolinium enhancement across the spectrum of chronic neuroinflammatory diseases. Neurology. 2017. 88: 1439-44
2. Aubart FC, Bouvry D, Galanaud D, Dehais C, Mathey G, Psimaras D. Long-term outcomes of refractory neurosarcoidosis treated with infliximab. J Neurol. 2017. 264: 891-7
3. Brotis AG, Tasiou A, Paterakis K, Tzerefos C, Fountas KN. Complications associated with surgery for thoracic disc herniation: A systematic review and network meta-analysis. World Neurosurg. 2019. 132: 334-42
4. Deng P, Krasnozhen-Ratush O, William C, Howard J. Concurrent LETM and nerve root enhancement in spinal neurosarcoid: A case series. Mult Scler. 2018. 24: 1913-6
5. Gelfand JM, Bradshaw MJ, Stern BJ, Clifford DB, Wang Y, Cho TA. Infliximab for the treatment of CNS sarcoidosis: A multi-institutional series. Neurology. 2017. 89: 2092-100
6. Ibitoye RT, Wilkins A, Scolding NJ. Neurosarcoidosis: A clinical approach to diagnosis and management. J Neurol. 2017. 264: 1023-8
7. Nozaki K, Judson MA. Neurosarcoidosis. Curr Treat Options Neurol. 2013. 15: 492-504
8. Pawate S, Moses H, Sriram S. Presentations and outcomes of neurosarcoidosis: A study of 54 cases. QJM. 2009. 102: 449-60
9. Saleh S, Saw C, Marzouk K, Sharma O. Sarcoidosis of the spinal cord: Literature review and report of eight cases. J Natl Med Assoc. 2006. 98: 965-76
10. Sohn M, Culver DA, Judson MA, Scott TF, Tavee J, Nozaki K. Spinal cord neurosarcoidosis. Am J Med Sci. 2014. 347: 195-8
11. Soni N, Bathla G, Maheshwarappa RP. Imaging findings in spinal sarcoidosis: A report of 18 cases and review of the current literature. Neuroradiol J. 2019. 32: 17-28
12. Varron L, Broussolle C, Candessanche JP, Marignier R, Rousset H, Ninet J. Spinal cord sarcoidosis: Report of seven cases. Eur J Neurol. 2009. 16: 289-96
13. Voortman M, Drent M, Baughman RP. Management of neurosarcoidosis: A clinical challenge. Curr Opin Neurol. 2019. 32: 475-83